- Visibility 25 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijca.2024.062
-
CrossMark
- Citation
Analgesic efficacy of ultrasound-guided bilateral sphenopalatine ganglion block as a sole analgesic in fess surgeries and reconstructive nasal surgeries
- Author Details:
-
Vasantha Kumar K.R
-
Parijaat Mukherjee
-
Prashanth Gowtham Raj S.K *
Introduction
Regional anesthesia and nerve block techniques are increasingly being used for the management of postoperative pain in recent years. These nerve block techniques require a good understanding of the anatomy of the surgical site to successfully perform these nerve block techniques. Over the years, these techniques have evolved from anatomical landmarks to fluoroscopy-guided surgery, but there are no limitations. These techniques rely on landmarks visible on fluoroscopy without visible soft tissue. Thanks to the availability and capabilities of advanced ultrasound machines, the use of ultrasound guidance (USG) has become common practice to avoid damage to arteries and vascular system, to visualize the needle tip, to avoid intravascular injection, and to directly visualize injectable being deposited at the target structure.[1] Sphenopalatine ganglion block (SPGB) is considered a simple, effective, and safe method for treating craniofacial pain. With the help of anatomical bony landmark and supraszygomatic approach, allow the needle to easily pass through the pterygomaxillary cleft into the pterygoid fossa while preventing the needle from accidentally passing into other unintended locations.[1] There are several ways to block the pterygopalatine fossa (PPF). A recently described method is the USG technique which allows immediate visualization of the pterygopalatine fossa, external pterygoid plate, and maxillary artery. This technique allows easy access to its contents, including the maxillary artery, sphenopalatine ganglion (SPG), and deep and superficial nerves.[2] Studies show that approximately 40% of the surgical patients experience mild to severe pain within 24 hours after surgery.[3] The use of regional blocks for postoperative care is known to reduce hospital stay, overall costs, opioid consumption, and improved recovery.[4] SPG blockade has been shown to provide post-operative analgesia and reduce the need for analgesics.[5] Systemic use of non-steroid anti-inflammatory drugs (NSAIDs) and opioids will cause potential side effects. We plan to reduce the need for these systemic analgesic drugs & get rid of their potential side effects. The sphenopalatine ganglion is located within the pterygopalatine fossa. These ganglia communicate with the cervical sympathetic chain via deep petrosal nerves resulting in sympathetic activity in the form of visceral motor functions and parasympathetic activity via the superficial petrosal nerves. Primary sensory distribution is the palate, buccal mucosa, nose, and orbit.[6]
