- Visibility 159 Views
- Downloads 18 Downloads
- DOI 10.18231/j.ijca.2025.010
-
CrossMark
- Citation
A comparative study of triamcinolone injection alone versus combined triamcinolone injection with pulsed radiofrequency for frozen shoulder pain: A randomized controlled study
Introduction
Frozen shoulder (FS), or adhesive capsulitis, is a progressively restrictive painful shoulder condition characterized by a gradual onset of pain, stiffness, and limited mobility in the shoulder joint.[1] Individuals with frozen shoulder experience discomfort, particularly when attempting to move the shoulder, and may find it challenging to perform daily activities that involve shoulder movement. The exact cause is often unclear, but it is associated with inflammation and the formation of adhesions within the shoulder joint capsule. The incidence is approximately 3-5% in the general population, whereas in diabetes mellitusit is 10%-20%.[2] Peak incidence is seen between 40 and 60 years of age.[3] Treatment varies depending on the individual's symptoms and stage and may include physical therapy, medications, and, in some cases, medical interventions. Among the different modalities of treatment available, minimally invasive treatments of FS include suprascapular nerve (SSN) interventions with steroids and local anesthetic agents, as well as pulsed radiofrequency (PRF) treatment.[4], [5], [6] "We hypothesized that combining the two modalities would result in more prolonged pain relief, as measured by the Visual Analog Scale (VAS), along with better efficacy in terms of Shoulder Pain and Disability Index (SPADI) scores, and improved range of motion (ROM) assessed through goniometry. A comparative study was conducted to compare triamcinolone alone versus triamcinolone combined with pulsed radiofrequency (PRF) of the suprascapular nerve in patients with frozen shoulder."
Materials and Methods
A prospective randomized controlled clinical trialwas conducted in the Pain Medicine outpatient department (OPD) in the department of Anaesthesiology and Pain Medicine from July 2019 to December 2020. After obtaining ethical clearance from the institutional ethical committee (IEC no. 59/18) and registration of study with the clinical trial registry, India (CTRI/2019/07/020233), patients of frozen shoulder who attended the Pain Medicine outpatient department (OPD), were assessed for possible recruitment in the study (consort flow chart).
The sample size was determined based on a previous study that measured the reduction in SPADI disability, using the following formula:[7]
n = Zα/2+ Zβ 2 ×Zσ2d2
where:
Zα/2 @ 95% C.I = 1.96
Zß @ 80% power = 0.84
σ (pooled S.D) = 5
d (difference in mean) = 8
To account for potential dropouts during follow-up, we recruited 21 participants for each group.

Study tools
The VAS is a subjective pain assessment tool used to quantify a patient's pain intensity consisting of a 10-centimeter straight line, ranging from "no pain" to "worst imaginable pain." The higher the score, the greater the perceived pain intensity, making VAS a valuable tool in pain assessment.[8] The Shoulder Pain and Disability Index score SPADI score is an easy, reliable set of questions that evaluate pain and functional activities: five questions for pain dimension and eight questions for activities of daily living to access functional activities of the upper extremity.[9] A goniometer was used to assess the range of motion among participants.
Patient selection, randomization, and group allocation
All patients included in the study had undergone at least six months of failed conservative care, including analgesics such as non-steroidal anti-inflammatory drugs (NSAIDs) and topical analgesics, skeletal muscle relaxants along with physiotherapy and occupational therapy including hot fomentation, transcutaneous electrical nerve stimulation (TENS), and diathermy application. After obtaining informed consent, Forty-one patients suffering from FS of either sex or age between 18-80years were considered in the study. Twenty-one patients were allocated to the Triamcinolone group (T), and 20 were allocated to the Triamcinolone and PRF combined (C). They were thoroughly examined to rule out cervical spine pathologies such as cervical facet syndrome and cervical radiculopathy, which may also present with shoulder pain. The patients with chronic obstructive pulmonary disease (COPD),known allergies to drugs, pregnant patients, and coagulopathy were excluded from the study.
A person not participating in the study assigned the participants to the groups. The participants were recruited using a computer-generated block randomization technique with fixed block sizes of four. A concealed allocation method using sealed and opaque envelopes was used to allocate patients to the two groups.
