- Visibility 206 Views
- Downloads 19 Downloads
- Permissions
- DOI 10.18231/j.ijca.2024.073
-
CrossMark
- Citation
A randomised, double blinded control study to compare the efficacy of intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief in patients undergoing laparoscopic appendicectomy
Abstract
Background: Patients scheduled for laparoscopic appendicectomy encounter moderate to severe shoulder pain on the first postoperative day. Intraperitoneal nebulization of local anaesthetics is a new technique which provides uniform spread of local anaesthetic drug particles all through the peritoneum thus providing enhanced analgesic efficacy when compared to intraperitoneal instillation which provides non uniform distribution of the drug.
Materials and Methods: Fifty participants posted for laparoscopic appendicectomy under general anesthesia were randomized into Group A (Intraperitoneal nebulization of 8ml ropivacaine 0.75%) and Group B (intraperitoneal instillation of 8ml ropivacaine 0.75%). Our primary aim was to evaluate analgesic efficacy in both the groups postoperatively. Our secondary objectives were to compare the incidence of shoulder pain post operatively, total 48 hours fentanyl consumption and postoperative complications like nausea & vomiting and paralytic ileus.
Results: There was statistically significance in the pain scores at 24 hours (static pain p=0.003 and dynamic pain p=0.005) & at 48 hours after surgery (static pain p=0.00 and dynamic pain p=0.015). Significant difference was seen in the incidence of shoulder pain. In Group A, no patients complained pain in shoulders while in Group B a maximum of 6 patients complained shoulder pain postoperatively (p=0.022). The total fentanyl consumption over 48 hours was 0.20 ± 0.005 in Group A and 0.80 ± 0.957 in Group B (p = 0.008). Occurrence of postoperative Nausea & Vomiting were similar in both groups. None of the patients complained paralytic ileus in both groups as systemic absorption of the ropivacaine is also considerably less in comparison to other local anaesthetic drugs .
Conclusion: Intraperitoneal nebulized ropivacaine provides greater reduction in postop pain, lesser consumption of opioids, reduction in referred shoulder pain in laparoscopic appendicectomy patients.
Introduction
Intraperitoneal carbon dioxide (CO2) instillation during laparoscopic surgeries leads to stretching of peritoneum, irritation of diaphragm and retention of the CO2 gas within the abdomen causing postoperative pain for the patients. Visceral and shoulder pain can be attributed mainly to the irritation of peritoneal nerves.
Almost 70% patients undergoing laparoscopic surgery require strong opioids for analgesia, however, the opioids are associated with undesirable side effects like nausea & vomiting and delayed gastric motility leading to morbidity and delayed recovery.[1] USG (ultrasonography) guided Transversus Abdominis Plane block is a routinely performed analgesic technique but its role is limited due to the skill required and it has no effect on shoulder pain. Injections of local anesthetics into the peritoneal cavity have been reported to attenuate postoperative analgesic requirements post laparoscopic surgery however the evidences are conflicting.[2]
Intraperitoneal nebulization of local anesthetic drugs is a newer technique that provides uniform drug distribution all over the peritoneal cavity thus providing greater analgesia.[3] Intraperitoneal local anesthetic instillation is widely studied for postoperative pain relief nevertheless the spread of drugs into the peritoneal surface in non-homogenous and some portions of the drugs may get removed through secured abdominal drain.[4] Several studies have established the fact that instilling or nebulizing local anesthetic drugs into the peritoneum can block the visceral pain receptors thus proving advantageous in relieving pain by followed by laparoscopic surgery.[5], [6] We hypothesized that nebulized local anesthetics into the peritoneal cavity would attenuate the postoperative pain following laparoscopic appendicectomy.
Our primary objective was to evaluate the analgesic efficacy of intraperitoneal nebulization versus instillation of ropivacaine for reducing the postoperative pain in patients undergoing laparoscopic appendicectomy. Secondary Objectives were to assess the incidence of shoulder pain, total 48 hours fentanyl consumption and postoperative complications like nausea & vomiting and paralytic ileus.