We conducted a study on bilateral SPGB under ultrasound guidance as a sole analgesic compared to fentanyl in patients undergoing FESS & reconstructive nasal surgeries performed with general anaesthesia. The primary aim of our study was to assess the analgesic effect, quality, and duration of analgesia of USG bilateral SPG block as a sole analgesic. In addition, the secondary aim was to further evaluate the adverse effects.
Materials and Methods
The randomized double-blind study was conducted between June 2022-June 2023, after approval of the institutional ethics committee bearing No.AIMS/IEC/119 with registration number EC/NEW/INST/2023/KA/0382. Informed written consent was obtained from all the patients.
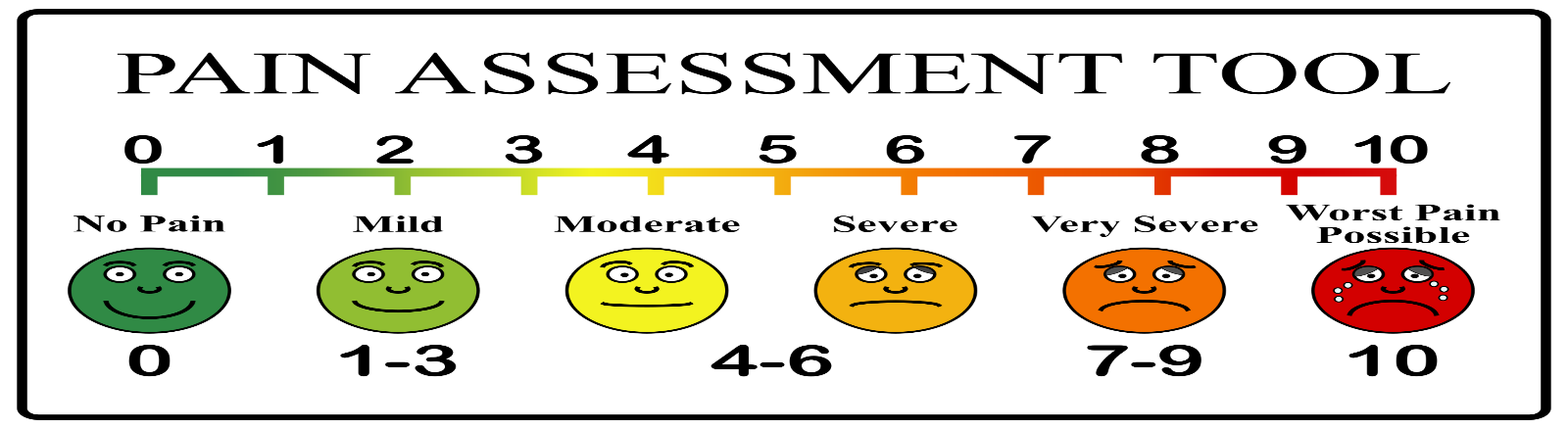
We enrolled 60 patients, 30 in each group according to inclusion & exclusion criteria. The study included participants with ASA1 &2, and below 18-60 years of either sex and patients undergoing elective procedures under general anaesthesia. Patients who refused, those with severe cardiovascular abnormality, bleeding disorders, increased intracranial pressure, on anticoagulants, local infection, with a known genetic susceptibility to malignant hyperthermia & history of allergy to test drugs were excluded. The night before surgery, we explained the block technique to the patients. All patients were instructed how to access their pain using a 10cm VAS, where score 0 denotes no pain & 10 indicates the maximum pain felt.[7]
Anesthesia: In the operating room, the hemodynamic data of the patient were recorded. All the patients underwent surgical procedures under general anesthesia with 0.02mg/kg of Midazolam IV, 2.5mg of Propofol 1%. Tracheal intubation was performed by a muscle relaxant IV inj. Atracurium 0.5mg/kg. Also, Isoflurane, oxygen, nitrous oxide, and intermittent positive pressure ventilation with atracurium bolus doses were used for the maintenance of anesthesia. All patients were ventilated mechanically to keep end-tidal CO2 between 35-45mmhg.
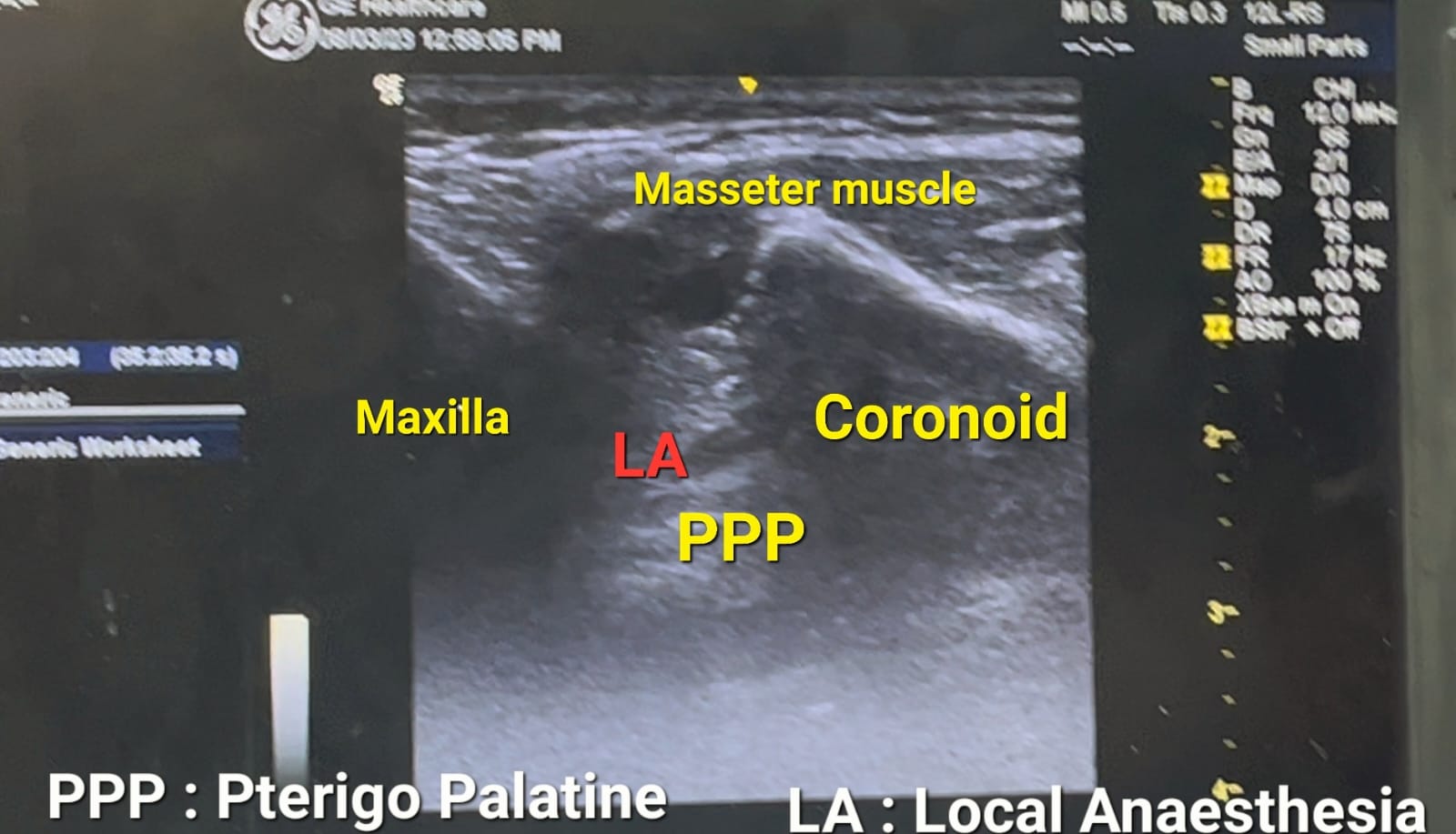
