Introduction
Thoracic segmental spinal anaesthesia is a type of regional anaesthesia that can be used as an alternative to general anesthesia for cases such as laparoscopic surgeries, and can be used mainly in patients who are considered at high risk if they undergo general anaesthesia.1 Since the spinal cord terminates at the level of L1, performing spinal anaesthesia above the lumbar level, which means at the thoracic level, the chances of spinal cord getting injured by the spinal needle may be there.2 The thoracic spinal canal anatomy has been studied by magnetic resonance imaging (MRI) in many of the studies recently. In a recent study which included 300 patients, there was no neurological sequelae when they performed spinal anaesthesia at the thoracic level and the incidence of paresthesia experienced in the patients who underwent thoracic spinal anaesthesia was same as those who received lumbar spinal anaesthesia.3 The spinal anaesthesia has been found to be associated with less emesis, less postoperative pain, postoperative stay is relatively shorter, and patient satisfaction is better, and the overall safety is more, in some minor laparoscopic procedures.4
Thoracic segmental spinal anesthesia can be specifically used for patients undergoing surgeries with major medical problems where the risk of giving general anaesthesia is greater. Even if general anesthesia is considered the standard for many of the surgical procedures, few drawbacks are there , which includes side effects of the anaesthetic agents, prolonged recovery after surgery, and the need for post-operative pain control. Nowadays in several common surgeries like laparoscopic cholecystectomies, breast cancer lumpectomies and abdominal cancer surgeries there is greater attention towards the use of thoracic spinal anaesthesia.1
So in the day to day practice there is can be an increase in the use of thoracic spinal anaesthesia in the future. There are lots of advantages of giving the spinal anaesthetic in only in the required region, so that the blockade occurs only in few specific segments of the body. There is no caudal spread of the drug therefore there is no anaesthetic effect in the lower extremities, which is an advantage to the patients. In thoracic spinal anaesthesia there is no venodilation in major portions of the body and also there will be compensation to adverse changes in blood pressure. In the section of the spinal cord there is very specific blockade to only certain nerve functions. It also has an advantage of requiring low dose of