Intervention and outcome measures
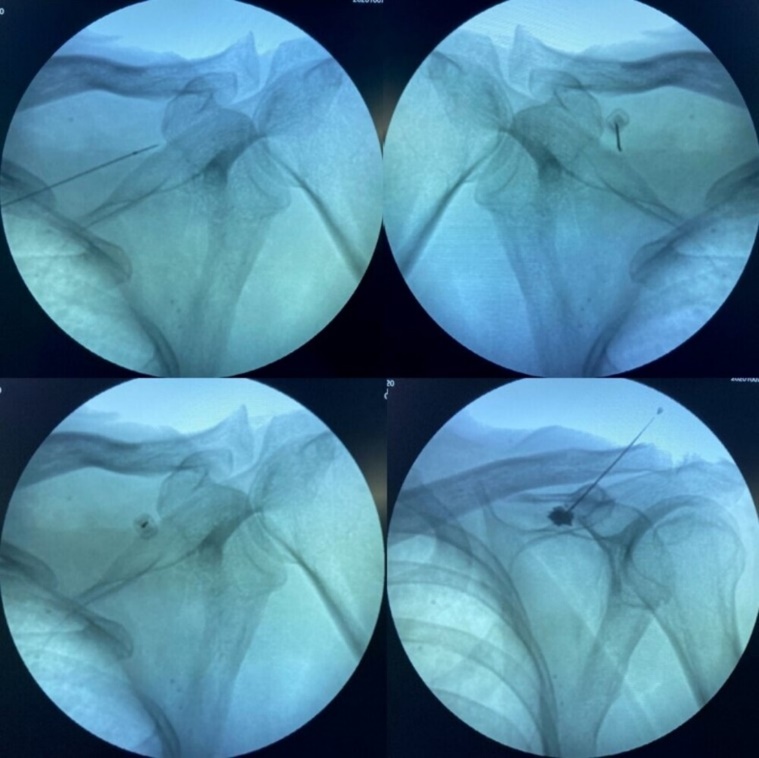
The procedures were performed under standard American Society of Anesthesiologists (ASA) monitoring under monitored anesthesia care (MAC). Intravenous access was obtained before beginning the procedure. Patients were conscious of responding to stimulation tests. Group-T patients who underwent SSN intervention with injection triamcinolone 40mg + Inj. Bupivacaine is 0.25%, with a total volume of 8 ml. Group-C Patients underwent SSN intervention with Injection triamcinolone 40mg + Inj. Bupivacaine is 0.25%, with a total volume of 8 ml. and PRF treatment. Pulsed radio frequency was performed at 50V with pulse delivered at every 20ms for 10 min with a maximum tip temperature of 42degree centigrade, using RF pain management generator (Kimberly Clark Inc.Worldwide, US) ([Figure 2]). A thorough preoperative check-up was done for all patients beforethe procedure, including a complete blood count and coagulation profile.
Data collection and statistical analysis
The data were entered into a Microsoft Excel sheet and coded. Statistical analysis was done using the software "Statistical Package for the Social Sciences" SPSS version 22. All qualitative data were presented as proportions (number and percentage), and continuous data were presented as mean ± SD. The chi-square test was used to ascertain the association between categorical variables. The mean ± SD of VAS and SPADI between the two groups were analyzed by unpaired t-test. The value of p<0.05 was considered statistically significant at 95% CI.
Results
The present study was conducted in department of anaesthesia in pain medicine unit. Total forty five patients were treated and forty one patients were enrolled for study, twenty-one patients in Triamcinolone group (Group T), and twenty-one patients in combined Triamcinolone and PRF group (Group C). Three patients did not complete follow-up until six months, so each Group had 19 patients at the end of the trial. Bothgroups were comparable in terms of demographic and clinical profile.
The mean age of the participants in Group T was 54.28±9.25, and in Group C, it was 52.75±9.39, with a statistically non-significant difference in age (p-value=0.998). Gender distribution and mean duration of symptoms between the two groups were also comparable (p> 0.05). The maximum duration of symptoms in Group T was 18 months; in the combinedGroup C, it was 24 months ([Table 1]).
|
Demographic and clinical Profile |
Group T |
Group C |
p-value |
|
|
Mean Age (Mean ±SD) |
|
54.28± 9.25 |
52.75± 9.39 |
0.99 |
|
Gender |
Male |
10 (47.6%) |
9 (45%) |
0.86 |
|
Female |
11 (52.4%) |
11 (55%) |
||
|
Mean Duration of Pain (months) (Mean ±SD) |
|
8.52± 3.26 |
7.6±3.72 |
0.40 |
|
Comorbidities |
None |
3 (14.3%) |
3 (15%) |
0.99 |
|
Diabetes Mellitus |
9 (42.9%) |
9 (45%) |
||
|
Hypertension |
5 (23.8%) |
4 (20%) |
||
|
Multiple |
4 (19%) |
4 (20%) |
VAS scores of Group T and C (8.14±0.65 and 8.35±0.67, respectively; p= 0.213) were statistically non-significant before intervention. The reduction in mean VAS score after intervention was found to be more in group C than in group T with a statistically significant difference at each interval (p-value<0.05) as shown in ([Figure 3]).

