- Visibility 21 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijca.2025.006
-
CrossMark
- Citation
Randomised controlled trial comparing the efficacy of ultrasound along with fluoroscopy versus fluoroscopy for lumbar selective nerve root block
Introduction
One of the most frequent complaints in clinical practice is low back discomfort. One of the most frequent complaints in clinical practice is low back discomfort. It is among the main global causes of disability. According to estimates, the lifetime prevalence of low back pain ranges from 60% to 90%,[1] with an incidence of 5% to over 30%.[1] A lower back discomfort that results from pressure or inflammation on nerve roots is referred to as lumbosacral radiculopathy. The compression of the nerve root is mostly caused by herniated discs in approximately 90% of cases.[2] Degeneration of the spinal vertebrae, and foramen stenosis (where the nerves leave the spinal canal) are other possible causes. Leg pain is one of the symptoms of lumbar radiculopathy (LR), which can also include tingling, numbness, weakness, and even paralysis. Inflammatory or compressive conditions affecting the spinal nerve roots, or both, may cause LR.[3] Since an incorrect diagnosis can result in an unsuccessful treatment, it is crucial to accurately diagnose the source of radicular pain and low back pain.[4] Radiculopathy, which is caused by compression of the nerve root, is diagnosed in the majority of patients by linkage of the imaging findings, clinical indicators, and symptoms. Nevertheless, radiological imaging and clinical findings are not perfect diagnostic tools. Non-operative treatment comprises rest, muscle relaxants, non-steroidal anti-inflammatory drugs, and physical therapy.[5] Under C-arm/ultrasound supervision, diagnostic selective nerve root blocks (SNRBs) inject local anaesthetic or other drugs around spinal nerves. Analgesic reactions (significantly reducing symptoms) and provocative responses (replicating symptoms during needle placement) to SNRB can be employed as diagnostic tools to confirm or exclude a specific nerve root as the cause of clinical symptoms.[6]
This method's basic idea is to inject a steroid with a local anaesthetic to reduce perineural inflammation.[7] Medications used in selective nerve root block include corticosteroids, which can inhibit the production and release of proinflammatory materials.[8] However, there is still a risk of corticosteroid-induced hypercortisolism, hyperglycaemia, fluid retention, and other systemic effects.[9] The C-arm has been in use for a while. Use of the C-arm in conjunction with ultrasound guided (US) has produced encouraging results. The anatomical structures of the surrounding muscles, intervertebral foramen, nerve roots, and blood vessels may all be clearly seen with ultrasound assistance. It can also precisely guide the puncture needle to the desired location in real time.[10] Apart from its low radiation exposure, the primary benefit of US selective nerve root block is its direct real-time visualization of vessels and nerves. It can also be utilized in locations where other methods could harm vessels in densely populated areas when the needle is advanced. Our goal was to determine whether, in comparison to using C-arm alone, using USG in conjunction with it would result in more accurate medication delivery, the elicitation of concordant pain, and a reduction in radicular discomfort.