Procedure: The patients were randomized and divided into 2 groups of 30 patients in each group. In group (A) i.e. the interventional group in which USG guided bilateral sphenopalatine ganglion block was given under aseptic precaution. Group (B) i.e. the control group received fentanyl 2ug/kg intra-operatively as an analgesic. At the end of the surgical procedure, before the reversal of neuromuscular blockade bilateral SPG block was performed in the interventional group. A linear transducer probe was positioned longitudinally in front of the mandibular condyle with a cephalad angulation, bringing the coronoid & condylar processes into view. The space between the lateral pterygoid plate posteriorly & maxilla bone is seen anteriorly in the pterygopalatine fossa. The pulsatile maxillary artery was visualized just superficial to the lateral pterygoid muscle over the lateral pterygoid plate. The sphenopalatine artery which is a branch of the maxillary artery can be seen just anterior to the lateral pterygoid plate in PPF.
Under USG, a 25gauge needle was inserted using an out-of-plain approach,1-1.5cm superior to the zygomatic arch & posterior to the orbital rim, advanced in a lateral to medial & posterior to the anterior direction towards the PPF. Following negative aspiration, a mixture of 0.25% inj. Ropivacaine with 4mg inj. Dexamethasone, 7.5ml on each side was deposited in PPF in all patients belonging to interventional group A. Group B received fentanyl 2mcg/kg IV intraoperatively as an analgesic. After concluding the surgical procedure neuromuscular block was antagonized with neostigmine 0.05mg/kg & glycopyrrolate 0.01mg/kg and after achieving all extubating criteria, patients were extubated & shifted to the postoperative care unit.
Postoperatively VAS scores, total duration of analgesia, total analgesic consumption & side effects were noted soon after extubating, i.e. from 0 hrs till 48hrs postoperatively in all 60 patients. In both the groups rescue analgesia with Inj. Diclofenac 75mg was used only if the VAS score was equal to or more than 4.
Statically analysis
From the pilot study, the mean and standard deviation of the duration of analgesia for Group-1 (4.43 ± 0.62) and Group-II (5.05 ± 1.65).
n=[Z1-α/2+Z1-β]2×2S2d2
Where:
Z1−α/2=1.96 (for a 5% significance level)
Z1−β=1.037 (for 85% power)
S = (s1+s2)/2= (0.62+1.65)/2=1.135
S2 = 1.1352=1.288
2S2 = 2×1.288=2.576
d = Mean1−Mean2=4.43−5.05=−0.62
d2 = 0.3844
Plugging the values into the formula:
n = [1.96+1.037]2×2.5760/.3844
n = 8.98×2.576/0.3844n=23.132480.3844
n = 23.13248/0.3844
n = 60.24
Therefore, the sample size was determined to be 60, with 30 participants in each group.
Statistical analysis was accomplished using SPSS software & P-value<0.05 was considered statistically significant. Data were collected, transcribed manually scored at each visit & were reported as mean & standard deviation. Between groups statistical significance were assessed by Mann-Whitney test for VAS score & t-test for age.