anaesthetic agent. When compared with general anesthesia there is greater muscle relaxation and there is no central or peripheral depression of respiration and circulation in thoracic spinal anesthesia. There is also an added advantage that there is no need for any other mode of analgesia for managing post-operative pain. There is postoperative early ambulation because the patients can move their legs during surgery this results in more patient satisfaction with the procedure and decreased anxiety during the procedure.5
Figure 1
Saggital gradient echo study of the thoracic spine. The cord is enlarged from T9 to T12, outlined by high signal CSF
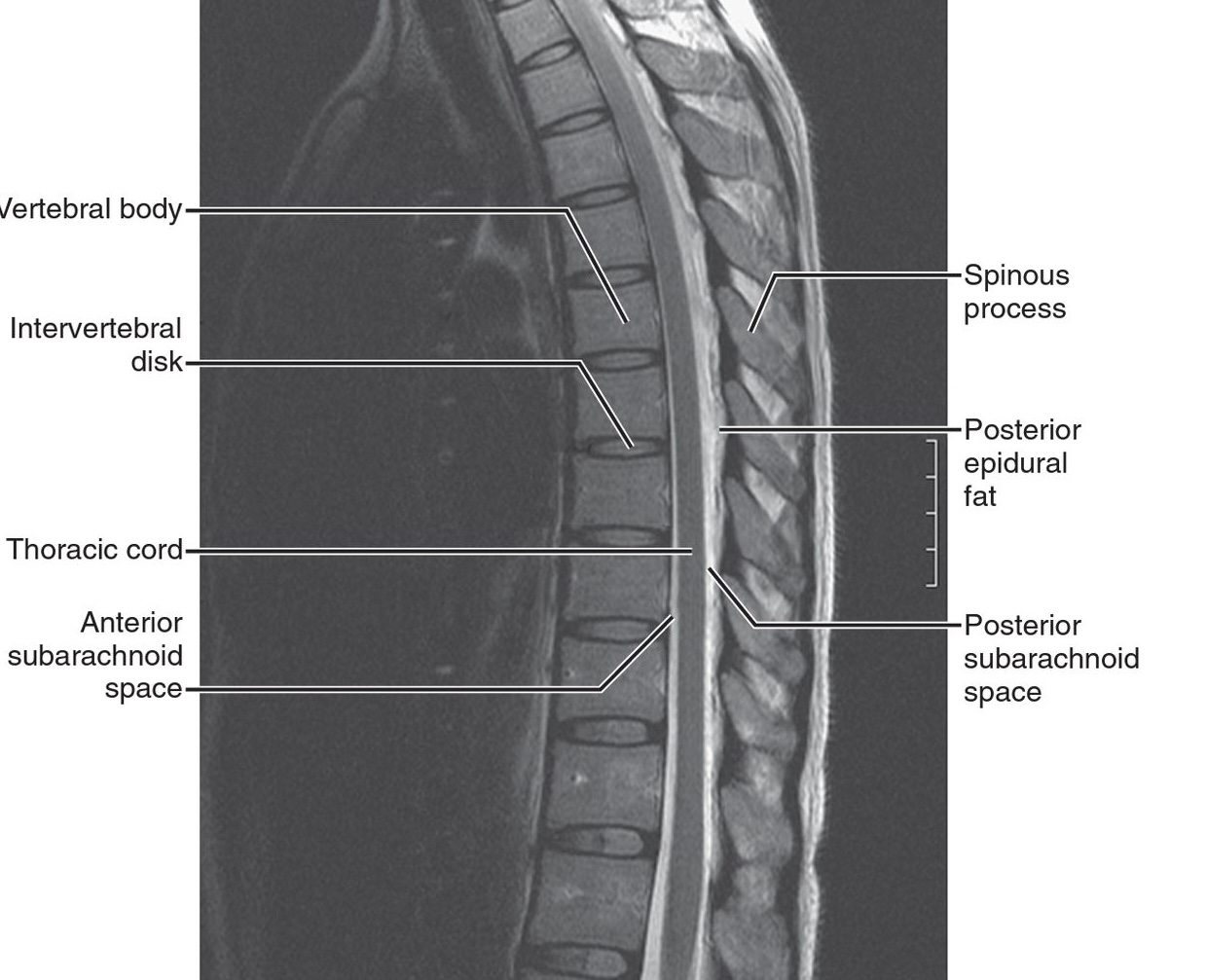
Figure 2
Saggital T1 MRI of thoracic spine. There is more cerebrospinal fluid (CSF) posteriorly in the thoracic area
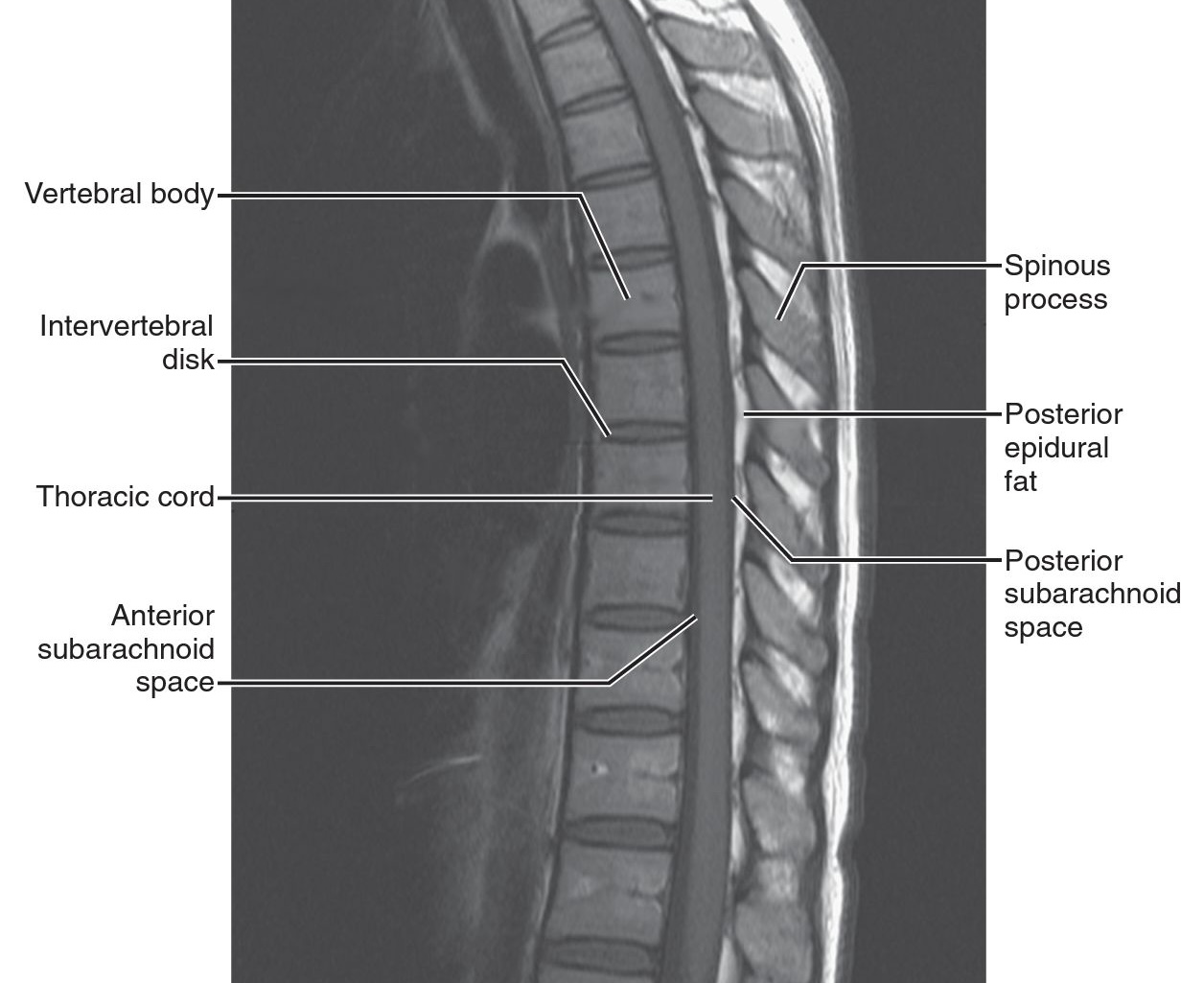
Table 1
Demographic characteristics of enrolled patients with their ASA (American society of Anaesthesiologists) grades
Case Series
We hereby report the use of thoracic segmental spinal Anesthesia in 14 patients in which few who underwent 10 laparoscopic surgeries among which 6 laparoscopic cholecystectomies, 2 laparoscopic appendicetomy and 2 diagnostic laparoscopies and 4 open upper abdominal surgeries (Table 2). All patients were explained about the procedure one day prior surgery during pre-anaesthetic checkup. Informed written consent was taken on day of surgery. All were explained about the effect of the procedure and also the possibility of conversion into general anesthesia if they were unsatisfied with spinal anaesthesia at any time during the procedure.
On the day of surgery Informed written consent was taken and other routine procedures like intravenous line placement and antibiotic prophylaxis given. In the operating room monitors like non-invasive BP, ECG and pulse oximeter were attached. All patients were given supplemental oxygen via a nasal cannula at a rate of 3 L min−1. Fentanyl (1 μg.kg−1) and midazolam (1 mg) was given after spinal anesthesia. With the patient in left lateral decubitus or sitting, we performed a puncture of the T9-T10 subarachanoid space through a median or paramedian with a 23 G Quincke needle (Figure 3). Free flow of CSF confirmed the position of the needle into the subarachnoid space. Injection isobaric Levobupivacaine 0.5% 2cc with dexmedetomidine 5 mcg was used for spinal anesthesia. After the spinal injection, the patients were placed in a supine position, The T4 dermatome level (tested by pinprick at 1-minute intervals) was targeted for the spinal block.
