Introduction
Difficult airways often necessitate multiple attempts and correlate with higher rates of complications and peri-intubation adverse events such as oesophageal intubation, airway trauma, and hypoxia.1 The prevalence of difficult intubations using laryngoscopes varies between 1.5% and 20%.2 Among 2.9 million general anaesthetics recorded in the 4th national audit project (NAP4) of the Royal College Of Anaesthetist database, severe complications, such as death, hypoxic brain injury, or emergency surgical airway, occurred at a rate of 1 in 22,0001.
Managing a difficult airway in patients undergoing decompressive cervical laminectomy presents a unique challenge, requiring a carefully tailored approach to ensure safe and effective intubation while minimizing the risk of perioperative complications.
Awake tracheal intubation (ATI) has emerged as the gold standard for managing predicted difficult airways.3 Commonly, Awake tracheal intubation has been conducted utilizing a flexible bronchoscope. Recently, ATI with video laryngoscope(VL) has become a core technique.4 Dual video-assisted flexible intubation (VAFI) integrates the benefits of both techniques and is currently garnering more attention.5 The term hybrid intubation refers to the amalgamation of two distinct techniques of intubation. Awake hybrid intubation helps to increase the first pass success rate and reduces adverse events.6 This case report delineates the successful application of awake hybrid intubation using an indigenously made video laryngoscope and flexible video bronchoscope in a patient with an anticipated difficult airway undergoing decompressive cervical laminectomy. The Objective of this case report is to highlight the efficacy and safety of this Awake Hybrid Intubation (AHI) technique as an alternative approach for securing the airway in patients with cervical spine pathology undergoing surgery, thereby contributing to the literature on airway management strategies in challenging clinical scenarios.
Case Presentation
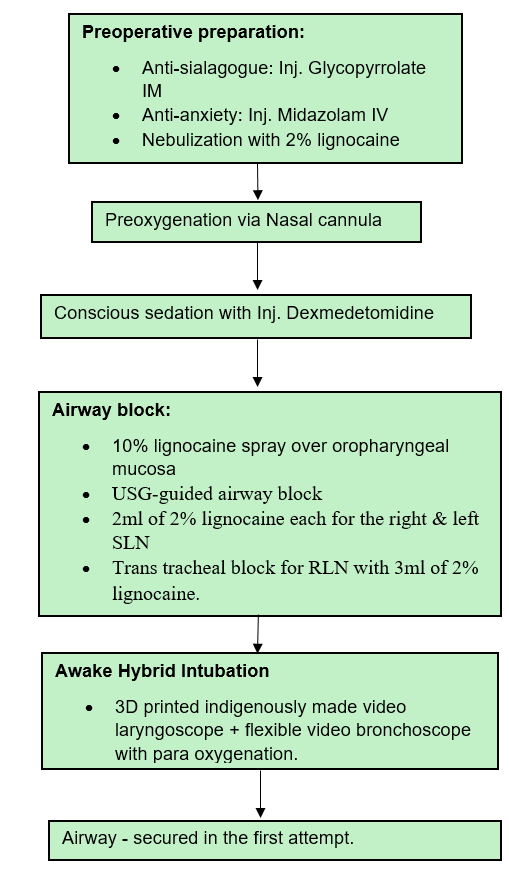
A 56-year-old male, weighing 62kilogram, known case of systemic hypertensive disorder on regular medication came with complaints of neck pain radiating to the left upper limb for 15 days and difficulty in lifting the left upper limb for 15 days. MRI cervical spine revealed cervical C3-C6 extradural space-occupying lesion with C4 C5 extra foraminal extension. He was planned for C3-C7 decompressive laminectomy and total excision of the canalicular component with posterior stabilization surgery. Preanesthetic airway assessment revealed an anticipated difficult airway (Table 1). The patient had limited extension at the atlanto-occipital joint and restricted flexion of the cervical spine, edentulous jaw, and sunken cheeks. Difficult laryngoscopy, difficult mask ventilation and increased risk of rapid desaturation were suspected. Hence according to the ASA guidelines for anticipated difficult airway in adults,7 we planned for an awake intubation. As per the literature, the awake hybrid technique has more first pass success rate with less adverse events,6 so we decided to proceed with awake hybrid intubation. The patient was counselled for AHI and written informed consent was obtained. The AHI technique mandates two skilled operators or anesthesiologists. With the use of video laryngoscope, the first anesthesiologist will enhance the visualisation of glottis by displacing the epiglottis, The next step involves the second operator employing the flexible bronchoscope as a maneuverable bougie to facilitate tracheal intubation, and then utilizing it as an introducer for the tracheal tube. In the preoperative unit, anti-sialagogue Injection (Inj.) Glycopyrrolate 0.2mg was given IM followed by Inj. Midazolam 1mg IV as an anti-anxiety measure. Nebulised with 2% lignocaine (40mg), for conscious sedation, Inj. Dexmedetomidine 0.5 mcg/kg IV infusion was started. Nasal cannula was used for oxygenation (4L). The patient was shifted to the OR. Intraoperative monitoring was done using standard ASA monitors. 10% lignocaine spray (40mg) was sprayed over the oropharyngeal mucosa. USG-guided airway block (Figure 2, Figure 3) was done with 2ml of 2% lignocaine each for the right & left superior laryngeal nerve, transtracheal block was given with 3ml of 2% lignocaine. A 3D-printed indigenously made video laryngoscope (Figure 4) was introduced by the first anaesthesiologist. After achieving a Percentage Of Glottic Opening (POGO) score of 50%, a Flexible video bronchoscope loaded with an armoured reinforced tube was introduced orally by the second anaesthesiologist which served as a guide for successful endotracheal tube (ETT) placement in the first attempt. As an incidental finding, a mass of about 1x2cm was found just beneath the glottis with the aid of the bronchoscope. The bronchoscope, along with the ETT, was manipulated skilfully to traverse the swelling without causing harm. The ENT specialist planned for a biopsy of the swelling later after this procedure. The hybrid technique (Figure 5), incorporating an indigenously manufactured video laryngoscope for improved airway visualization and a flexible bronchoscope for guiding the endotracheal tube placement, led to a safe and successful intubation process without adverse events. Para oxygenation using a nasal cannula was maintained throughout the intubation. Steps of our intubation are outlined in (Figure 1). After ensuring the correct placement of the ETT by visualizing the tracheal rings using the bronchoscope, clinically through auscultation and EtCo2 confirmation, Inj. Propofol 2mg/kg, Inj. Fentanyl 2mcg/kg were given. Neuromuscular Blockade was achieved with Inj. Vecuronium. The radial arterial line was secured for IABP monitoring and serial ABG analysis. Anaesthesia was sustained through volume-controlled mechanical ventilation employing isoflurane, Inj. Propofol infusion through TCI pump, Inj. Dexmedetomidine infusion at 0.5mcg/kg/hr and intermittent IV vecuronium administration. (Figure 6) shows the airway being secured safely after intubation. The surgical procedure lasted for about 6 hours in the prone position. The patient was hemodynamically stable throughout the procedure. He was extubated on the table uneventfully.
