Introduction
The lower leg surgeries (Below knee) involving fractures of distal tibia, ankle surgeries, lower limb amputation, debridement, PVD surgeries are very common. When these patients are associated with co-morbid cardio-respiratory problems then it becomes challenge for anaesthesiologists to maintain homeostasis with good surgical anesthesia. Choice of anesthesia in such cases may be either general anesthesia or regional anesthesia, (specifically spinal anesthesia and epidural anesthesia.)1 Patient with associated co-existing disease may have to face many unwanted effect of either spinal or general anesthesia during the course of surgery.
Now question arises to reduce such undesirable effects and the choice of anesthesia technique to do so. If we choose to give spinal anesthesia, limiting the block to lower dermatomal level and avoiding the occurrence of hypotension is important because fluid loading and vasopressor administration may not be ideal methods to treat hypotension since end-stage renal disease and coronary artery occlusive disease are common in these patients. Zeinab I. EL Hossary suggested single shot unilateral spinal anesthesia can be utilized for such operative procedures. Ayukut Urfalioglu suggested another alternative technique in a form of peripheral nerve blocks by blocking the pain pathways at multiple levels which present a clear advantage of stable haemodynamics in this clinical setting.1, 2, 3
Distal sciatic nerve block (popliteal block) is a very clinically valuable technique that results in anesthesia of calf, tibia, fibula, ankle and foot. The sciatic nerve at popliteal fossa can be approached from either posterior approach described by Duane Keith Eonie or the lateral approach described by Jerry Vloka. Popliteal sciatic block performed with long acting anesthetic such as bupivacaine can provide 10-12hr of analgesia after foot surgery. When used as a sole technique, it can provide excellent anesthesia and post-operative analgesia, allows usage of calf tourniquet and avoids disadvantage of neuraxial block. Study by David H. McLeod found that lateral approached popliteal block with 0.5% bupivacaine provided analgesia for 18hr compared to ankle block which lasted only 6.2hr.4
For intraoperative anesthesia or postoperative pain control, a popliteal sciatic nerve block is an effective method when the surgery does not involve the medial side of the foot and ankle. When the surgery involves the medial side of the lower tibia, foot and ankle, the saphenous nerve should be blocked in addition, to ensure proper anesthesia or analgesia.
Adductor canal block (Saphenous nerve block) is novel technique in combination with popliteal sciatic block to provide complete anesthesia of lower leg for various surgical procedures. The saphenous nerve is purely sensory nerve; it innervates the medial, anteromedial and posteromedial lower leg, ankle and foot. Adductor canal contains Nerve to vastus medalis, saphenous nerve and branches from the obturator nerve in distal part. So, adductor canal block is often used to block pain from medial leg, ankle and knee. Michael B. Canales suggested that a combination of the popliteal sciatic nerve block and saphenous nerve block has shown to be efficacious in patient satisfaction and pain relief for 24 hours.5 So, after reviewing various references we decided to evaluate this novel approach of adductor canal block combined with popliteal block in our institute.
Materials and Methods
The study was conducted in department of Anaesthesiology, Government Medical College and SSG Hospital, after taking permission from Institutional Ethical Committee for Human Research. It was a prospective randomized case controlled study involving 60 patients. It is time bound study. As per hospital record approximately 5 patients were expected to be operated for the aforementionedprocedures per month hencein 12 months approximately 60 patients were to be included as a part of study. So in each group 30 cases will be studied. Randomization was done by envelope method.
Patient of either sex of age 18 to 70 year, ASA grading I, II or III, Malampatti Grade I and II, duration of surgery less than 2hours, posted for lower leg surgeries (e.g. orthopedic surgeries like foot, ankle, distal tibia, PVD surgeries like tarsal and metatarsal amputations and debridement etc.), able to give written & informed consent and understand VAS regarding assessment of pain were included in study.
After pre-anesthetic evaluation patients meeting the inclusion criteria were selected for study. Written informed consent was taken. After all preoperative preparation patients were randomly allocated into two groups by sealed envelope method. Patients in Group P (n=30) were given Popliteal Sciatic Block plus Adductor Canal Block (Drug to be used:- 0.5% Bupivacaine 20 ml + 2% Lignocaine 20ml with 5mcg/ml 1:200000 Adrenaline and Soda bicarbonate 2ml). Patients in Group S (n=30) were given Unilateral Spinal Anesthesia with Inj. Bupivacaine Heavy 0.5% 1ml, patient kept positioned laterl with operating side on lower side for 10 minute.