The pre-intervention SPADI total scores in group T (64.11±7.31) and group C (64.9±5.32) were comparable (p=0.064). There was statistically significant improvement inboth Groups post-intervention, but it was more in Group C compared to Group T (p-value<0.05), as shown in ([Figure 4]).

A comparative analysis between the two groups shows statistically non-significant differences in pre-intervention ROM in flexion (p=0.113), extension (p=0.234), and abduction (p=0.173). A statistically significant difference was found between both groups at each follow-up in all ranges of motion ([Figure 5]).

Discussion
Frozen shoulder (FS) is a condition characterized by stiffness and pain in the shoulder joint, affecting a person's daily activities. Conservative treatment and physiotherapy are the mainstay of treatment, but due to excessive pain and stiffness, it isn't easy to do effective physiotherapy. The minimally invasive intervention of the Suprascapular nerve may help the patients to eliminate the pain. Suprascapular nerve minimally invasive pain and spine intervention (SSN MIPSI) using local anaesthetics and steroids is a safe and well‑tolerated treatment option for the treatment of frozen shoulder.
It is effective in reducing severity of pain and functional disability, hence improves quality of life of the patients with FS.[10] The suprascapular nerve (SSN) originates from the upper trunk of the brachial plexus (C5–C6), and it innervates approximately 70% of the superior and posterior regions of the shoulder joint, capsule, and acromioclavicular joint. This nerve also supplies motor innervation to the supra- and infraspinatus muscles. An SSN MIPSI with steroid and local anesthetic can effectively relieve the pain and increase the ROM in patients with long histories of shoulder pain including FS, rotator cuff injuries, osteoarthritis, and rheumatoid arthritis.[11] However, the effects of suprascapular nerve intervention using steroids are short-lived;which requires search of more treatment modalities. The recent use of radiofrequency in pain medicine add promising result in resistant frozen shoulder patient.
Pulsed mode radiofrequency (PRF) lesioning of suprascapular nerve is a non-neuroablative i.e., neuro-modulatory method which can alleviate chronic pain without evidence of neural damage by delivering an electrical field and heat bursts (temperature of <42°C, in contrast to conventional radiofrequency applications, which deliver a constant temperature of 60°C–80°C). Some preliminary reports support its long-term efficacy in pain relief.[12] Several case studies have reported a favourable outcome for pulsed radiofrequency (PRF) neuromodulation to the suprascapular nerve (SSN) in treating FS and it facilitated functional recovery without risking paralysis of the supraspinatus or infraspinatus muscles.[13] In our study, we prospectively compared the effects of suprascapular nerve intervention using triamcinolone injection alone versus a combination of triamcinolone with PRF in patients with frozen shoulder. We anticipated immediate relief from the local anesthetic (LA) and triamcinolone, alongside sustained benefits from the neuro-modulatory effects of PRF.
On comparison of demographic data, the mean age of participants in the Triamcinolone group (Group T) was 54.28±9.25 years, while in the combined group was 52.75±9.39 years, with the participants' ages ranging from 37 to 75 years. There were 19 (46.4%) men and 22 (53.6%) women. Our findings are similar to those of Kiera Kingston et al. who, in their epidemiological study, found the mean age 56.4±13.1years, with most patients’ ages ranging from 40 to 70 years.[14] They also reported that frozen shoulders affect females (58.4%) more than males.[13] The most common comorbidity associated with frozen shoulder was diabetes mellitus (DM) in 24 (58.53%) patients followed by hypertension in 12 (29.26%) patients. Our findings are similar to Connie B. Tighe et al in their study that the prevalence of DM in patients with frozen shoulder was found to be 38.6% (34 of 88) and in prediabetes was found to be 32.95% (29 of 88) with total prevalence of 71.5% (63 of 88). Similar results were observed by Kiera Kingston et al who in their epidemiological study found that diabetes mellitus (55.3%) and hypertension (33.5%) were the most common medical comorbidities.[2], [14]
The VAS score in the Triamcinolone and combined groups reduced significantly at every follow-up, but more pronounced pain relief was evident in the combined group. Our results are comparable to those of Teja et al, who used an injection of bupivacaine and methylprednisolone acetate for suprascapular nerve block in their randomized controlled trial and found a significant reduction in painat the end of three months, and Jang et al, who found effective pain relief with pulsed radiofrequency neuromodulation in 11 patients with chronic shoulder pain.[15], [16]
In our study, SPADI scores were reduced significantly in both groups at six months compared to pre-intervention values. However, it was more pronounced in the combined Group than in the triamcinolone group(p = 0.019). Our results were consistent with the prospective randomized control trial studies conducted by Yung Tsan Wu and Davinder et al. showing a significant (p<0.001) reduction in SPADI score at various follow-up intervals compared to baseline. [17], [18]
There was a significant improvement in ROM in all axis, with a more pronounced effect in the combined Group than in the Triamcinolone group. Our findings are in coherence with Davinder et al.Shanahan et al. found significant (p<0.05) improvement in the ROM in the abduction and external rotation post-intervention up to three months.[19], [20] In contrast, we followed up until six months frozen shoulder patients.