Materials and Methods
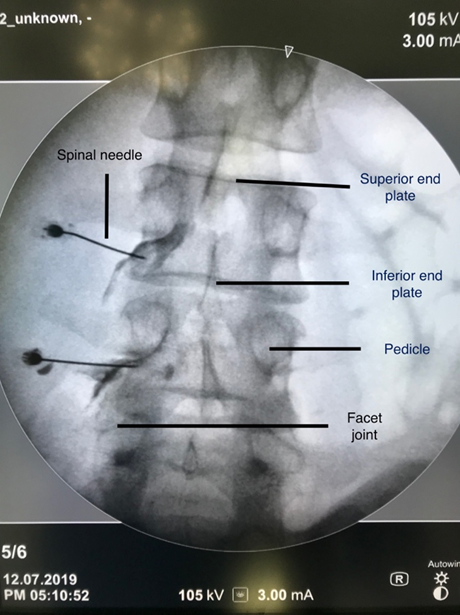
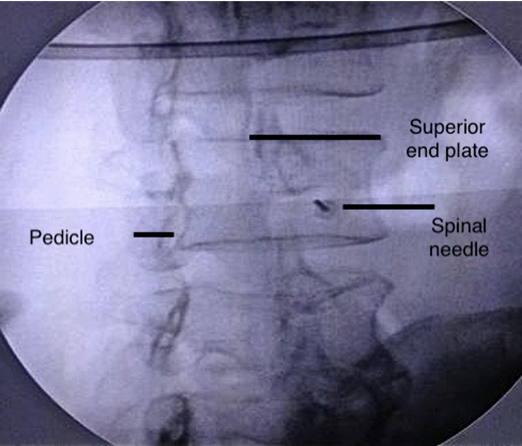
The study was conducted prospectively between June 2016 and June 2019. 78 patients who were over 20 but under 60 years old, complained of radicular pain with or without mild back pain, had intervertebral disc lesions affecting a specific lumbar nerve root, had foraminal stenosis without neurological deficit, had not received relief from their radicular pain after three months of non-operative treatment, and had radiological correlation were included in the study after receiving approval from the institutional review board. Patients with predominant back pain than radiculopathy, neurological deficit, infective aetiology, cauda equina syndrome, lack of radiological correlation, post spine surgery, history of hypersensitivity to local anaesthetics, infection at the site of injection, cognitive dysfunction were excluded from the study. The spine surgeon and the pain specialist performed a thorough clinical examination of each patient, including a radiological correlation. Every patient had an MRI as part of regular procedure. The patients were allocated randomly into two groups by computer generated random allocation, group A (n=39) constituted of patients who were given fluoroscopy guided selective nerve root block and group B (n=39) constituted of patients who were given ultrasound and fluoroscopy guided selective nerve root block. Allocation was done by an independent researcher by sealed envelopes with random numbers generated by computer. Patients were informed about the procedure and clearly explained that they would have symptomatic improvement and there are high chances that pain may recur and patient might need surgery depending on the disease progression. All the patients had symptoms due to L4-L5, L5-S1 disc disease and among those, 58 patients had L4-L5 disc prolapse and 20 patients had L5-S1 prolapse. After obtaining informed consent, the patient was shifted to operation theatre and placed in prone position in a radiolucent table. Both ultrasound guided and fluoroscopy guided selective nerve root block was done by an anaesthesiologist with at least 2 years experience in interventional pain procedures. In order to visualize the "Scotty Dog" appearance in group A, selective nerve blocks at the L4-5 and L5-S1 levels were performed under fluoroscopy. The image intensifier was tilted to 15 degrees and maintained in an anteroposterior position. Two millilitres of 2% lignocaine were used to anesthetize the skin covering the insertion site. A 22-gauge spinal needle was inserted toward the "safe triangle" inferolateral to the pedicle, with the needle being positioned close to the nerve root. 0.5 mL of Omnipaque (Iohexol) contrast solution was injected to ensure the correct position of the needle and the nerve root after the proper needle positioning was confirmed under anteroposterior (AP) and lateral fluoroscopic position ([Figure 1], [Figure 2]). Following the visualization of the radiculogram, 2 millilitres (80 mg) of triamcinolone acetonide and 1 millilitre of 0.25% bupivacaine are injected around the nerve root. After the surgery, a sterile dressing was used.
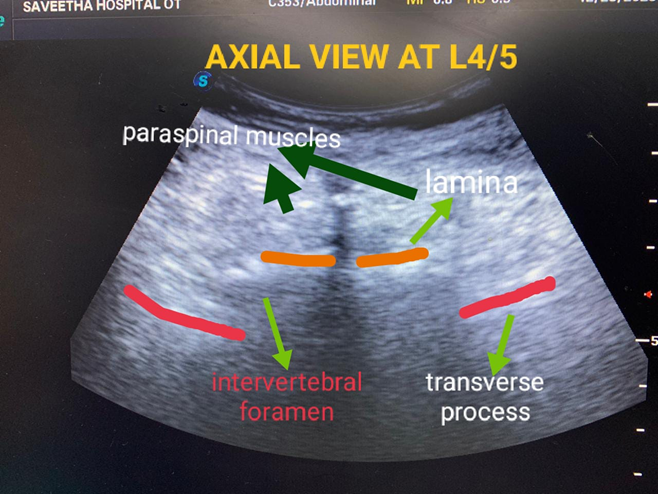
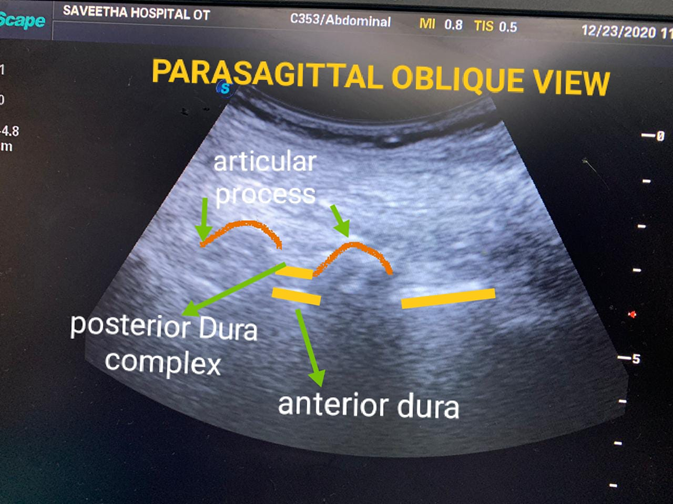
