Introduction
In cardiovascular anaesthesia, monitoring of neurological function is a huge challenge. Cerebral oximetry using near-infrared spectroscopy (NIRS) is a noninvasive, continuous, and real-time measure of cortical oxygenation that can provide an early warning of decreased oxygen delivery. This has the potential to institute measures to reverse cerebral hypoperfusion in cardiac surgery. This review talks about how cerebral oximetry is used to find cardiovascular disease in adults and children when NIRS is used.
Maintaining acceptable oxygen delivery to tissues and organs, especially the brain, is a fundamental requirement of anaesthetic management. The perils of cerebral hypoxia and reduced oxygen delivery to the central nervous system are well documented. However, priority is given to maintenance of haemodynamic stability during anaesthesia and less attention is paid to cerebral monitoring under anaesthesia.1
By monitoring blood oxygen saturation in the cerebral tissue immediately underneath its sensors, cerebral oximetry (Cox) helps to identify diminished blood flow to the brain. Cox generates a parameter called ‘regional cerebral oxygen saturation’ (rSo2). A decrease in this value indicates compromised tissue perfusion and increased ischemic risk, and this provides the physician an opportunity to prevent or minimise ischemic complications. Regional cerebral oxygen saturation (rSO2) can be measured in real-time, continuously, and non-invasively using near-infrared spectroscopy (NIRS), and this method is increasingly being used intraoperatively.2
It has been thought of as a surrogate for cerebral blood flow and therefore as a viable technique to diagnose cerebral hypoperfusion by measuring rSO2 in a representative volume of cortical brain tissue (and assuming sustained metabolic suppression of the brain under anaesthetic settings).2, 3 It provides a regional and not systemic measurement. Traditional assessing measures such as mean arterial pressure (MAP), peripheral capillary oxygen saturation (SpO2), arterial blood gases (ABG), and lactates, which may be time-delayed or reflect a whole-body status, often provide an earlier and more significant warning than rSO2.4, 5 For patients having certain kinds of cardiovascular surgery, precise NIRS oxygenation monitoring is essential for preventing perioperative brain injury. We conducted a literature review to assess the intraoperative use of Cox and investigate perioperative cerebral damage in cardiovascular surgery. To identify which group of patients would be at a higher risk of neurological ischemia insult, cerebral oximetry, specifically assessing the baseline rSo2 values and their variations throughout the conduct of cardiac surgical cases, may be helpful.
Discussion
Cerebral autoregulation, role of cerebral oximetry and cox index
The capacity of blood vessels to maintain relatively constant cerebral blood flow (CBF) throughout a broad range of systemic blood pressure levels is known as cerebral autoregulation. This is accomplished by means of sophisticated myogenic, neurogenic, and metabolic processes. Vascular conductance and arterial blood pressure affect the CBF. A homeostatic mechanism called cerebral autoregulation controls and keeps cerebral blood flow (CBF) steady throughout a wide range of blood pressures. This homeostatic process makes sure that when MAP or CPP rises, resistance rises and the tiny cerebral arteries narrow (vasoconstriction). Individuals who are at risk for perioperative neurocognitive problems may be identified by identifying periods of cerebral desaturation by the use of near-infrared spectroscopy to monitor cerebral oxygenation. There is a lack of information on the effectiveness of near-infrared spectroscopy monitoring during profound hypothermic circulatory arrest. The current research presents data on the use of a commercially available near-infrared spectroscopy monitor during profound hypothermic circulatory arrest in paediatric patients having congenital heart surgery. The cohort included 8 patients, 2 weeks to 6 months of age, who required deep hypothermic circulatory arrest for repair of congenital heart disease. The baseline cerebral oxygenation was 63 ± 11% and increased to 88 ± 7% after 15 min of cooling to a nasopharyngeal temperature of 17-18°C on cardiopulmonary bypass. In 5 of 8 patients, the cerebral oxygenation value had achieved its peak value (either ≥ 90% or no change during the last 2-3 min of cooling on cardiopulmonary bypass). For the other 3 patients, an extra period of cardiac bypass was necessary to reach the highest possible level of brain oxygenation. Deep hypothermic circulatory arrest lasted anywhere between 36 and 61 minutes (43.4 8 min). Following the start of profound hypothermic circulatory arrest, brain oxygenation gradually declined to a low value of 53 ± 11%. The biggest drop (9 ± 3%) happened in the first five minutes after profound hypothermic circulatory stoppage. The brain oxygenation value dropped by 0.9% per minute on average during the profound hypothermic circulatory arrest (with a range of 0.5 to 1.6% fall per minute). Monitoring using near-infrared spectroscopy during cardiopulmonary bypass, cooling, and profound hypothermic circulatory arrest adhered to the clinically anticipated parameters. This monitoring might be helpful in identifying individuals who, after 15 minutes of cooling on cardiopulmonary bypass, have not reached the greatest feasible cerebral oxygenation value. Future studies are needed to define the cerebraloxy genation value at which neurological damage occurs and if interventions to correct the decreased cerebral oxygenation will improve perioperative outcomes.