Wu et al. and Sinha et al. in their prospective studies used standard parameters of PRF treatment (2 Hz, 30-ms pulse width, 42°C with 120-180 seconds duration) and found significant relief in both pain and ROM while we used fixed and high voltage PRF for an extended duration (10 minutes), and increasing output voltage giving better and extended pain relief as recommended by previous studies showing better outcomes with PRF treatment.[12], [17], [20], [21]
Limitations
A key limitation of this study is the relatively short follow-up period, as frozen shoulder often exhibits a chronic and recurrent nature, with symptoms that can persist long-term. To better understand the efficacy and sustainability of the treatments, future studies should incorporate larger sample sizes, extended follow-up durations, and robust methodologies such as double-blinded, placebo-controlled designs. This approach will help validate the findings and provide more comprehensive insights into treatment outcomes
Conclusion
This study demonstrates that adding pulsed radiofrequency to triamcinolone steroid injections can extend the duration of pain relief provided by suprascapular nerve intervention in managing frozen shoulder patients who have not responded to conservative treatment.The combined approach had sustained pain relief, improved range of motion, and improved functional outcome.While the results are promising, the study's limitations should be considered, and further research is warranted to confirm these findings and assess the long-term outcomes of these interventions.
List of Abbreviations
ASA: American Society of Anesthesiologists; CI: Confidence Interval; CTRI: Clinical Trial Registry of India; COPD: Chronic Obstructive Pulmonary Disease; FS: Frozen Shoulder; LA: Local anesthetics; MAC; Monitored Anesthesia Care; NSAIDS: Non-Steroidal Anti-Inflammatory Drugs; OPD: Outpatient Department; PRF: Pulsed Radiofrequency; ROM: range of Motion: SPADI: Shoulder Pain and Disability Index; SSN: Supra-Scapular Nerve; TENS: Transcutaneous Electrical Nerve Stimulation; VAS: Visual AnalogScale.
Sources of Funding
None.
Conflict of Interest
None.
References
- DDL Serna, S Navarro-Ledesma, F Alayón, E López, L Pruimboom. A comprehensive view of frozen shoulder: a mystery syndrome. Front Med (Lausanne) 2021. [Google Scholar]
- CB Tighe, WS Oakley. The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. South Med J 2008. [Google Scholar]
- CM Robinson, KM Seah, YH Chee, P Hindle, IR Murray. Frozen shoulder. J Bone Joint Surg Br 2012. [Google Scholar]
- JC Winters, JS Sobel, KH Groenier, HJ Arendzen, B Meyboom-de Jong. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomised, single blind study. BMJ 1997. [Google Scholar]
- M Ranalletta, LA Rossi, SL Bongiovanni, I Tanoira, CM Elizondo, GD Maignon. Corticosteroid injections accelerate pain relief and recovery of function compared with oral NSAIDs in patients with adhesive capsulitis: A Randomized controlled trial. Am J Sports Med 2016. [Google Scholar]
- A Agarwal, S Rastogi, S Rai, M Giri, S Parashar, D Malviya. Effect of minimally invasive pain intervention in frozen shoulder patients: A cross-sectional study. Anesth Essays Res 2020. [Google Scholar]
- J Charan, T Biswas. How to calculate sample size for different study designs in medical research?. Indian J Psychol Med 2013. [Google Scholar]
- IS Thong, M P Jensen, J Miró, G Tan. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure?. Scand J Pain 2018. [Google Scholar]
- KE Roach, E Budiman-Mak, N Songsiridej, Y Lertratanakul. Development of a shoulder pain and disability index. Arthritis Care Res 1991. [Google Scholar]
- Z Klç, MB Filiz, T Çakr, NF Toraman. Addition of suprascapular nerve block to a physical therapy program produces an extra benefit to adhesive capsulitis: A Randomized controlled trial. Am J Phys Med Rehabil 2015. [Google Scholar]
