- Visibility 313 Views
- Downloads 55 Downloads
- Permissions
- DOI 10.18231/j.ijca.2021.104
-
CrossMark
- Citation
Successful anesthetic management in a case of grade V splenic injury in covid 19 positive patient: A case report
Abstract
Splenic injuries are amongst the most frequent trauma-related injuries which requires emergency surgeries demanding meticulous surgical and anesthetic management. The aim while managing splenic trauma patients, is to restore homeostasis and normal pathophysiology in the body by achieving hemostasis with an emergency splenectomy.
To date, there have been few reports describing the anaesthetic management of COVID-19 patients presenting for emergency surgery. In this article, we outline the anaesthetic management for a case with hemoperitoneum, posted for emergency exploratory laparotomy and splenectomy in our operating theatre who was incidentally diagnosed to be COVID positive in the emergency unit by a rapid antigen test.
Case Presentation
We report a case of a 45 years old male presented to our emergency department with an alleged history of a road traffic accident and having sustained trauma to the left side of the upper abdomen and chest.
On examination, he was conscious and was responding to verbal commands. He complained of pain on the left side of his chest and abdomen. On physical examination, he had a bruise over the left side of chest and abdomen along with abdominal distension. His vitals consisted of a blood pressure of 92/60 mm of Hg (without any inotropic support), heart rate of 122 beats per minutes, respiratory rate of 20-22/ min and 95 % saturation on room air with decreased visible chest expansion on the left side. Immediately wide bore 18 gauze intravenous cannulation was done. All routine blood investigations, blood grouping and cross matching were sent. Fluid resuscitation with intravenous fluid (Ringer lactate) was started. On quick medical history taking, he was known hypertensive, on regular medication (Tablet Telmisartan 40 mg OD) and had complained of cough and fever for last 4 days.
Focussed assessment with sonography in trauma (FAST) revealed presence of free fluid in abdomen. CECT chest and abdomen was suggestive of grade V splenic laceration, left chest wall injury of lower ribs (4th to 10th), hemothorax and ground glass opacities on bilateral lung sides.
Rapid antigen test for COVID 19 was performed with the patient's nasopharyngeal swab which tested Positive.
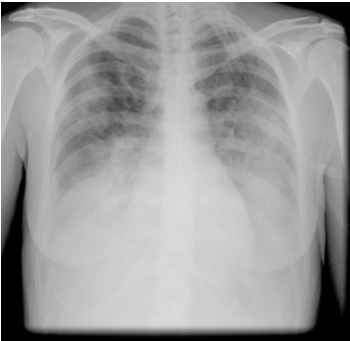
12 lead ECG showed LAD and LVH. CXR showed left side ribs fracture, hemothorax and few patchy ground glass ([Figure 1]) opacity on bilateral lung fields.
Routine blood investigations showed hemoglobin of 10 gm/dl, total leucocytes count of 16700/mm3, platelets 1.74 lacs/mm3. LFT, KFT and serum electrolytes were within normal range. Bleeding Time and Clotting Time were normal. Four units of packed cell volumes, fresh frozen plasma and platelet concentrates were arranged.
As this was grade V splenic injury, emergency exploratory laparotomy and splenectomy under general endotracheal anaesthesia was planned in compliance with tertiary protection regulations,[1] which means that all involved medical staff had to wear full personal protective equipment (PPE), including disposable N95/FFP2 respirators, double gloves, goggles, visors, caps, shoes, and body protection coveralls/gowns. After informing the emergency OT nursing and technical staff, patient was shifted to emergency OT with ongoing fluid resuscitation. After wearing adequate personal protective equipment, the patient was received in OT. Quick examination, surgical checklist, written and informed high risk consent in view of major emergency surgery in a Covid-19 positive case with anticipated blood loss and massive blood transfusion, postoperative ventilation and ICU admission was taken and confirmed.
All routine and emergency drugs, anesthesia work-station, defibrillator, difficult airway cart, video-laryngoscopes, direct layngoscopes with incremental size blades, intubation box, ET tube with inline suctioning was checked and kept ready.
All standard ASA monitors were attached. Another 18G intravenous cannula was secured. Modified rapid sequence induction was planned. Intubation box was placed at the head end.
After preoxygenation with 100% oxygen for 3 minutes, patient was induced with Injection fentanyl, Thiopentone sodium and Succinylcholine. Trachea was secured with 8.5 no. portex cuffed endotracheal tube with inline suction device and confirmed with bilateral chest rise and persistent capnogram. Patient was ventilated to maintain end tidal CO2 within 35-45 mm of Hg with following ventilatory settings: tidal volume - 6 ml/kg, respiratory rate -16 to 18 per minute, PEEP -5. Anesthesia was maintained with oxygen: nitrous oxide (50:50), Isoflurane, Inj. Morphine and intermittent boluses of Inj. vecuronium.