Perioperative cerebral injury in adult cardiovascular surgery
Major outcomes of perioperative cerebral injury are classified as Type I (stroke and hypoxic encephalopathy) and Type II (new decline in logical function, confusion, nervousness, perplexity, memory decline, seizure without indication of focal injury), and postoperative cognitive dysfunction (POCD).6 In both Type I and Type II cerebral injuries, elderly patients are at a higher risk. The rate of perioperative stroke in patients going through cardiovascular surgery is much higher than in patients having non-cardiac surgery. The occurrence of stroke increases the perioperative mortality rate by six-to eight-fold.7, 8 Post-operative cognitive decline (POCD) is well-defined as cortical dysfunction characterized by impairments in speech, memory, attention, concentration, and executive function and is detected by neuropsychological examination after surgery. Postoperative delirium is associated with a higher long-term risk of death and POCD. This may be the downstream outcome of decreased cerebral perfusion pressure, cerebral autoregulation impairment, or other unknown hemodynamic indices.9 Emerging clinical evidence recommends that Cox can help clinicians monitor and manage cardiac surgery patients throughout the entire perioperative period with a view to avoiding unwelcome neurological sequelae. Preoperative baseline measurement of cerebral oxygen saturation may provide an extra measure for risk stratification before cardiac surgery. When it comes to forecasting death, these low rSo2 readings are almost as accurate as the EuroScore or Society of Thoracic Surgeons mortality risk scores.10, 11 A spike in operating mortality,10, 11 death at 30 days and 1 year, significant adverse events and complications,12 a longer time to extubation, 13 and post-operative delirium have all been associated with low rSo2 levels.14, 15
Cardiac surgery
The significance of monitoring and maintaining rSO2 during major surgery, particularly in high-risk patients, has been stressed in recent reviews. While Moerman and De Hert state that "the human brain is an astonishingly poorly monitored organ, considering its crucial significance," Murkin and Arango argue that "the right management of cerebral oxygenation should be one of the key objectives of all anaesthesia treatments".1
According to the 5th National Audit Project (NAP5) of the Royal College of Anesthetists and the Association of Anesthetists of Great Britain and Ireland in the United Kingdom,16 40,600 patients received cardiac surgery per year. Patients undergoing cardiac surgery are becoming older and have more pre-operative risk factors, with a mean EuroSCORE of 7.7 in 2013, about 25% higher than 10 years previously. With post-operative delirium occurring up to 48% of the time.17 AKI occurring at a rate of around 38% 18, and myocardial infarction occurring at a rate of up to 24%, the 1-year mortality rate after bypass surgery is about 5%.18 The topic of whether better monitoring of oxygen delivery (DO2) and its optimization may assist in supplying adequate oxygen to the tissues is still open given the high prevalence of documented end-organ harm. Cox has the ability to evaluate patterns in the oxygenation of cerebral tissue and might thus detect an imbalance between the supply and demand for oxygen in the brain. Additionally, continuous rSO2 monitoring has been shown to be helpful in non-invasively assessing cerebral autoregulation during cardiac surgery.19 Emboli, including air, atherosclerotic plaques, fat and platelet aggregates can form during cardiopulmonary bypass operations, cross clamping, unclamping of the aorta and other such mechanical maneuvers, and results in reduced blood flow in brain if they enter the cerebral circulation.20, 21 Long-term cerebral desaturation during on-pump CABG and valve replacement surgery has been associated with adverse and unsatisfactory postoperative patient outcomes, including neurological deficit and extended hospital stay.22, 23 Additionally, a prospective observational analysis of 1178 patients found that very low preoperative readings before heart surgery are associated with considerably increased postoperative morbidity and death in patients at high risk.12 It is well recognised that rSO2 desaturations, especially during aortic surgery, reveal CPB cannula malposition that is readily corrected. By using the rSo2 cerebral/somatic oximeter together with an interventional method to restore baseline cerebral oxygen saturation during heart surgery, many studies have demonstrated up to a 97% success rate in correcting cerebral desaturation occurrences.24, 25, 26, 27 Randomised, controlled trials have shown that postoperative outcomes such as postoperative cognitive failure,28 ICU length of stay, major organ disease, and mortality are improved by monitoring and intervention.24, 25, 26, 27, 28