Materials and Methods
After obtaining approval of the Institute’s Ethical board (SNMC/IECHSR/2020-21/A-46/1.1) Indian Clinical Trial Registration of the research was done (CTRIno2021/03/032115). Written and informed consent was taken from all patients. Our study adhered to guidelines set forth in the Helsinki Declaration.
Fifty patients of aged 18-60 years with Body Mass Index (BMI) ≤30 kgm-2 belonging to American Society of Anaesthesiologists (ASA) classification I / II electively posted for laparoscopic appendicectomy under general anesthesia were considered for the study. Patients who refused to give consent, patients suffering from chronic pain and those taking antiepileptic drugs, pregnant/lactating women and those allergic to drugs like local anesthetics were excluded from the study. Patients who needed to convert from a laparoscopic to an open approach were excluded from the analysis because intraperitoneal nebulization or instillation of ropivacaine could not be performed. Thus, these patients were considered dropouts.
Randomization was done with computerized random number sequence in a sealed opaque envelope. Patients in the nebulization group (Group A) were given intraperitoneal nebulization through inline nebulizer with 8 ml (0.75%) ropivacaine whereas patients in the instillation group (Group B) were given intraperitoneal instillation with 8 ml (0.75%) ropivacaine. Both patient and the observer were blinded to the group allocation.
On shifting to the operation theatre, standard monitors like pulse oximetry (SPO2), electrocardiogram (ECG), Noninvasive blood pressure (NIBP), and end tidal Carbon dioxide (ETCO2) were connected and all the baseline parameters were recorded. Premedication glycopyrrolate(0.01mg/kg), midazolam (0.05mg/kg) along with fentanyl (2mcg/kg) IV were delivered. General anaesthesia was administered using propofol (2mg/kg) and vecuronium (0.1mg/kg) and tracheal intubation was carried out. Maintenance was done using oxygen and Nitrous oxide mixture (50:50) and isoflurane 1 to 1.5% end tidal concentration. Patients were then ventilated with Intermittent positive pressure ventilation (IPPV) maintaining an ETCO2 of 35 to 40 mmHg.
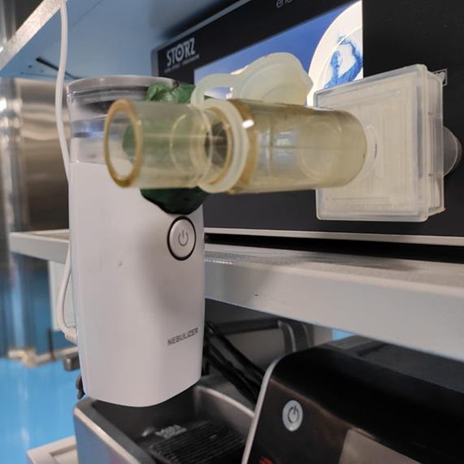
Laparoscopic appendicectomy was performed with one 10-mm port and two to three 5mm ports Pneumoperitoneum was attained by insufflating non-heated and non-humidified CO2 gas up to intraabdominal pressure of 12-15 mmHg. Nebulization was carried out through the main trocar at the onset of pneumoperitoneum using Inline mesh nebulizer (CONTEC Medical System Co Ltd China) as other ports were being inserted. The unit of nebulization was situated in between the insufflator & insufflation tubing. ([Figure 1])
Ropivacaine was administered to the peritoneum through the insufflator tubing (200cm long) connected to the umbilical port during gas insufflation. Patients of Group A were administered intraperitoneal nebulization and patients in the Group B were administered intraperitoneal instillation of 8 ml (0.75%) ropivacaine with 12ml of normal saline at two different time periods. Out of the prepared drug solution of 20ml the 1st half nebulization(10ml) commenced with insufflation via umbilical port, as other surgical ports were getting placed. The 2nd half of the nebulization(10ml) was carried out just before withdrawing the ports by the end of surgery. Nebulization was carried out for approximately 10 mins until the nebulizer chamber became empty. At the time of suturing, port site infiltration was done with ropivacaine 0.5% at the incision site.