For popliteal sciatic block patient was positioned supine with hip flexed at 30ﹾ by putting pillow below the heel and knee fully extended. A 22-gauge 8-inch insulated needle attached to the negative electrode of the PNS, inserted approximately 10cm above the most prominent part of lateral femoral condyle in the groove between biceps femoris and the vastus lateralis muscle. The initial current strength was set at 3mA with 2Hz frequency and 0.1ms duration. Amplitude was decreased up to 0.5 mA while seeking maximal planter flexion contraction. If the aspiration for blood was negative, 20ml local anesthetic was injected.
For adductor canal block patient was positioned supine with pillow placed under knee and thigh. A 22-gauge 8-inch insulated needle attached to the negative electrode of the PNS, was inserted approximately 4 finger breadth (7 -8 cm) above the adductor tubercle on the medical condyle of the femur in the groove between Sartorius and the vastus medialis muscle. The initial current strength was set at 3mA with 2Hz frequency and 0.1ms duration. Amplitude was decreased up to 0.5 mA while seeking maximal vastus medialis contraction. If the aspiration for blood was negative, 20ml local anesthetic was injected.
Preoperative vitals were recorded for baseline. Patient was allowed for Surgery after assessing sensory and motor blockade. Intra-Operatively patient were monitored for vital parameters (pulse, Blood pressure, Spo2) sensory block, motor block. Post operatively patient were monitored for vital parameters (pulse, blood pressure, spo2) duration of sensory block and motor block, total duration of analgesia, total requirement of rescue analgesia required in 24 hours and complications if any for 24 hours.
All the observed parameters were noted in a master chart and these were then subjected to statistical analysis using MedCalc Software 2020. The results were expressed as Mean ± SD. T-test and Chi Square test were used for parametric and non-parametric variables respectively.
Result
It was time bound study. So in each group 30 cases will be studied. Randomization was done by envelope method. Study was conducted in Department of Anaesthesiology, Government Medical College and SSG Hospital, Vadodara during a period of October 2019 to October 2020, after taking permission from Institutional Ethical Committee for Human Research.
Table 1
Patient‘s age, sex and weight in both group
|
Parameters |
Group P Mean ± SD |
Group S Mean ± SD |
P value |
|
Age(years) |
42.43±12.75 |
41.76± 11.74 |
>0.05 |
|
Sex(M:F) |
20 :10 |
22:8 |
>0.05 |
|
Weight |
63.4±7.78 |
62.43±6.50 |
>0.05 |
After giving block patients were observed for vital parameters like Pulse rate, Blood Pressure and Spo2, immediately after block, at 5 minute interval for first 10 minute, at 10minute interval for 1 hour and at 20 minute interval for next hour.
Intra operatively evaluation of block was done by observing number of patients requiring additional anesthesia like 1) Patient not required any additional anesthesia 2) Patient given local anesthetic 3) Patient given IV sedation (Inj.Midazolam/ Inj.Fentanyl) 4) Patient given both local anesthetic and IV sedation 5) Patient given general anesthesia.
Post operatively patients was observed every 2 hourly for 24 hour for duration of analgesia using VAS score, duration of sensory and Motor Block, demand for rescue analgesia in 24 hrs, vital parameters and any postoperative complication.