- GK Karataş, J Meray. Suprascapular nerve block for pain relief in adhesive capsulitis: comparison of 2 different techniques. Arch Phys Med Rehabil 2002. [Google Scholar]
- PC Liliang, K Lu, CL Liang, YD Tsai, CH Hsieh, HJ Chen. Pulsed radiofrequency lesioning of the suprascapular nerve for chronic shoulder pain: a preliminary report. Pain Med 2009. [Google Scholar]
- K Keskinbora, I Aydinli. Long-term results of suprascapular pulsed radiofrequency in chronic shoulder pain. Agri 2009. [Google Scholar]
- K Kingston, E J Curry, J W Galvin, X Li. Shoulder adhesive capsulitis: epidemiology and predictors of surgery. J Shoulder Elbow Surg 2018. [Google Scholar]
- AM Teja, RC Banshiwal. Frozen shoulder: Evaluation of intraarticular corticosteroids injection versus suprascapular nerve block a prospective clinical study. Int J Orthop 2017. [Google Scholar]
- JS Jang, HJ Choi, SH Kang, JS Yang, JJ Lee, SM Hwang. Effect of pulsed radiofrequency neuromodulation on clinical improvements in the patients of chronic intractable shoulder pain. J Korean Neurosurg Soc 2013. [Google Scholar]
- YT Wu, CW Ho, YL Chen, TY Li, KC Lee, LC Chen. Ultrasound-guided pulsed radiofrequency stimulation of the suprascapular nerve for adhesive capsulitis: a prospective, randomized, controlled trial. Anesth Analg 2014. [Google Scholar]
- DK Verma, O Neyaz, S Nanda, G Handa. Comparison of outcome of ultrasound-guided suprascapular nerve block versus intra-articular steroid injection in adhesive capsulitis of shoulder: A randomized control trial. Indian J Rheumatol 2019. [Google Scholar]
- EM Shanahan, M Ahern, M Smith, M Wetherall, B Bresnihan, O Fitzgerald. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis 2003. [Google Scholar]
- P Sinha, B Sarkar, S Goswami, PR Karmakar, SR Dasgupta, S Basu. Effectiveness of Combination of Ultrasonography-Guided Pulsed Radiofrequency Neuromodulation With Steroid at the Suprascapular Nerve in Chronic Shoulder Pain. Pain Pract 2020. [Google Scholar]
- F Luo, L Meng, T Wang, X Yu, Y Shen, Ji N. Pulsed radiofrequency treatment for idiopathic trigeminal neuralgia: a retrospective analysis of the causes for ineffective pain relief. Eur J Pain 2013. [Google Scholar]
How to Cite This Article
Vancouver
Rastogi S, Sharma D, Agrawal A, Rai S, Mahapatra S, Khan IA. A comparative study of triamcinolone injection alone versus combined triamcinolone injection with pulsed radiofrequency for frozen shoulder pain: A randomized controlled study [Internet]. Indian J Clin Anaesth. 2025 [cited 2025 Sep 03];12(1):66-72. Available from: https://doi.org/10.18231/j.ijca.2025.010
APA
Rastogi, S., Sharma, D., Agrawal, A., Rai, S., Mahapatra, S., Khan, I. A. (2025). A comparative study of triamcinolone injection alone versus combined triamcinolone injection with pulsed radiofrequency for frozen shoulder pain: A randomized controlled study. Indian J Clin Anaesth, 12(1), 66-72. https://doi.org/10.18231/j.ijca.2025.010
MLA
Rastogi, Shivani, Sharma, Deepti, Agrawal, Anurag, Rai, Sujeet, Mahapatra, Swagat, Khan, Imran Ahmed. "A comparative study of triamcinolone injection alone versus combined triamcinolone injection with pulsed radiofrequency for frozen shoulder pain: A randomized controlled study." Indian J Clin Anaesth, vol. 12, no. 1, 2025, pp. 66-72. https://doi.org/10.18231/j.ijca.2025.010
Chicago
Rastogi, S., Sharma, D., Agrawal, A., Rai, S., Mahapatra, S., Khan, I. A.. "A comparative study of triamcinolone injection alone versus combined triamcinolone injection with pulsed radiofrequency for frozen shoulder pain: A randomized controlled study." Indian J Clin Anaesth 12, no. 1 (2025): 66-72. https://doi.org/10.18231/j.ijca.2025.010