In group B, selective nerve blocks at L4-5 and L5-S1 levels were done under ultrasound guidance and the patients were placed in prone position with curvilinear transducer (3-8 MHz) draped in a sterile cover (sonoscape S8 Exp, China) and C-arm in AP and lateral position. Spine vertebral level was obtained by placing the transducer in midline sagittal and parasagittal oblique view following which the transducer was kept in axial view in which the interspinous space, lamina, transverse process and the intervertebral foramen was identified ([Figure 3], [Figure 4]). The needle was advanced in plane with the transducer and the needle was inserted lateral to lamina and progressed into the intervertebral foramen. The C-arm was used to assess the needle tip's position, and Doppler was started over the needle tip to rule out any vascular structures close to it. Following the verification of the accurate positioning of the 22G spinal needle, 0.5mL of Omnipaque (Iohexol) contrast solution was administered to ascertain that the needle was in the intended location near the chosen nerve root. Once the position was established, 1ml of 0.25% bupivacaine was mixed with 2ml (80mg) of triamcinolone acetone. For roughly an hour, the patients were under surveillance. On the same day, the patients were released with instructions for a typical post-procedure regimen: one day of rest and restricted activity based on personal comfort levels. After two hours, they were only permitted to walk for necessary motions. The patient was checked on every two days, five days, one week, two weeks, six weeks, three months, and six months. The patients were asked to rate their pain on a scale of 0 to 10, with 0 denoting no pain and 10 denoting the worst possible agony, in order to calculate the VNS score outcomes.[11], [12] Using the study by Wenxing et al, we took a sample size of 40 for our study with a power of about 80% and with an alpha error of 5%.[13] The Statistical Package for Social Sciences, version 20, was used to analyse all the data that were entered into an Excel sheet. While intragroup analysis was analysed using a paired t-test, continuous data were reported as mean ± standard deviation and were subjected to independent samples t-test analysis. The number of patients (n) was used to represent categorical data, which were then subjected to Chi-square analysis. P less than 0.05 was deemed significant.
Results
Among 78 patients, 39 patients underwent the procedure under C - arm guidance (Group A), and 39 patients under C-arm and USG guidance (Group B). Mean age of patients in Group A were 45 years and Group B were 42.5 yrs. Of the total 78 patients concordant pain was elicited in 61 patients (78%). No pain relief was seen in 17(22%) patients in whom concordant pain was not elicited. Of 61[78%] patients, 54 of our patients were comfortable and were able to proceed with their day to day activities after just one block, 28 patients from Group A and 26 patients from Group B and 11 patients did not get pain relief in spite of elicitation of concordant pain. 24 patients required more than one block, 11 patients (46%) from Group A and 13 patients (54%) from Group B. Of the total 78 patients 52 patients had lumbar disc disease and 26 had foraminal stenosis. Of the total 24 patients requiring second block, 11 patients had pain relief and 13 patient required surgery. So of the total 78 patients, 65(83%) patients had pain relief and 13(17%) patients required surgery. These data are illustrated in [Table 1].