Results
Demographic data
[Table 1] presents the comparison of age, sex, and gender between Group I and Group II. The mean age for Group I was 40.83 ± 11.82 years, while Group II had a mean age of 43.63 ± 10.62 years. The p-value for age comparison was 0.33, indicating no significant difference between the groups. Patients in both groups were compared with respect to demographic data. The sex distribution was as follows: Group I: 20 females (66.7%) and 10 males (33.3%). Group II: 19 females (63.3%) and 11 males (36.7%). There were no significant statistical differences between the groups in terms of sex distribution.
|
Variable |
Group I (n=30) |
Group II (n=30) |
P value |
|||
|
Age |
40.833+11.82 |
43.63+10.62 |
0.33 |
|||
|
Group |
Sex |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
|
Group A |
Valid |
F |
20 |
66.7 |
66.7 |
66.7 |
|
M |
10 |
33.3 |
33.3 |
100.0 |
||
|
Total |
30 |
100.0 |
100.0 |
|
||
|
Group B |
Valid |
F |
19 |
63.3 |
63.3 |
63.3 |
|
M |
11 |
36.7 |
36.7 |
100.0 |
||
|
Total |
30 |
100.0 |
100.0 |
|
Surgical procedures
[Figure 3], [Figure 4] illustrate the types of surgical procedures performed in Group A and Group B, respectively. No significant statistical differences were found between the two groups regarding the types of surgery.


Postoperative VAS scores and analgesia consumption
[Table 2] compares postoperative VAS scores and analgesia consumption up to 48 hours between the two groups.
In Group A, the VAS scores remained at 0 up to 8 hours postoperatively, with minor increases observed at 10 hours (mean = 0.33) and 12 hours (mean = 0.17). The scores remained minimal through 48 hours.
In Group B, VAS scores showed significant increases starting from 2 hours (mean = 0.17) to 48 hours (mean = 1.13), with higher scores compared to Group A at all time points beyond 2 hours.
The standard deviation in group A was 0.365,0.8840,0.461,0.183 & in group B was 2.03,1.77,2.03,2.13 at 8hrs,10hrs,12hrs & 16hrs respectively which were statistically significant as P-value remains <0.00 in group A. The standard deviation of VAS score for Group A was consistently lower than that of Group B, indicating more stable pain levels in Group A.
[Figure 5] illustrates the VAS scores up to 48 hours, showing consistently higher pain levels in Group B compared to Group A after 2 hours.
|
Statistics |
||||||||||||||||
|
Group |
0 hrs |
2 hrs |
4 hrs |
6 hrs |
8 hrs |
10hrs |
12 hrs |
16 hrs |
20 hrs |
24 hrs |
30 hrs |
36 hrs |
42 hrs |
48 hrs |
||
|
Group A |
N |
Valid |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
|
Missing |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
||
|
Mean |
0 |
0 |
0 |
0 |
0.07 |
0.33 |
0.17 |
0.03 |
0 |
0 |
0 |
0 |
0 |
0 |
||
|
Median |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
||
|
Std. Deviation |
0 |
0 |
0 |
0 |
0.365 |
0.884 |
0.461 |
0.183 |
0 |
0 |
0 |
0 |
0 |
0 |
||
|
Group B |
N |
Valid |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
30 |
|
Missing |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
||
|
Mean |
0 |
0.17 |
1.33 |
2.33 |
2.03 |
1.77 |
2.03 |
2.13 |
1.97 |
1.7 |
1.5 |
1.33 |
1.2 |
1.13 |
||
|
Median |
0 |
0 |
2 |
2 |
2 |
2 |
2 |
2 |
2 |
2 |
1 |
1 |
1 |
1 |
||
|
Std. Deviation |
0 |
0.648 |
1.213 |
0.711 |
0.669 |
0.817 |
0.809 |
0.681 |
0.669 |
0.596 |
0.572 |
0.479 |
0.61 |
0.73 |
||
|
|
|
P- Values |
1 |
0.154 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |

VAS scores were similar in both groups at 0 hrs. After 2 hrs, there were consistently higher VAS scores in Group B up to 48 hours. Even though VAS scores at 8 hrs, 10 hrs, 12 hrs & 16 hrs had slightly increased in Group A, they were statistically significantly lower compared to Group B.
Rescue analgesic consumption
[Figure 6] demonstrates a significant difference in the total consumption of rescue analgesics between the groups. Group A, the interventional group, had a mean consumption of 5 mg, whereas Group B, the control group, had a mean consumption of 49.32 mg. This difference was statistically significant, with a lower requirement for rescue analgesics in Group A.