There was mild hypotension following induction which was managed with crystalloids.
Immediately after induction, left sided ICD was placed which drained approximately 150 ml of hemothorax.
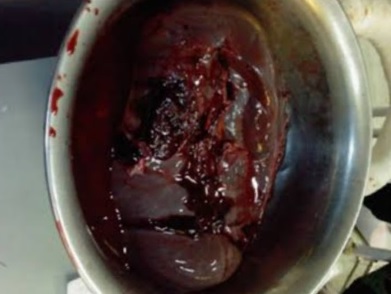
Exploratory laparotomy was commenced and 3.5 litres of hemoperitoneum was drained, lacerated spleen was dissected out by meticulous ligation of splenic vessels ([Figure 2]). Suction devices were intensively used to remove the body fluid and smoke to prevent airborne and aerosol viral transmission. Hypothermia was avoided by infusing warm intravenous fluids, warm blood and by wrapping the patient’s extremities with cotton. Total per-operative blood loss was approximately 4.5 litres.
There were few episodes of hypotension which were successfully managed by low dose of noradrenaline infusion which was tapered according to response and crystalloids to maintain mean arterial blood pressure above 65 mm of Hg.
Patient received 2 units of FFP, 2 units of platelet concentrates, 2 unit of packed cells after clamping of splenic vessels. Apart from blood products he was infused 2 litres of crystalloids, 1 litre colloid (hydroxyethyl starch) and his urine output at end of surgery was 700 ml (approximately 175 ml/hour). He was given 1 ampule of Inj. Calcium Gluonate (10 ml / 950mg /2.2 mmol) and 10 mg furosemide. Surgery lasted for 4 hours. At the end of the surgery, incision line and ICD port site were infiltrated with 0.25% bupivacaine. Intra-op ABG revealed mild metabolic acidosis (pH- 7.28, pO2-125, pCO2- 43.5, HCO3-19.4, Hct- 30.4%, BE: -6). In view of massive blood loss and metabolic acidosis, the patient was planned to be electively ventilated.
At the end of surgery, the patient was shifted to Covid-19 Intensive care unit for post- operative ventilation (ARDS lung protective ventilatory setting). In the post-operattive period further 2 units of packed cells, 2 units of FFP were transfused. After 12 hours of blood replenishment, good breathing efforts and acceptable ABG patient was successfully extubated and was maintaining saturation of 99 percent with non- rebreathing mask at 10 litres /min oxygen flow. Pain was managed with intravenous tramadol, paracetamol and diclofenac sodium. Injection Clexane 40 mg (0.4 ml) subcutaneously OD was started along with antibiotics in view prothrombotic condition in covid 19 and massive blood transfusion.
Patient was vaccinated with pneumococcal, meningococcal and H- influenza type B vaccines and had ICU stay for 5 days. His inflammatory markers were d-dimer of 850, IL-6 of 49 and serum ferritin of 106. He was put on HFNC (High flow nasal cannula) on 50% fiO2 at 50 litres /minute flow intermittently on day 3 and 4. Later, his oxygen requirement was reduced and inflammatory markers improved. Later, on day 6 he was shifted to ward. On repeat RTPCR test, patient tested negative for covid 19 on 10th post-operative day and then was discharged from hospital after 17 days of hospitalization.
Discussion
At present, COVID-19 has made a significant impact on almost all countries in the world, majorly in India. However, there have been no reported cases of Grade V splenic injury with Severe Acute Respiratory Syndrome (COVID 19) infection undergoing emergency surgery. Few case reports of spontaneous atraumatic splenic rupture in covid 19 patients have been reported.[2]
Coronaviruses are a large family of viruses and the subset of Coronaviridae, ranging from the common cold virus to more serious diseases such as SARS, MERS, and COVID–19. Depending on the type of coronavirus, the symptoms can range from common cold symptoms to fever, cough, shortness of breath, and acute respiratory problems. In severe cases it is seen to be associated with coagulopathies.
As there is extreme rise in the number of cases of covid 19 patients, it is inevitable that some patients with COVID-19 will require elective as well as emergency surgeries.
Splenic injuries are among the most frequent trauma-related injuries requiring emergency laparotomy. The management of splenic trauma must be multidisciplinary and should focus on physiological and anatomical derangement together with the immunological effects.
Based on our experience and available literature, following are perspectives and precautions regarding clinical and anesthetic management of emergency surgical procedures on COVID 19 positive patients. As indications for emergency surgery in COVID-19 pandemic are almost same as before in regular patients, there are difficulties in the decision-making regarding the differential diagnosis of COVID-19 from other types of pneumonia like presentations before surgery. However, our primary concern should be timely intervention of these urgent cases along with the protection of all medical staff.