|
Total patients(78) |
||||
|
|
N |
Group A (39) |
Group B(39) |
Percentage (%) |
|
Concordant pain elicited with first block |
61 |
31 |
30 |
78.2 |
|
Pain relief After first block |
54 |
28 |
26 |
69.2% |
|
Patients requiring second block |
24 |
11 |
13 |
30.7% |
|
Pain relief after second block |
11 |
5 |
6 |
14.1% |
|
Patients requiring surgery |
13 |
6 |
7 |
16.7% |
Of the 52 patients with lumbar disc disease, 43(83%) had pain relief and only 9 patients required a second block among which 3 patients were from Group A and 3 patients from Group B and other 3 patients who did not get pain relief proceeded for surgery(1 from Group A and 2 from Group B). 26 cases of foraminal stenosis were studied, and among them 11 patients had relief with first block, 15 required two blocks(7 patients from Group A and 8 patients from Group B), and among them 10 patients proceeded for surgery because of inadequate pain relief (5 patients from Group A and 5 patients from Group B). There was no significance between Group A and Group B but significant between the Disc group and Foraminal group (p value < 0.001). These data are illustrated in [Table 1]. Postoperative hospital stay was the same in both groups.
In the Disc group, 49(94%) patients had pain relief and only 3 (6%) went ahead for surgery and in the foraminal group, 16(62%) patients had relief of pain and 10(38%) proceeded for surgery which is given. 17 patients who did not have concordant pain with the first block went for the second block and among them 7 had pain relief with the second block and we attribute this to improper to the elicitation of concordant pain in the second block which is illustrated in [Table 3]. 7 patients who had concordant pain with first block were given a second block and among them only 4 got relief while 3 proceeded for surgery which is illustrated in [Table 4]. Among foraminal group patients, 38% went for surgery compared to just 6% of disc patients and this is likely due to other causes of pain such foramen or recess narrowing, osteophyte formation and other mechanical factors that didn’t subside by nerve block in foramen group of patients compared to disc.
In our study, majority of the patients showed an improved of pre and post injection VNS scores. VNS scores of both groups are shown in [Table 5]. Of the total 78 patients only 13 (17%) patients had persistent pain and underwent surgery, 65 (83%) had an improvement of symptoms out of which 33 of patients were from Group A and 32 of patients were from group B. Among 78 patients, 65 patients had improvement of symptoms out of which 74% of patients were from Group A and 72% of patients from group B based on clinical improvement in the post injection VNS scores.
|
Group |
N |
Pain relief after first block |
Patients requiring second block |
Pain relief from second block |
Patients requiring surgery |
|
Lumbar disc |
52 |
43 (82.6%) |
9 (17.3%) |
6 (11.5%) |
3 (5.8%) |
|
Foraminal stenosis |
26 |
11 (42.3%) |
15 (28.8%) |
5 (9.6%) |
10 (19.2%) |
|
Total patients |
78 |
54 (69.2%) |
24 (30.7%) |
11(14.1%) |
13 (16.7%) |
|
No of patients who did not get concordant pain in first block (17) |
||||
|
Level |
Group A |
Group B |
||
|
L4-L5 |
L5-S1 |
L4-L5 |
L5-S1 |
|
|
DISC |
2 (11.7%) |
1 (5.9%) |
2 (11.7%) |
2 (11.7%) |
|
FORAMEN |
2 (11.7%) |
3 (17.7%) |
2 (11.7%) |
3 (17.7%) |
|
Pain relief after second block(7) |
||||
|
Level |
Group A |
Group B |
||
|
L4-L5 |
L5-S1 |
L4-L5 |
L5-S1 |
|
|
DISC |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
|
FORAMEN |
0 |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
|
No of patients who got concordant pain but no pain relief (7) |
||||
|
Level |
Group A |
Group B |
||
|
L4-L5 |
L5-S1 |
L4-L5 |
L5-S1 |
|
|
DISC |
2 (11.7%) |
1 (5.9%) |
2 (11.7%) |
2 (11.7%) |
|
FORAMEN |
2 (11.7%) |
3 (17.7%) |
2 (11.7%) |
3 (17.7%) |
|
Pain relief after second block (7) |
||||
|
Level |
Group A |
Group B |
||
|
L4-L5 |
L5-S1 |
L4-L5 |
L5-S1 |
|
|
DISC |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
|
FORAMEN |
0 |
1 (14.3%) |
1 (14.3%) |
1 (14.3%) |
|
Mean VNS Score |
Group A |
Group B |
|
PRE OP |
8.2 |
8.5 |
|
POD 2 |
3.4 |
4.2 |
|
POD 5 |
4 |
4.5 |
|
POD 7 |
4 |
4.2 |
|
1 Month |
5 |
5 |
|
3 Months |
4.5 |
5 |
|
6 Months |
5 |
4.5 |
Discussion