Once surgery was over reversal of paralysis was done with neostigmine(0.05mg/kg) & glycopyrrolate (0.01mg/kg), then patient safely got extubated. Ondansetron 4mg IV was administered to prevent postoperative nausea & vomiting (PONV) at the end of surgery. As a multimodal analgesia all patients were administered paracetamol (15mg/kg) infusion. All patients were kept hospitalized until 48 hrs post-surgery. Pain at rest (static)and on coughing, deep breathing or changing position to sitting from supine (dynamic) was evaluated by Numeric rating scale (NRS), where 0 meant no pain and 10 signified extreme possible pain. Pain severity was graded based on NRS scoring (0-3) mild; (4-6) moderate and (7-10) severe. Pain assessment was done at 2, 4, 6, and 24h postoperatively in post anesthesia care unit (PACU) by an anesthetist unaware of group allocation. Patients experiencing static & dynamic NRS≥ 3 or those requesting pain relief, were administered (50mcg) Fentanyl bolus followed Subsequent rescue doses of fentanyl as required. Number of patients with significant pain (static and dynamic NRS >3), time for first rescue analgesia, and 48-hour analgesics utilization was documented.
The sample size was determined using OpenEpi Software (version 2.3.1). Based on the study by Kumar et al., which reported a static pain reduction score of 41 ± 14 for the nebulized group and 28 ± 14 for the instillation group, the required sample size was calculated.[7] With a 95% confidence level, 80% power, and α = 0.05 and β = 0.20, the sample size was estimated to be 19 per group, which was rounded up to 25 patients per group. Statistical analysis was performed using SPSS software (version 19). Quantitative data were presented as means and standard deviations, while qualitative data were expressed as percentages and proportions. To assess significance, independent t-tests and chi-square tests were employed, with a p-value of less than 0.05 considered statistically significant.
Results
The details regarding the study protocol are mentioned in the consort chart. ([Figure 2])

Demographic variables like age, weight gender, BMI etc. were similar among both groups ([Table 1])
|
Parameters |
Group A |
Group B |
P value |
Significance |
|
Age (Mean ±SD) |
42.90± 8.51 |
40.73± 9.44 |
0.397 |
NS |
|
Weight (Mean±SD) |
59.50± 9.98 |
58.28± 7.49 |
0.627 |
NS |
|
Gender |
|
|
|
|
|
Male |
16 |
15 |
0.0023 |
NS |
|
Female |
9 |
10 |
0.0023 |
|
|
BMI (Mean±SD) |
21.53 ±4.02 |
20.16± 3.33 |
0.100 |
NS |
|
ASA Status(I/II) |
15/ 10 |
13/12 |
|
NS |
No significant difference in postoperative pain scores (NRS >3) static & dynamic were observed immediately after surgery and 6 hours after surgery.
However significant difference between 2 groups in postoperative pain (NRS>3) @ 24 hours (static pain p=0.003 and dynamic pain 0.005) and 48 hrs after surgery (static pain p=0.00 and dynamic pain 0.015) were noted ([Table 2] and [Figure 3])
|
NRS score |
Group A (Nebulization) (Mean ±SD) |
Group B (Instillation) (Mean ±SD) |
P value |
Significance |
|
Immediately after surgery |
Nil |
Nil |
|
|
|
6 hours after surgery |
1.40±1.225 |
2.04±1.485 |
0.103 |
NS |
|
24 hours after surgery |
1.36±0.569 |
2.40± 1.528 |
0.003 |
HS |
|
48 hours after surgery |
1.12±0.526 |
2.20±1.190 |
0.000 |
HS |

First rescue of analgesia given was delayed in nebulization group when compared with instillation group. The overall 48hrs consumption of fentanyl between the groups was statistically significant (p=0.008) ([Table 3])
|
|
Group A |
Group B |
P value |
Significance |
|
Time for first Rescue Analgesia (hrs) |
0.80±1.915 |
5.84±8.484 |
0.006 |
S |
|
Total requirement of rescue analgesics in 48hours |
0.20±0.50 |
0.80±0.95 |
0.008 |
S |
Significant difference was seen in reduction of shoulder pain (p=0.022) In Group A, none of the patients complained pain in shoulders where as in Group B 6 patients complained shoulder pain postoperatively. Postoperative Nausea Vomiting was comparable within the groups. None complained paralytic ileus in both the groups ([Table 4]).
|
|
Group A |
Group B |
P value |
Significance |
|
Shoulder pain |
0/25 |
6/25 |
0.022 |
HS |
|
PONV |
2/25 |
6/25 |
0.123 |
NS |
|
Paralytic ileus |
0 |
0 |
|
|
Discussion
Analgesia for laparoscopic surgeries is conventionally provided by NSAID’s & opioids which are however not without undesirable side effects in the postoperative phase. Our research aimed to analyze the efficacy of nebulization versus instillation of intraperitoneal Ropivacaine for attenuating postoperative pain after laparoscopic appendicectomy.