Among 14 patients 2 developed hypotension which was treated with mephenteramine, 6 patients developed shoulder tip pain which was treated with midazolam(1mg IV) and fentanyl(50mcg IV) in 5 patients, 1 required conversion into general anaesthesia (Table 4). Postoperatively patients dermatomal level was checked (Table 3), and duration of motor and sensory blockade were observed and postoperative complications like vomiting, urinary retention were followed up and treated accordingly. All patients were followed up for 24 hours for any neurological sequelae. There was no residual neurological sequelae in any of the patients.
Table 3
Level of sensory and motor blockage (T-Thoracic, L-Lumbar)
Discussion
There is greater risk of injuring the spinal cord if spinal anaesthesia is given above L1. The anatomy of the thoracic spinal canal with magnetic resonance imaging (MRI) in 50 patients were studied and concluded that there is low incidence of neurologic complications during thoracic segmental neuraxial anaesthesia.3 The depth of the posterior subarachnoid space at the mid-thoracic levels is greater than the depth at lumbar and upper thoracic levels. This indicates that we can give anaethetic drug intrathecally avoiding spinal cord contact in the thoracic region.6 Some hemodynamic changes occur even in thoracic segmental spinal anaesthesia but these changes are comparatively less than lumbar spinal anaesthesia because here we used small amount of drug and due to which dilution concentration of drug decreases and therefore chances of hemodynamic changes are less.7, 8
There are certain high risk cases where the chances of morbidity mortality are high and the need for post-operative ventilator support. In such cases this technique can be used safely. This technique has many advantages like Post-operative analgesia, which reduces the use of opioid for post-operative pain reducing their side effects, maintain spontaneous breathing , and the advantage of remaining conscious throughout the procedure decreases the post-operative cognitive dysfunction. There is earlier recovery of gastric motility and better post-operative pain control. As there is no need for post-operative ventilator for patient the duration of hospital stay can be decreased, unnecessary sedation or paralysis for ventilator, and burden of cost to patient is decreased.3, 9, 10 Neuraxial anaesthesia has the advantage of inhibiting the neuro endocrine stress response and since there is no pain post-operatively the need for opioid analgesia is decreased.5