Radiating pain down the leg or foot from the lower back is known as lumbar radiculopathy. In both the cervical and lumbar areas, selective nerve root block (SNRB) is used in the diagnosis and treatment of radicular pain caused by a specific damaged nerve root.[14], [15], [16], [17] Surgery may not always be necessary for patients whose conservative care has failed; in these cases, selective nerve root block serves a critical therapeutic function. However, the results of conservative management are not always predictable. The clinical outcomes in these patients differ, even though SNRB does not cure the underlying condition that is generating the nerve root irritation. The degree of improvement in LLRP within 6 hours after selective nerve root block can predict the degree of improvement that will be experienced 12 months after surgery for only single level DLSS.[18] Patients who have not responded to conservative treatment, require anaesthesia, loss of control of the bladder or bowel sphincter, and significant neurological impairments should consider surgical surgery. Ultrasound (US)-guided nerve blocks have become more popular in recent years due to their benefits, which include real-time needle trajectory, mobility of the equipment, and the ability to visualize soft tissue without radiation exposure. The use of US-guided cervical selective nerve root block was documented by Galiano et al. in 2005, and a number of other investigations have confirmed the procedure's viability and efficacy.[19] The accuracy and pain relief degree of ultrasound guidance were similar to those of fluoroscopy guidance, but the operation time and needle angle adjustment times were significantly less than that of fluoroscopy guidance.[20] These trials, however, did not contrast the US-guided approach with alternative approaches, like fluoroscopy guided selective nerve root block. When Jee et al. evaluated the short-term treatment outcomes of FL-guided transforaminal epidural steroid injection (TFESI) and US-guided cervical selective nerve root block, they discovered no discernible intergroup differences.[17] Weiner and Fraser examined the effectiveness of selective nerve root block in thirty patients with foraminal and extra-foraminal disc herniation in a prospective trial. After a follow-up of one to ten years, they found that, out of the 28 patients, 22 (or 79%) saw a significant and long-lasting reduction in pain (Average follow-up: 3.4 years).[19] Nonetheless, out of the 78 patients in our trial, 54 individuals (26 from Group A and 26 from Group B) experienced significant symptom reduction and were able to resume their regular activities following SNRB.
A total of thirty people (aged 29 to 82) with a clinical picture of mono-radiculopathy in the lumbar region, radiographic evidence of herniation in 20 patients, and foraminal stenosis in 10 patients with mild neurologic loss were analysed in a retrospective study. After these patients were evaluated, it was determined that all of them needed surgical decompression; however, selective nerve root block with triamcinolone and bupivacaine was given to them instead. Five patients needed a second injection, whereas 26 patients (87%) experienced a quicker and more noticeable relief in pain. Following an average follow-up of 16 months (6-23 months), 60% of patients with disc herniation or foraminal stenosis saw a lasting remission of their pain, allowing for the postponement of surgery.[21] Of the 55 patients in a prospective research by Riew et al., 29 chose not to undergo surgery during the follow-up period following the nerve-root injections, even though all of them had initially desired it. Although every patient in the trial requested surgical intervention, they were all randomly assigned to receive SNRB treatment (bupivacaine plus betamethasone or bupivacaine alone). According to this study, patients with lumbar radiculopathy should be treated with corticosteroid injections into specific nerve roots before considering surgical intervention.[22] In our study, out of 78 patients, only 24 patients required more than one block (11 patients from Group A and 13 patients from Group B) and 13 patients ended up requiring surgery. Of the 52 disc patients, 49 (94%) patients had pain relief and only 3(6%) went ahead for surgery. Of the 26 foraminal cases, 16(62%) patients had pain relief while 10(38%) patients went for surgery. Similar to our study, Hazra et al RCT compared the effects of ultrasound versus fluoroscopy guided caudal epidural injection for patients with radiculopathy and chronic back pain. They discovered that both group’s post-injection scores on the VAS (visual analogue score) and ODI (Oswestry Disability Index) significantly improved.