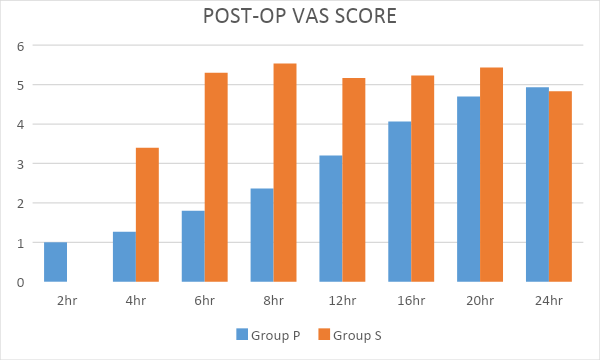
Both the groups were comparable to each other with respect to demographic parameters like age, sex, weight & type of surgery (p>0.05). The mean onset time for both Sensory & Motor Block was significantly higher in Group P (Sensory block: 112±50.4052 sec, Motor block:188±72.1779 sec) as compared to Group S (Sensory block:14±3.9740 sec Motor block: 26.26±4.9753 sec) (P < 0.0001). Mean time to achieve both complete sensory block & complete motor block was significantly higher in Group P (Sensory block: 928±151.7347 sec, Motor block: 1078±105.0911 sec) as compared to Group S (Sensory block: 44.16±8.7733 sec, Motor block :- 89.06±12.9240 sec). (P < 0.0001). Mean Intra-operative Pulse Rate, mean arterial pressure & Spo2 was comparable in both the Groups intraoperatively (P > 0.05). Mean Post-Operative Pulse Rate, Spo2 & Mean arterial pressure were comparable in both the Groups post-operatively (P > 0.05). We have included ASA I, II & III patients as well as no major blood loss was observed intraoperatively, so haemodynamic stability was maintained in all patients in our study. Mean Duration of Sensory and Motor block was 634±231.9423 minute and 394±158.88 minute respectively in Group P as compared to 203.4±35.7699 minute and 130±32.6010 minute respectively in Group S, which is statistically highly significant (p <0.0001). Mean time for first demand of rescue analgesia was 954 ± 321.5115 minute in Group P as compared to 363 ± 75.2994 Minute in Group S, which is statistically very highly significant (p <0.0001). Mean requirement of rescue analgesia was 130 ± 59.59mg inj.tramadol in Group P as compared to 216.66 ± 37.90mg inj.tramadol in Group S, which is statistically very highly significant (p <0.0001). Post-operative VAS score increased rapidly in Group S as compared to Group P where VAS seen to be increasing gradually. Out of 30 patients of Group P 18 patients did not require any additional anesthesia while 6 patients required injection of local anesthetic by surgeon, 4 patients required injection of local anesthesia plus IV sedation and 2 patients were given additional IV sedation only, while none of the patient of Group S required any additional anesthesia, suggest that intra operative additional anesthesia requirement was more in Group P as compared to Group S.
Discussion
Mean time to achieve both complete sensory block & complete motor block was significantly higher in Group P (Sensory block: 928±151.7347 sec, Motor block: 1078±105.0911 sec) as compared to Group S (Sensory block: 44.16±8.7733 sec, Motor block:-89.06±12.9240 sec). (P < 0.0001)
It has been universally accepted worldwide that time to achieve sensory and motor block onset as well as complete block is faster in spinal anesthesia as compared to peripheral nerve blocks. We also found similar result in our study. Prerana Jogdand et al. compared psoas compartment block and sciatic nerve block with that of spinal block anesthesia also observed delay in onset of sensory and motor blockade in block group (psoas compartment block and sciatic nerve block) as compared with the spinal anesthesia group.(Block group:- Sensory block - 5.4 ± 1.28 min, Motor block - 15.3 ± 2.32min ; Spinal group :- Sensory block - 3.03 ± 0.69min, Motor block - 7.393 ± 0.34min) Aykut Urfalioglu et al compared ankle block with spinal anesthesia & Zeinab i. El Hossary et al compared popliteal sciatic block with spinal anesthesia also observed similar results.3, 6, 7
Aykut Urfalioglu et al., noted in their study a fall in mean blood pressure at 5th and 15th minute after block in spinal group as compared to block group which was in consensus with our study. They have used 2ml 0.5% Bupivacain for spinal anesthesia while we have used 1ml 0.5% bupivacaine in our study. Prerana Jogdand et al., too, found significant fall in mean blood pressure in spinal group as compared to block group who have used 3ml 0.5% bupivacaine for spinal anesthesia. Zeinab i. El Hossary et al., however, found no significant difference between the mean values of the heart rate (b/m), systolic (SBP) and diastolic (DBP) blood pressure readings in the block group as well as the spinal groups at various times of measurements.3, 6, 7
Out of 30 patients of group P 12 patients required additional anesthesia while none of the patients of group S required any additional anesthesia, suggesting that intra operative additional anesthesia requirement was more in Group P as compared to Group S. Thus, in terms of quality of anaesthesia spinal anesthesia provides dense block as compared to peripheral nerve block. Many other studies also noticed similar difference between spinal anesthesia and peripheral nerve block.1, 3, 6, 8
In 12 cases out of 30 cases we used additional anesthesia in block group, although we found that combined adductor canal block plus popliteal sciatic block provides effective anesthesia to conduct surgery in high risk patient where spinal anesthesia is contra-indicated.