Postoperative complications
The incidence of postoperative complications such as nausea, vomiting, headache, and bleeding was higher in Group B compared to Group A, as reported by the patients.
Overall, Group A experienced lower pain scores and required fewer rescue analgesics compared to Group B, with a higher incidence of postoperative complications observed in the control group.
Discussion
Sphenopalatine ganglion is one of the four parasympathetic ganglia in the skull, also known as Meckel’s ganglion and nasal ganglion.[8] The SPG carries only preganglionic parasympathetic axons. Both postganglionic and somatosensory afferents pass near the SPG.[9] SPG carries somatosensory, sympatho-secretory fibres supplying the nose, nasal cavity, palate, sinuses etc. FESS & Septo-rhinoplasty surgeries improve the patient’s quality of life of patients, but are associated with very significant postoperative pain and higher analgesics consumption. This study utilized an ultrasound-guided technique to block the sphenopalatine ganglion bilaterally and evaluated its ability to control postoperative pain in patients undergoing these surgeries. It is also important to maintain satisfactory analgesia to reduce the risk of bleeding due to distress & agitation. The study results suggested that group (A) patients who received Sphenopalatine ganglion block had reported significantly lower VAS scores as opposed to the control group (B) throughout 48 hours post-operatively. We found that patients in group (A) needed fewer rescue analgesics than group (B). The occurrence of side effects like nausea, vomiting, bleeding, headache, gastritis, etc was comparatively more in the control group (B). This block also reduces postoperative analgesic consumption & improves recovery characteristics with fewer side effects. The results of the present study are consistent with the results of previous studies conducted by many authors. Hwang et al. concluded SPG blockade applied before removal of nasal packing is an effective method of analgesia with minimal side effects.[10] Friedman et al. showed that SPG block was associated with prolonged postoperative analgesia following FESS.[11] Kesimci et al compared 3 groups of patients undergoing FESS using bupivacaine, levobupivacaine & saline given for bilateral SPG block.[12] They concluded that the patients who received bilateral SPG block with bupivacaine and levobupivacaine had excellent analgesia, lower VAS scores compared to group which received saline & with minimal side effects. De Maria et al. studied 70 patients to evaluate analgesia using the bilateral SPGB technique.[13] Their study suggested that SPGB decreased the hospitalization time & need for opiates following the surgery. A randomized control trial by Gokcek et al, on application of SPG block in patients who underwent Septorhinoplasty concluded excellent analgesic effects of SPG block in early postoperative period.[9] A recent meta-analysis by Wang Ping on revealed reduced blood loss and additional benefits of reduced postoperative pain scores after bilateral SPG block in patients undergoing endoscopic sinus surgeries.[14] Ekici NY, Alagoz S in their randomised control trial (RCT) concluded that endoscopically performed SPGB with bupivacaine is a safe and effective method to reduce pain after septoplasty, and it is a cost-effective alternative to high doses of analgesics.[15] Degirmenci et al. conducted a retrospective analysis of a clinical trial and concluded that Preoperatively performed SPGB is an effective option to reduce postoperative pain and the need for rescue analgesics in patients undergoing Septorhinoplasty.[16] Another RCT by Nabil A Sarhan et al, using bilateral SPGB in FESS under GA has proved to be of great importance in reducing the heart rate, arterial blood pressure, bleeding, operation time, and VAS in the studied groups. Also, bupivacaine 0.5% is significantly reducing the analgesics usage.[17] A study by Ahmad K Abubaker et al, on endoscopically applied SPG injection with lidocaine at the end of surgery is a safe and effective technique in reducing early PONV, VAS scores in endoscopic sinus surgery patients.[18] A study by Marhofer et al on ultrasound guidance in regional anaesthetic technique greatly emphasized on ultrasound guidance enabling the anaesthesiologists to secure an accurate needle position, to monitor the distribution of the local anaesthetic in real time, also the safety profile as the added advantage over conventional guidance techniques.[19] Though an old but very much relevant study by J N Peterson et al. confirmed that sphenopalatine ganglion (SPG) block is a safe, easy method for the control of both acute or chronic pain of musculoskeletal, vascular or neurogenic pain.[20] In this present study, we also noted the safety profile ultrasound guidance, ease of performing and effectiveness of SPG block in postoperative period in reducing VAS scores with excellent analgesia upto 48 hours, reduced need for analgesics, minimal PONV, headache and others postoperative complications who received bilateral SPGB. We are delighted to say there were no postoperative complications & side effects related to block or drugs used in the interventional group.