[22] Further multicentric research is required to validate our results. Sahu et al studied ultrasound guided and fluoroscopy verified SNRB and they measured number of attempts for identification of transforaminal space, number of needle passes, time taken for needle insertion and duration of radiation exposure and concluded that lumbar SNRB can be safely and efficiently done by ultrasound guidance but fluoroscopic verification with contrast is required to rule out intrathecal and intravascular spread.[23] Yang and colleagues studied the accuracy, effect on post procedure pain relief, and safety of Ultrasound guided SNRB in 80 patients with low back pain and radicular pain and they kept the needle tip at the lateral side of the lamina in the axis view and the middle of the adjacent facet joints in the parasagittal view and confirmed the needle placement with contrast in fluoroscopy. Their success ratio was 85% and had no difference in pain relief between both the groups.[24] Gofeld and colleagues did a feasibility and validation study of ultrasound guided lumbar SNRB with procedural accuracy and proposed anatomically sound approach with fluoroscopy validation in 50 patients. Out of 50 injections, they did 46 procedures and L5/S1 SNRB was not possible in 4 patients(8%). Fluoroscopy confirmed the correct placement in foramen in all 46 injections (100%). The contrast-spread pattern was extraforaminal (nerve root) in 4 patients (8.7%), intraforaminal in 42 patients(91.3%) and Intravascular injection was detected in 3 patients(6.5%).[13]
There are several factors which can affect the outcome of the study like ultrasound visibility of neuraxial structures, experience of the personnel doing the procedure, resolution of ultrasound image which is based on the quality of ultrasound machine. Ultrasound guided SNRB is a reality these days with the availability of ultrasound machines with very good resolution and training in these procedures are required for acquiring results in patients. Our study results are unique in ways that shows that eliciting concordant pain during procedure is vital for better long term post procedure symptom relief in patients with lumbar disc prolapsed and compared the effect of SNRB in patients with posterior disc prolapse and foraminal stenosis. This data adds new evidence to the efficacy of SNRB in lumbar canal stenosis and foraminal stenosis and further multicentric studies are required to validate our results. Our suggestion is to elicit concordant pain during SNRB which is vital for long term results and switch over to ultrasound guided SNRB with fluoroscopy as an adjuvant which is efficacious both to the patient and physician in terms of real time placement of needle, anatomical precision, radiation and efficacy. Limitations of our study are that we didn’t include ultrasound visibility score in our study which is one of the factors which can influence the success of the procedure, expertise is required to perform ultrasound guided neuraxial procedures, translation of the same knowledge to patients with obesity, post spine surgery, scoliosis is limited.
Conclusion
US guided SNRB with fluoroscopy as an adjuvant versus fluoroscopy alone was similar in terms of pain relief and functional outcome. Patients in whom concordant pain was elicited had better outcome compared to patients in whom concordant pain was not elicited and patients in disc group had favourable outcome compared with the foramina group. There was no incidence of complications in both the groups. On the other hand, US guided selective nerve root block with fluoroscopy as an adjuvant has the advantage of reduced radiation exposure. Hence, we conclude that US guided SNRB with fluoroscopy as an adjuvant is a reasonable alternative to fluoroscopic guided SNRB.
Disclosure Statement
No potential conflict of interest was reported by the authors.
Source of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' Contributions
All authors contributed to data analysis, drafting, and revising of the paper and agreed to be responsible for all the aspects of this work.