Jagadeep Nayak et al. conducted a study comparing intraperitoneal nebulization of ropivacaine versus lignocaine for postoperative pain relief and hemodynamic stability in laparoscopic cholecystectomy.[7] Their findings suggested that ropivacaine provided a longer duration of analgesia and better hemodynamic stability than lignocaine. Hence, we opted to use ropivacaine for intraperitoneal nebulization and instillation in our laparoscopic surgeries. Due to its vasoconstricting properties, ropivacaine can increase intraperitoneal pressure, potentially causing collapse of peritoneal vessels. As a result, intraperitoneal ropivacaine is minimally absorbed into the systemic circulation, which may lead to fewer cardiac and neurological complications.[8] Several studies have established that ropivacaine nebulisation with or without opioids is more effective than placebo for post-operative pain relief after laparoscopic cholecystectomy without significant side effects.[9] Allegri et al., in their dose-finding study, concluded that 50 mg of ropivacaine nebulization provided effective pain relief in laparoscopic cholecystectomy surgeries. Based on these findings, we used 60 mg (8 ml of 0.75% ropivacaine, equating to 60 mg) for nebulization and instillation in both groups.[10]
In our study, we used Inline CONTEC-mesh nebulizer. It is not only reusable but also allows simultaneous administration of the anesthetic drugs while the surgery is performed. Particles arising from nebulization are much smaller thus leading to homogenous distribution of anesthetic drug particles throughout the peritoneum surface, thus acting on the nerve endings liable for local & systemic inflammation causing pain.[11] The only limitation similar to previous studies was fogging during nebulization throughout the procedure, to prevent that in our study- we have given 4ml ropivacaine nebulization during insufflation and the remaining 4ml was given after surgery, before deflation with average time being 10mins.
Kang H et al. evaluated the effectiveness of intraperitoneal instillation of ropivacaine in the relief of pain in patients undergoing laparoscopic appendectomy.[12] They observed that intraperitoneal ropivacaine instillation reduced pain during the post-operative period after laparoscopic appendectomy similar to our study however we noted better pain relief with ropivacaine nebulization than instillation.
Kumar et al. conducted a similar study comparing intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief following donor nephrectomy.[7] In comparison to Kumar et al., the study by Bucciero et al. observed that the reduction in postoperative pain was significantly different only at 6 hours (for both static and dynamic pain) and at 24 hours (for dynamic pain only).[13] However, in our study significant difference between 2 groups in postoperative pain (NRS>3) @ 24hours and 48 hrs after surgery were noted. This difference may be attributed to the fact that nephrectomy is generally a more painful procedure compared to the laparoscopic cholecystectomy performed in our study. Additionally, we utilized an objective Numeric Rating Scale (NRS) for assessing pain, whereas Kumar et al. used a subjective Visual Analog Scale (VAS). Our findings are consistent with reduced postoperative fentanyl consumption and a lower incidence of shoulder pain, supporting the effectiveness of our approach. They reported a higher incidence of postoperative nausea and vomiting (PONV) compared to our study. This discrepancy may be due to the lower pain scores and reduced fentanyl consumption observed in our study. Additionally, the incidence of shoulder-tip pain was significantly lower in Group A in our study. It is reasonable to suggest that the intraperitoneal administration of ropivacaine effectively blocked nociceptive input from the inflamed diaphragmatic peritoneum, contributing to this reduction in pain.