Table 1
Airway assessment components
|
Teeth |
Edentulous |
|
Inter incisor gap |
5cm |
|
Modified mallampatti |
Iii |
|
Neck movement |
Restricted |
|
Thyromentaldistance |
5.8cm |
Figure 3
Indigenously made video laryngoscope showing the passage of flexible bronchoscope into the glottis

Discussion
The utilization of AHI in anticipated difficult airways, particularly in situations where intubation is proceeded in a neutral head position, represents a paradigm shift in airway management strategies. This case underscores the importance of a multidisciplinary approach, meticulous planning, and adaptability in addressing complex airway challenges.
In scenarios of difficult airway management where conventional laryngoscopy proves ineffective, alternative techniques including non-channelled video laryngoscopy, non-channelled video laryngoscopy with hyper-angulated blades, channelled devices, rigid optical stylets, awake tracheal intubation, awake fibreoptic intubation, awake video laryngoscopy, and intubation via supraglottic airway devices should be considered.8
A randomized control trial study done by Mazzinari et al. on comparing the first pass success rate between dynamic and stylet-guided intubation in difficult airway using a glidescope proved that the successful first attempt intubation rate was significantly higher when utilizing the fiberscope as a dynamic guide during Glidescope laryngoscopy compared to the control standard stylet-guided intubation.9 In our case, we used the flexible bronchoscope as a dynamic guide during video laryngoscopy and achieved success on the first attempt.
A recent study done by M.L.Stein et al. on determining the efficacy of a hybrid technique using VL Scopy and flexible bronchoscopy revealed that this hybrid technique had success rates similar to advanced airway techniques. The same study suggested that the hybrid technique combining the VL scopy and flexible bronchoscopy can be used as an alternative rescue technique while developing an airway plan in paediatric patients with difficult airway.6
The capacity to secure the airway in a patient with intact intrinsic airway tone underscores the superior safety profile of awake tracheal intubation (ATI) compared to techniques involving heavy sedation or anesthesia.10 In our case, we combined the ATI and hybrid technique which increased the safety and aided in securing the airway without complications.
In our case, the patient had anticipated difficult airway with suspected difficult laryngoscopy, difficult mask ventilation and increased risk of rapid desaturation. The recent ASA guidelines for anticipated difficult airways suggests awake intubation in this scenario.7 From the literature, the AHI has more first pass success rate with less adverse events6. Hence in our case we used awake hybrid intubation technique.
In our case, the successful use of AHI facilitated the safe passage of the endotracheal tube in a patient with a potentially compromised airway with restricted neck movement due to pathology involving the cervical spine. Maintaining spontaneous ventilation during the procedure mitigates the risk of airway collapse and hypoxia, which may be exacerbated by anaesthetic induction in patients with cervical spine instability.
Furthermore, the utilization of video laryngoscopy in conjunction with awake flexible bronchoscope intubation provided a dynamic visualization of the airway anatomy, enabling precise placement of the endotracheal tube while minimizing trauma and optimizing patient comfort. The judicious use of sedatives and local anaesthetics helps alleviate patient anxiety and discomfort while preserving the ability to maintain airway patency and responsiveness throughout the intubation process.
Continued education, training, and proficiency in advanced airway management techniques are essential for anaesthesia providers to ensure readiness to address difficult airway situations effectively. Through ongoing refinement of skills and the adoption of innovative approaches such as awake hybrid intubation, clinicians can optimize patient outcomes and enhance the quality of care in the perioperative setting.
Limitation
Awake hybrid intubation requires specialized training and expertise, which may limit its widespread adoption. Future studies could focus on evaluating the learning curve associated with the technique and developing standardized training protocols to ensure proficiency among healthcare providers.
Conclusion
The findings presented in this case report underscore the significance of awake hybrid intubation as a safe and effective technique for managing difficult airways in patients undergoing cervical decompression surgery. By combining video laryngoscopy- guided intubation with fiberoptic bronchoscopy assistance, this approach offers several advantages, including the preservation of spontaneous ventilation, avoidance of apnea-related complications, and minimized risk of exacerbating cervical spine instability. Moving forward, large-scale prospective studies comparing the outcomes of AHI and other awake tracheal intubation techniques are warranted to validate the findings of this case report and establish awake hybrid intubation as a standard of care in airway management for cervical decompression surgery.