References
- CE Alexander, LJ Weisbrod, M Varacallo. . Lumbosacral Radiculopathy 2024. [Google Scholar]
- T Kanaan, R Abusaleh, J Abuasbeh, M Al, Jammal, S Al-Haded. The Efficacy of Therapeutic Selective Nerve Block in Treating Lumbar Radiculopathy and Avoiding Surgery. J Pain Res 2020. [Google Scholar]
- D Hoy, P Brooks, F Blyth, R Buchbinder. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol 2010. [Google Scholar]
- RA Deyo, AK Diehl. Lumbar spine films in primary care: current use and effects of selective ordering criteria. J Gen Intern Med 1986. [Google Scholar]
- M Sakai, A Inokuchi, R Imamura, T Izumi, M Yamamoto, M Yoshimoto. Efficacy of Nerve Root Block for the Treatment of Lumbar Spinal Canal Stenosis in Adults Older than 80 Years of Age. Cureus 2022. [Google Scholar]
- R Beynon, MMC Elwenspoek, A Sheppard, JN Higgins, AG Kolias, RJ Laing. The utility of diagnostic selective nerve root blocks in the management of patients with lumbar radiculopathy: a systematic review. BMJ Open 2019. [Google Scholar]
- K Arun-Kumar, S Jayaprasad, K Senthil, H Lohith, KV Jayaprakash. The outcomes of selective nerve root block for disc induced lumbar radiculopathy. Malays Orthop J 2015. [Google Scholar]
- S Ko, S Chae, W Choi, J Kwon. Prolonged pain reducing effect of sodium hyaluronate-carboxymethyl cellulose solution in the selective nerve root block (SNRB) of lumbar radiculopathy: a prospective, double-blind, randomized controlled clinical trial. Spine J 2019. [Google Scholar]
- S Ko, C Jun, J J Lee, J Nam. Comparison of the effects of corticosteroid and hyaluronic acid-carboxymethylcellulose solution on selective nerve root block for lumbar radiculopathy: A prospective, double-blind, randomized controlled clinical trial. Pain Pract 2021. [Google Scholar]
- L Guang-Hui, Z Guang-Yu, L Yu-Zhang, Z Yong-Tao, Z Shi-Min, J Jiao. Value of ultrasound-guided transforaminal nerve block in the treatment of lumbar disc herniation. J Int Med Res 2020. [Google Scholar]
- H Jee, JH Lee, J Kim, KD Park, WY Lee, Y Park. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: A randomized, blinded, controlled study. Skeletal Radiol 2012. [Google Scholar]
- CT Hartrick, JP Kovan, S Shapiro. The numeric rating scale for clinical pain measurement: a ratio measure. Pain Practice 2003. [Google Scholar]
- W Zhao, G Guo, Q Wang, L Yang. Ultrasound-guided transforaminal epidural injection with fluoroscopy confirmation for the treatment of unilateral lumbar radiculopathy: A randomized controlled non-inferiority study. Clin Neurol Neurosurg 2023. [Google Scholar]
- J Chung, J Yim, H Seo, S Kim, K Cho. The Efficacy and Persistence of Selective Nerve Root Block under Fluoroscopic Guidance for Cervical Radiculopathy. Asian Spine J 2012. [Google Scholar]
- L Anderberg, M Annertz, L Persson, L Brandt, H Säveland. Transforaminal steroid injections for the treatment of cervical radiculopathy: a prospective and randomised study. Eur Spine J 2006. [Google Scholar]
- M Narozny, M Zanetti, N Boos. Therapeutic efficacy of selective nerve root blocks in the treatment of lumbar radicular leg pain. Swiss Med Wkly 2001. [Google Scholar]
- P Soni, J Punj. Ultrasound-Guided Lumbar Transforaminal Epidural Injection: A Narrative review. Asian Spine J 2021. [Google Scholar]
- S Ko, C Jun, W Min, E Son, S Lee, GW Lee. Pain Relief After Selective Nerve Root Block as a Predictor of Postoperative Functional Outcome in Patients with Degenerative Lumbar Spinal Stenosis Patients Undergoing Decompressive Surgery. Spine (Phila Pa 1976) 2021. [Google Scholar]
- K Galiano, A Obwegeser, G Bodner, M Freund, H Gruber, H Maurer. Ultrasound-Guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med 2005. [Google Scholar]
- B Wang, Y Sun, J Zhang, H Meng, H Zhang, L Shan. Ultrasound-guided versus fluoroscopy-guided lumbar selective nerve root block: a retrospective comparative study. Sci Rep 2024. [Google Scholar]
- BK Weiner, RD Fraser. Foraminal injection for lateral lumbar disc herniation. J Bone Joint Surg Br 1997. [Google Scholar]
- KD Riew, Y Yin, L Gilula, KH Bridwell, LG Lenke, C Lauryssen. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am 2000. [Google Scholar]
- G Yang, J Liu, L Ma, Z Cai, C Meng, S Qi. Ultrasound-guided Versus Fluoroscopy-controlled Lumbar Transforaminal Epidural Injections: A Prospective Randomized Clinical Trial. Clin J Pain 2016. [Google Scholar]
- M Gofeld, SJ Bristow, SC Chiu, CK Mcqueen, L Bollag. Ultrasound-guided lumbar transforaminal injections: feasibility and validation study. Spine (Phila Pa 1976) 2012. [Google Scholar]