In studies conducted by Catenacci et al., Somaini et al., and Das et al., nebulization was found to provide better pain relief during the postoperative period.[14], [15], [16] Baird et al. showed no remarkable difference in the pain scores and opioid consumption, probably because of the decreased pain perception in children.[17]
Sai Sandhya et al. also studied intraperitoneal nebulization of ropivacaine in lap cholecystectomy.[18] They concluded that static and dynamic pain scores were significantly less in nebulized patients similar to our study. Similarly, Porika et al. compared intraperitoneal nebulization’s of ropivacaine versus bupivacaine.[19] They also concluded that both ropivacaine and bupivacaine were equally effective in relieving pain, which corresponds with our study’s findings.
The limitations of the current study include a smaller sample size and the focus on only laparoscopic appendectomy surgeries, which means our results may not be applicable to other cases such as long-duration surgeries or those involving peritoneal spillage. Additionally, due to practical difficulties, we could not measure patients' serum concentrations of the study drugs, so the exact amount of drug absorbed through nebulization or instillation remains unquantified. Although the dosage used was within safety limits, further research may be needed to address any potential safety concerns.
Future Scope
Further trials are necessary to evaluate the different techniques of administration into the peritoneal cavity to improve the post operative recovery in laparoscopic procedures.
Conclusion
Intraperitoneal nebulization offers enhanced postoperative pain relief, reduced opioid consumption, and a decrease in referred shoulder pain for patients undergoing laparoscopic appendectomy.
Sources of Funding
None.
Conflict of Interest
None.
References
- Lee L, Caplan R, Stephens LS, Posner K, Terman G, Voepel-Lewis T. Postoperative opioid-induced respiratory depression: a closed claims analysis. Anaesthesiology. 2015;122(3):659-65. [Google Scholar]
- Bhatia N, Mehta S, Saini V, Ghai B, Kaman L. Comparison of intraperitoneal nebulization of ropivacaine with ropivacaine-fentanyl combination for pain control following laparoscopic cholecystectomy: A randomized, double-blind, placebo-controlled trial. J Laparoendosc Adv Surg Tech A. 2018;28(7):839-44. [Google Scholar]
- Mcdermott A, Chang K, Mieske K, Mcanena P, Kinirons B, Abeidi A. Aerosolized intraperitoneal local anaesthetic for laparoscopic surgery: a randomized, double-blinded, placebo-controlled trial. World J Surg. 2015;39(7):1681-9. [Google Scholar]
- Singh D, Boga J, Saxena S, Chaudhary A, Bhusana S, Chandra G. The effect of intraperitoneal ropivacaine for post-operative pain management in patients undergoing laparoscopic cholecystectomy: A prospective double-blind randomized control study. Open J Anesthesiol. 2013;3(3):193-8. [Google Scholar]
- Kahokehr A, Sammour T, Soop M, Hill A. Intraperitoneal use of local anaesthetic in laparoscopic cholecystectomy: systematic review and metanalysis of randomized controlled trials. J Hepatobiliary Pancreat Sci. 2010;17(5):637-56. [Google Scholar]
- Choi G, Kang H, Baek C, Jung Y, Kim D. Effect of intraperitoneal local anesthetic on pain characteristics after laparoscopic cholecystectomy. World J Gastroenterol. 2015;21(47):13386-95. [Google Scholar]
- Kumar R, Nath S, Agarwal A. Intraperitoneal nebulization versus intraperitoneal instillation of ropivacaine for postoperative pain management following laparoscopic donor nephrectomy. Korean J Anesthesiol. 2019;72(4):357-65. [Google Scholar]
- Meissner W, Mescha S, Rothaug J, Zwacka S, Goettermann A, Ulrich K. Quality improvement in postoperative pain management: results from the QUIPS project. Dtsch Arztebl Int. 2008;105(50):865-70. [Google Scholar]
- Gowda A, Govil N, Kumar A, Singla D, Dhar M, Huda F. A Randomized Double-Blind Study Evaluating Intraperitoneal Ropivacaine Nebulization With and Without Nalbuphine for Post-operative Analgesia in Laparoscopic Cholecystectomy. Turk J Anaesthesiol Reanim. 2022;50(3):219-24. [Google Scholar]