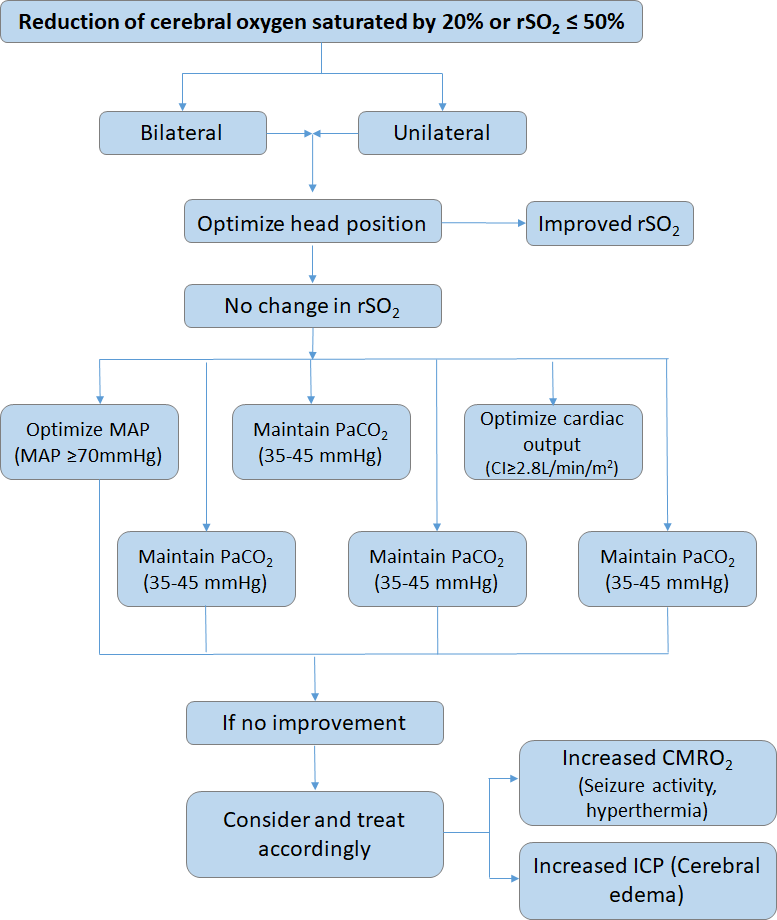
This hypothesized cerebral desaturation algorithm may help in the management of patients when the rSO2 value falls more than 20% from baseline or rSO2 is less than 50%.29
Additionally, two recent multi-centric trials with adequate power showed that 95–97% of patients may effectively normalise their rSO2 saturations after therapy. Desaturations were defined by Deschamps et al. as a rSO2 < 10% of the baseline in their study of 201 individuals.26 In a study of 235 adult patients by Subramanian et al., 50–75% of the patients had several desaturations, which were indicated by a decrease of more than 20%.27 Patients who received precise interventions had their hypotension treated in 29.8% of cases; their inhalational oxygen concentration increased in 15.6%, their cardiopulmonary bypass flow was normalised in 14.2% of cases, they received red blood cell transfusions in 13.8% of cases; their cardiopulmonary bypass "sweep speed" was decreased in 11.1% of cases; their anaesthesia was deepened in 10.7% of cases, their cardiopulmonary bypass cannula was adjusted in 8.0% of cases, and their head was realigned in 2.28, 29 The list above showed that at least one intervention was given to 10% of all patients. Denault and colleagues devised another treatment algorithm mentioned below based on improving cerebral oxygen delivery and intake to treat a decrease in rSo2 values Adapted from original by Denault and colleagues.30 Rajinder Singh Rawat reported that NIRS-based cerebral oximetry permits early detection of cerebral hypoxia and intervention to restore cerebral oxygenation. A decreased incidence of neurological injury is linked to this.31 Cardiopulmonary bypass (CPB) monitoring, as shown by Mohandas BS et al., may dramatically lower the risk of postoperative neurological deterioration.32 The combined use of BIS and NIRS in 40 patients undergoing coronary artery bypass grafting (CABG) was researched by Sandeep Kumar et al. They suggested using both BIS and NIRS to improve patient safety.33
Extended peri-operative rSvO2 desaturations have been demonstrated to be reliable indicators of poor clinical outcomes in cardiac surgery. When intraoperative treatment is proactive in reducing cerebral oxygen desaturation, brain and other major organ disorders are less prevalent. 34
The use of cerebral oximetry to define the limits of cerebral autoregulation is gaining popularity. The cerebral oximetry index, which evaluates autoregulation, is calculated by plotting brain oxygen saturation versus blood pressure (COx). The determination of limits of autoregulation in a given subject and the integration of this monitoring ability into daily anaesthetic management may allow clinicians to tailor blood pressure management to the individual patient’s needs and might prove to be a major step forward in terms of patient outcome. Advances in perioperative management will depend on understanding of the fact that goal-directed therapy with parameters being maintained within a particular range for all patients and refraining from assumptions and individualizing physiological targets. In the near future, real-time cerebral autoregulation monitoring will provide an opportunity to individualize blood pressure targets and may direct critical care management to the individual patient’s needs.35
Carotid endarterectomy (CEA)
Patients who have high-grade carotid artery stenosis36 and are at a higher risk of neurological complications should have a carotid endarterectomy (CEA). The adverse events described in the European Carotid Surgery Trial (ECST) studies36 and the North American Symptomatic Carotid Endarterectomy Trial Collaborators (NASCET)37 investigations included major stroke rates of 5.8% and 7.5% and death rates of 2.1 and 3.2%, respectively. When the internal carotid artery is clamped, hypoperfusion may cause a new stroke to occur or exacerbate existing damage from previous episodes. Therefore, maintaining suitable perfusion during the procedure is critical.