As in our hospital, COVID emergency OT should be negative-pressure theatre or else air exchange cycles should be increased whenever possible to ≥ 25 exchanges/hour[3] and should be out of heavy-traffic zones. There should be the development of specific patient transfer pathways for patient’s transit to and from OT, labelled as Red Zone with nearby isolated recovery rooms (post-operative areas), ICUs or medical wards.For inter-hospital patient transfer or transfer from other buildings within the hospital, a dedicated vehicle should be used. Transfer personnel should be specifically trained and equipped with PPEs.[4]
Whole medical team involved in surgery should be equipped with full PPE as described above. The number of surgical, nursing and anesthetist team members working in the OT should be limited to the minimum required to perform the surgery.
Anesthetic considerations:[3]
Meticulous anesthetic planning is required to minimize any infection potentially associated with unexpected complex endotracheal intubation procedures. Disposable airway equipment should be preferred. Intubations techniques with the highest chance of first-time success should be preferred to avoid repeated airway instrumentation. Awake intubation including fibreoptic techniques should be avoided.[3] Rapid sequence intubation (RSI) should be considered to avoid manual ventilation and potential aerosolization. A closed suction system should be preferred during airway aspiration. HEPA (high-efficiency particulate air) filter should be connected to the patient end of the breathing circuit and another one between the expiratory limb and the anesthetic machine. Both HEPA filters and soda lime must be changed after each case. Regarding ventilatory settings, ARDS lung-protective ventilation guidelines should be followed[5] : (1) a tidal volume less than or equal to 6 ml/kg predicted body weight; (2) a respiratory rate less than or equal to 35 breaths/min; (3) a plateau airway pressure less than or equal to 30 cm H2O; and (4) a positive end-expiratory pressure (PEEP) greater than or equal to 5 cm H2O6.
In trauma emergency surgeries as we came across, there is risk of massive blood loss which requires early damage control resuscitation including massive blood transfusion. Our patient had blood loss of 4.5 litres which was replenished by 4 units of packed cell volumes, 4 units of FFP and 4 units of platelets in 24 hours. Our concern in such scenario was whether massive blood transfusion would have any adverse effects on outcome of the patient as he was infected with covid 19 which is known to cause exaggerated inflammatory response due to cytokine storm and formation of microemboli.[6] The virus is also known to attack red blood cells, thus decreasing the oxygen-carrying capacity.[7] Iron released from lysed red blood cells is also implicated in endothelial inflammation induced by viral infections through induction of reactive oxygen species leading to nuclear factor kB (NF-kB) activation and subsequent upregulation of proinflammatory mediators such as IL-1β, IL-6 and TNF-α.[8] Understanding of this pathophysiology has led some clinicians to use packed cell volume[9] and iron chelating agents like dexferrioxamine[10] for COVID-19 treatment, as it can increase oxygen-carrying capacity and decreases reactive oxygen species and hence might prevent the patient from going into a hypoxic state. As our patient showed clinical improvement after surgery and blood transfusion and was extubated next day, we might assume that blood transfusion could have increased oxygen carrying capacity and helped in early recovery. Although thromboembolic risks are increased in massive blood transfusions, damage control resuscitation in form of 1:1:1 may help in reducing these risks.[11] In view of prothrombogenesis as seen and documented in covid 19 patients, use of anticoagulants is helpful.[12] Our patient was started in Injection Clexane 40 mg (0.4 ml) once a day subcutaneously from postoperative day 1.
Regarding surgical practices, all techniques which might generate aerosols should be minimized (electrocautery or ultrasonic scalpels). Separate suction machines, one for anesthesia provider and other for surgical site should be used so that there is minimal unnecessary disconnection.
Compared with regular post-operative patients, COVID-19 patients need more intensive postoperative care due to their lung conditions, their comorbidities need extra attention, duration of hospital stay is usually prolonged. It has been observed that mortality rate for patients with COVID-19 with several comorbidities is higher than for those without comorbidities.[13]
Conclusion
We could successfully manage a Covid 19 positive patient with grade V splenic injury in shock for emergency laparotomy and splenectomy under general endotracheal anesthesia by following proper protocols and using adequate protective equipments. We recommend use of proper guidelines and protocols so as to provide timely medical and surgical care to covid positive trauma patients and at the same time maintaining adequate safety of medical staff. Use of massive blood transfusion protocol and good post operative intensive care can help in improving prognosis of these patients.