- Allegri M, Ornaghi M, Ferland C, Bugada D, Meghani Y, Calcinati S. Peritoneal nebulization of ropivacaine during laparoscopic cholecystectomy: dose finding and pharmacokinetic study. Pain Res Manag. 2017;2017:1-9. [Google Scholar]
- Ingelmo P, Bucciero M, Somaini M, Sahillioğlu E, Garbagnati A, Charton A. Intraperitoneal nebulization of ropivacaine for pain control after laparoscopic cholecystectomy: a double-blind, randomized, placebo-controlled trial. Br J Anaesth. 2013;110(5):800-6. [Google Scholar]
- Kang H, Kim B. Intraperitoneal ropivacaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. J Int Med Res. 2010;38(3):821-32. [Google Scholar]
- Bucciero M, Ingelmo P, Fumagalli R, Noll E, Garbagnati A, Somaini M. Intraperitoneal ropivacaine nebulization for pain management after laparoscopic cholecystectomy: a comparison with intraperitoneal instillation. Anesth Analg. 2011;113(5):1266-71. [Google Scholar]
- Catenacci S, Lovisari F, Peng S, Allegri M, Somaini M, Ghislanzoni L. Postoperative analgesia after laparoscopic ovarian cyst resection: double-blind multicenter randomized control trial comparing intraperitoneal nebulization and peritoneal instillation of ropivacaine. J Minim Invasive Gynecol. 2015;22(5):759-66. [Google Scholar]
- Somaini M, Brambillasca P, Ingelmo P, Lovisari F, Catenacci S, Rossini V. Effects of peritoneal ropivacaine nebulization for pain control after laparoscopic gynecologic surgery. J Minim Invasive Gynecol. 2014;21(5):863-9. [Google Scholar]
- Das N, Deshpande C. Effects of intraperitoneal local anaesthetics bupivacaine and ropivacaine versus placebo on postoperative pain after laparoscopic cholecystectomy: a randomised double-blind study. J Clin Diagn Res. 2017;11(7):8-12. [Google Scholar]
- Baird R, Ingelmo P, Wei A, Meghani Y, Perez E, Pelletier H. Nebulized analgesia during laparoscopic appendectomy (NALA): A randomized triple-blind placebo-controlled trial. J Pediatr Surg. 2019;54(1):33-8. [Google Scholar]
- Sandhya S, Puthenveettil N, Vinodan K. Intraperitoneal nebulization of ropivacaine for control of pain after laparoscopic cholecystectomy-A randomized control trial. J Anaesthesiol Clin Pharmacol. 2021;37(3):443-8. [Google Scholar]
- Porika S, Naga L. Intraperitoneal nebulization of ropivacaine 0.75% vs intraperitoneal nebulization of bupivacaine 0.5% for post-operative analgesia in laparoscopic surgeries: Prospective double blinded randomised controlled trial. Int Arch Integr Med. 2018;5(9):105-17. [Google Scholar]
How to Cite This Article
Vancouver
Masur S, Kelageri S, Kumbar BV, Endigeri A. A randomised, double blinded control study to compare the efficacy of intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief in patients undergoing laparoscopic appendicectomy [Internet]. Indian J Clin Anaesth. 2024 [cited 2025 Sep 18];11(3):395-400. Available from: https://doi.org/10.18231/j.ijca.2024.073
APA
Masur, S., Kelageri, S., Kumbar, B. V., Endigeri, A. (2024). A randomised, double blinded control study to compare the efficacy of intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief in patients undergoing laparoscopic appendicectomy. Indian J Clin Anaesth, 11(3), 395-400. https://doi.org/10.18231/j.ijca.2024.073
MLA
Masur, Shilpa, Kelageri, Satish, Kumbar, Bhagyashri V, Endigeri, Archana. "A randomised, double blinded control study to compare the efficacy of intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief in patients undergoing laparoscopic appendicectomy." Indian J Clin Anaesth, vol. 11, no. 3, 2024, pp. 395-400. https://doi.org/10.18231/j.ijca.2024.073
Chicago
Masur, S., Kelageri, S., Kumbar, B. V., Endigeri, A.. "A randomised, double blinded control study to compare the efficacy of intraperitoneal nebulization and instillation of ropivacaine for postoperative pain relief in patients undergoing laparoscopic appendicectomy." Indian J Clin Anaesth 11, no. 3 (2024): 395-400. https://doi.org/10.18231/j.ijca.2024.073