Because routine intraluminal shunt placement during CEA carries its own risk of intimal impairment or embolization,38, 39 selective shunting via a consistent monitoring procedure should ensure an ideal intraoperative approach and avoid unnecessary shunting. Electroencephalogram (EEG), stump pressure measurement (SP), or transcranial Doppler (TCD) monitoring are the most common ways to figure out if there is enough blood flow to both sides of the brain and if shunting is needed after carotid endarterectomy (CEA) under general anesthesia.
During extracranial carotid surgery, near-infrared refracted spectroscopy (NIRS) has been proposed as a simple, non-invasive, constant, real-time monitor.40 This review aims to determine which patients would benefit from such monitoring under general anaesthesia, either alone or in combination with other modalities, and what percentage drop in rSO2 from baseline, 2 minutes after clamping the carotid artery, can be safely tolerated without the risk of cerebral ischemia. Data from T. Mille et al.41 was similar to that referred to Samra et al.40 in conscious patients and stated that an rSo2 reduction of less than 20% from baseline indicated that use of a shunt was not necessary. However, the period of reduction in rSo2 was also an important predictor of brain ischemia. Thus, for accurate decision-making, the surgeon should delay until 2 min after clamping, the necessary time for autoregulation.41 Also, it was firmly stated that the relative change in rSo2 is a more dependable indicator of the ischemic threshold to establish the necessity for a shunt than an absolute number.41
NIRS also has a significant advantage over EEG and evoked potential monitoring, in that NIRS is not altered by anaesthetic drugs which decrease brain activity or neuromuscular transmission.41 When considering other aspects, such as the great easiness of use, the quickness of measurement, and the fact that NIRS offers a constant, real-time and non-invasive means for the monitoring of cerebral cortical oxygenation, the authors concluded that NIRS was a valuable means of monitoring hypoperfusion during CEA.41 NIRS is also superior to assessing blood flow by transcranial doppler (TCD), since the latter can’t be used in 15-20% of patients because of poor temporal windows. This finding is supported by a Korean study that shows that NIRS may control shunt utilisation more effectively than TCD, which is likely to reduce post-operative stroke or neurological sequelae.