Conclusion
We conclude bilateral USG-guided SPGB is very effective in controlling postoperative pain following FESS and reconstructive nasal surgeries. It provides sustained postoperative analgesia in FESS & nasal reconstructive surgeries and also superior in terms of quality & duration of analgesia when compared to sole analgesics like Fentanyl. Also, USG-guided bilateral SPGB is a safe procedure as it helps in visualizing vascular structures, spread of local anaesthetic in real time which minimizes the potential of inadvertent needle puncture and intravascular injection.
Sources of Funding and Conflicts of Interest
None.
References
- J Li, A Szabova. Ultrasound-Guided Nerve Blocks in the Head and Neck for Chronic Pain Management: The Anatomy, Sono anatomy, and Procedure. Pain Physician 2021. [Google Scholar]
- A Nader, H Schittek, MC Kendall. Lateral pterygoid muscle and maxillary artery are key anatomical landmarks for ultrasound-guided trigeminal nerve block. Anesthesiology 2013. [Google Scholar]
- L Beauregard, A Pomp, M Choinere. Severity and impact of pain after day-surgery. Can J Anaesth 1998. [Google Scholar]
- AL Russell. Sphenopalatine block--the cheapest technique in the management of chronic pain. Clin J Pain 1991. [Google Scholar]
- ON Aydin, S Başak, F Ünal. Functional endoscopic sinus surgery under sphenopalatine block or general anaesthesia: Effects on postoperative pain. Agri 2002. [Google Scholar]
- S Waxman. . Correlative neuroanatomy 1996. [Google Scholar]
- YT Sung, JS Wu. The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement. Behav Res Methods 2018. [Google Scholar]
- RE Windsor, S Jahnke. Sphenopalatine ganglion blockade: a review and proposed modification of the transnasal technique. Pain Physician 2004. [Google Scholar]
- E Gökçek, G Kozan. Postoperative effects of bilateral sphenopalatine ganglion blockade in septorhinoplasty operations; double-blind randomized clinical trial. Braz J Otorhinolaryngol 2024. [Google Scholar]
- JH Hwang, CM Liu, TC Liu, MC Hsu. Sphenopalatine ganglion block before removal of nasal packing. Laryngoscope 2003. [Google Scholar]
- M Friedman, TK Venkatesan, D Lang, DD Caldarelli. Bupivacaine for postoperative analgesia following endoscopic sinus surgery. Laryngoscope 1996. [Google Scholar]
- E Kesimci, L Öztürk, S Bercin, M Kırış, A Eldem, O Kanbak. Role of sphenopalatine ganglion block for postoperative analgesia after functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol 2012. [Google Scholar]
- S Demaria, S Govindaraj, N Chinosorvatana, S Kang, AI Levine. Bilateral sphenopalatine ganglion blockade improves postoperative analgesia after endoscopic sinus surgery. Am J Rhinol Allergy 2012. [Google Scholar]
- P Wang. The efficacy of sphenopalatine ganglion block for pain management after endoscopic sinus surgery: a meta-analysis of randomized controlled studies. Eur Arch Otorhinolaryngol 2021. [Google Scholar]
- NY Ekici, S Alagöz. The effectiveness of endoscopic sphenopalatine ganglion block in management of postoperative pain after septal surgery. Int Forum Allergy Rhinol 2019. [Google Scholar]
- N Degirmenci, A Ozdem, H Uysal, P Sen, E Senturk, O Ozturan. The Effect of Sphenopalatine Ganglion Block on the Postoperative Pain in Patients Undergoing Septorhinoplasty. Ann Otol Rhinol Laryngol 2020. [Google Scholar]
- NA Sarhan, MA Fathalla, MH Alahmer, ME Mohamed, MM Khalifa, . Effects of bilateral sphenopalatine ganglion block in functional endoscopic sinus surgery under general anesthesia. Al Azhar Med J 2020. [Google Scholar]
- AK Abubaker, MA Al-Qudah. The role of endoscopic sphenopalatine ganglion block on nausea and vomiting after sinus surgery. Am J Rhinol Allergy 2018. [Google Scholar]
- P Marhofer, M Greher, S Kapral. Ultrasound guidance in regional anaesthesia. Br J Anaesth 2005. [Google Scholar]
- JN Peterson, J Schames, M Schames, E King. Sphenopalatine ganglion block: a safe and easy method for the management of orofacial pain. Cranio 1995. [Google Scholar]