Abbreviations
mm of Hg - milimetres of mercury; %- percentage; OD- once a day; ECG –Electrocardiogram; LAD - Left axis deviation; LVH- Left ventricular hypertrophy; CXR - chest x-ray; gm/dl – grams per deciliters; mm3 – cubic mililitres; N95 – Non- oil 95; FFP2 – filtering face piece; OT – operation theatre; ET – endotracheal tube; ASA – American society of anesthesiologists; 18G – 18 guaze; CO2 – carbon dioxide; Inj – Injection; ICD – Intercostal drain; FFP – Fresh frozen plasma; ml – mililitres; pH – potential of hydrogen; pCO2 – partial pressure of carbon dioxide; pO2 – partial pressure of oxygen; HCO3- - bicarbonate; Hct – hematocrit; BE – base excess; ABGA – arterial blood gas analysis; IL 6 – interleukin 6; HFNC – high flow nasal cannula; fiO2 – fraction of inspired oxygen; RTPCR – reverse transcriptase polychromatic chain reaction; SARS – severe acute respiratory syndrome; MERS – middle east respiratory syndrome; PPE – personal protective equipments; HEPA – high efficiency particulate air filter; NF-kB – nuclear factor kappa beta; TNF -α – tumour necrosis factor alpha; CECT – contrast enhanced computerized tomography.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- Meng L, Wan H, Ai Y, Xue Z, Guo Q, Deshpande R. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan's Experience. Anesthesiology. 2020;132:1317-32. [Google Scholar]
- . National Health Commission of the People's Republic of China. Diagnosis and treatment of novel coronavirus pneumonia (7th version). . . [Google Scholar]
- Mobayen M, Yousefi S, Mousavi M, AA. The presentation of spontaneous splenic rupture in a COVID-19 patient: a case report. BMC Surg. 2020. [Google Scholar] [Crossref]
- Ti L, Ang L, Foong T, BN. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020;67(6):756-8. [Google Scholar] [Crossref]
- Coccolini F, Perrone G, Chiarugi M, Marzo F, Ansaloni L, Scandroglio I. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15. [Google Scholar] [Crossref]
- Mehta P, Mcauley D, Brown M, Sanchez E, Tattersall R, Manson J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033-4. [Google Scholar]
- Wenzhong L, Hualan L. COVID-19:Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism. ChemRxiv. 2020. [Google Scholar] [Crossref]
- Visseren F, Verkerk M, Bruggen T, Marx J, Asbeck BV, Diepersloot R. Iron chelation and hydroxyl radical scavenging reduce the inflammatory response of endothelial cells after infection with Chlamydia pneumoniae or influenza A. Eur J Clin Invest. 2002;32:84-90. [Google Scholar]
- Ejigu T, Patel N, Sharma A, Vanjarapu J, Nookala V. Packed Red Blood Cell Transfusion as a Potential Treatment Option in COVID-19 Patients With Hypoxemic Respiratory Failure: A Case Report. Cureus. 2020;12(6). [Google Scholar] [Crossref]
- Dalamaga M, Karampela I, Mantzoros C. Commentary: Could iron chelators prove to be useful as an adjunct to COVID-19 Treatment Regimens?. Metabolism. 2020;108. [Google Scholar] [Crossref]
- Holcomb J, Tilley B, Baraniuk S, Fox E, Wade C, Podbielski J. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471-82. [Google Scholar] [Crossref]
- Ahmed S, Zimba O, Gasparyan A. Thrombosis in Coronavirus disease 2019 (COVID-19) through the prism of Virchow’s triad. Clin Rheumatol. 2020;39:2529-43. [Google Scholar]
- Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-62. [Google Scholar]
How to Cite This Article
Vancouver
Kumari A, Husain F, Sethi A, Saxena KN. Successful anesthetic management in a case of grade V splenic injury in covid 19 positive patient: A case report [Internet]. Indian J Clin Anaesth. 2021 [cited 2025 Oct 30];8(4):49-53. Available from: https://doi.org/10.18231/j.ijca.2021.104
APA
Kumari, A., Husain, F., Sethi, A., Saxena, K. N. (2021). Successful anesthetic management in a case of grade V splenic injury in covid 19 positive patient: A case report. Indian J Clin Anaesth, 8(4), 49-53. https://doi.org/10.18231/j.ijca.2021.104
MLA
Kumari, Anupama, Husain, Farah, Sethi, Anjili, Saxena, Kirti Nath. "Successful anesthetic management in a case of grade V splenic injury in covid 19 positive patient: A case report." Indian J Clin Anaesth, vol. 8, no. 4, 2021, pp. 49-53. https://doi.org/10.18231/j.ijca.2021.104
Chicago
Kumari, A., Husain, F., Sethi, A., Saxena, K. N.. "Successful anesthetic management in a case of grade V splenic injury in covid 19 positive patient: A case report." Indian J Clin Anaesth 8, no. 4 (2021): 49-53. https://doi.org/10.18231/j.ijca.2021.104