Mean duration of sensory and Motor block was 634±231.9423 minute and 394±158.88 minute respectively in Group P as compared to 203.4±35.7699 minute and 130±32.6010 minute respectively in Group S in our study, which is statistically highly significant. (p <0.0001) This was in correlation with the study conducted by Prerana Jogdand et al., who also reported the prolonged mean duration of sensory and motor block in block group (Sensory block: 8.1 ± 0.96hr, Motor block: 2.3 ± 0.58hr) as compared with that of spinal group (Sensory block: 5.45 ± 1.0hr, Motor block: 2.81± 0.77hr). Zeinab i. El Hossary et al., Ayukut Urfalioglu et al. and Hyun-Jun Jeon et al. also reported the same results.3, 6, 7, 9
Mean duration of sensory and motor block was 634±231.9423 minute and 394±158.88 minute respectively in Group P as compared to 203.4±35.7699 minute and 130±32.6010 minute respectively in Group S in our study, which is statistically highly significant. (p <0.0001) This was in correlation with the study conducted by Prerana Jogdand et al., who also reported the prolonged mean duration of sensory and motor block in block group (Sensory block: 8.1 ± 0.96hr, Motor block: 2.3 ± 0.58hr) as compared with that of spinal group (Sensory block: 5.45 ± 1.0hr, Motor block: 2.81± 0.77hr). Zeinab i. El Hossary et al, Ayukut Urfalioglu et al. and Hyun-Jun Jeon et al. also reported the same results.3, 6, 7, 9
Chart shows mean post-operative VAS score at 2, 4, 6, 8, 12, 16, 20 & 24 Hour intervals. From chart, we observed that VAS score increased rapidly in Group S whereas in Group P it was increasing gradually with statistically significant difference initially up to 12 hours. However, no significant difference was found at 24-hour post-operatively. In our study we have not used any adjuvant but by using it we can increase duration of analgesia further. Ayukut Urfalioglu et al, compared ankle block with spinal anesthesia using 2ml 0.5% bupivacaine, noted significant lower value of VAS score at 6th, 12th and 24th postoperative hours in block group as compared to spinal anesthesia. Zeinab I. El Hossary et al., compared popliteal sciatic nerve block with spinal anesthesia using 1ml bupivacaine with adjuvant, either 25mcg fentanyl or 2.5mg midazolam, also noted in their study significantly lower postoperative VAS values at 6 hours in block group as compared to spinal groups, without any significant difference at other time intervals.3, 7
The common side effects of peripheral nerve blocks are incomplete block, direct nerve injury, hematoma, infection, and the risk of intravenous administration of local anesthetic. There were no side effects found in both the group in our study, but Hajek et al., reported superficial peroneal nerve and sural nerve injury in three patients (1.9 1%) out of 157 patients who were anesthetized with continuous popliteal nerve block. Prerna Jogdand et al. and Zeinab i. El Hossary et al. observed no major complications in either of the two groups which was in accordance with our study. Despite the small chance of complications, all patients were informed of occurrence of such side effects.6, 7, 10
Limitations of the Study
Limitations of our study are that we have included only ASA I, II & III cases in our study, however block can be better alternative in high risk cases where spinal anesthesia is relatively contraindicated in patients with comorbidities such as uncompanseted ischeimic and valvular heart disease in emergency settings. We also have not used adjuvants and ultrasonography machine for performance of the blocks specially in case of adductor canal block. By using adjuvant, we can prolong the duration of analgesia. We have performed block using peripheral nerve stimulator. However, we agree that in modern day anesthesia ultrasonography increases success rate of adductor canal block and popliteal sciatic nerve block.
As we are using peripheral nerve stimulator, it is a skill based instrument and blind procedure. So, failure rate can be decreased by using ultrasound guided block.