In 2019, the mentioned flowchart was proposed by the Japanese Society of Cardiovascular Anesthesiologists (JSCVA) for hemodynamic management in CEA surgery,42 with a slight alteration of the algorithm developed by Zogogiannis and colleagues.43
They recommend that the surgeon consider implanting a shunt if patients with a MAP of 60 mmHg or above experience a 20% reduction of rSO2 from baseline or an absolute rSO2 value equal to or below 50%. NIRS oxygenation monitoring for several post-operative days is neither practical nor beneficial. However, the surgeon may consider maintaining NIRS oxygenation monitoring until the patient leaves the ICU.42
In research examining the prevalence of carotid artery stenosis in neurologically asymptomatic individuals receiving coronary artery bypass grafting for coronary artery disease, Taneja et al. employed NIRS and BIS.44
Aortic surgery
The aortic arch surgical repair process is still time-consuming and technically difficult, and it is also linked with high morbidity and death rates. These operations include prolonged cardiopulmonary bypass (CPB) periods, embolic risk, and stoppage of cerebral blood flow. Thus, neurologic and neuropsychologic sequelae occur more commonly with aortic arch surgery than with coronary and valvular cardiac surgery; stroke rates have been stated in the range of 6% to 13%,45 with neuropsychologic impairment being even more common.46
Deep hypothermic circulatory arrest (DHCA), antegrade cerebral perfusion (ACP), and retrograde cerebral perfusion (RCP) are the techniques for protecting the brain.42 The goal of DHCA is to keep the brain tissue safe by increasing its ischemic tolerance via hypothermia. DHCA alone is inadequate to ensure satisfactory cerebral safety during long surgery. Therefore, ACP has been introduced as an adjunct procedure for brain protection where an inflow cannula is inserted into the arch branch of interest.42 However, ACP may end with cerebral ischemia if the inflow cannula is not positioned properly. Clinically, near-infrared spectroscopy (NIRS) monitoring of brain tissue oxygenation during ACP has been employed among other approaches to boost safety and improve neurologic prognosis.47, 48, 49
In individuals with acute aortic dissection and thoracic aneurysm rupture, the risk of cerebral ischemia is relatively high. According to a 2013 annual report on thoracic and cardiovascular surgery in Japan, hospital death rates for burst aneurysms were 22.2% and 9.1%, respectively, for Stanford Type A acute aortic dissection. These high rates may be attributable to stenosis/occlusion of the arch branch by the thrombosed false lumen, and cardiac tamponade, myocardial ischemia, or heavy bleeding causing circulatory failure and subsequent cerebral ischemia.50
Notably, cerebral hypoperfusion in individuals with acute aortic dissection may elicit preoperative neurologic symptoms. The actual lumen of the right carotid artery may constrict in instances of acute Stanford Type A aortic dissection,51 and the observation of a difference in rS02 between the right and left sides of the forehead may prompt remedial treatments, Thus restoring perfusion to the right hemisphere.42 The emergence of new side-to-side asymmetry in rSO2 post aortic surgery suggests a high likelihood of unilateral perfusion problems. The surgeon should conduct appropriate interventions as soon as possible.42 NIRS oxygenation monitoring assists the surgeon in making an educated choice about moving from unilateral to bilateral ACP during aortic arch surgery. Changes in NIRS oxygenation data, such as a drop of 65-80% of baseline and the beginning of a difference between the left and right hemisphere values, should lead the surgeon to investigate the reason of the change and, if required, take appropriate corrective procedures. The surgeon should consider the catheter's location, the rate of blood flow, the patient's body temperature, and other clinical data.42
Our understanding of the utility of NIRS in deep hypothermic circulatory arrest (DHCA) during aortic surgery: Cerebral desaturation was connected to stroke in 8 patients and delirium in 1 in a retrospective examination of 40 patients undergoing aortic surgery at a tertiary care centre (unpublished data). The results of this research are in favour of using cerebral oximetry in patients having aortic surgery when their circulatory systems are profoundly hypothermic.
Role of NIRS in DHCA
In recent years, the feasibility of near-infrared spectroscopy to continuously assess cerebral autoregulation has gained increasing interest. The cerebral oximetry index is a measure of autoregulation that doctors may create by graphing brain oxygen saturation against blood pressure (COx). If this monitoring capability is successfully incorporated into routine critical care, doctors may be able to customise blood pressure treatment to each patient's needs, which might significantly improve patient outcomes.
Barriers to assessing cerebral autoregulation with near-infrared spectroscopy.
Cardiological interventional procedures
Patients going through cardiac procedures, such as cardiac catheterization or electrophysiological interventions, have significant cardiovascular disease, and therefore, these patients are susceptible to major peri-procedural complications. In a study on the frequency and cause of stroke during and after transcatheter aortic valve implantation, Nuis et al.52 reported a 9% occurrence of stroke (19 of 214 patients), with an early (24 hours after TAVI) stroke in 8 patients and a late (> 24 hours, mean 3.5 days after TAVI) stroke in 11 patients (TAVI). They utilised brain computed tomography scans to investigate the source of the stroke further. Interestingly, they reported that 26% of strokes (5 patients) had lacunar lesions, which are generally thought to be caused by cerebral hypoperfusion in the presence of local atherosclerosis. As a result, the researchers recommended that all attempts be made during TAVI to ensure adequate brain perfusion. According to Meex et al.,53 transcutaneous cardiac treatments, especially those involving transitory partial cardiac standstill, may result in chronic cerebral hypoperfusion despite quick restoration of normal blood pressure. Future initiatives should therefore emphasise the use of noninvasive continuous brain monitoring, such as NIRS, which can offer real-time monitoring and assure cerebral perfusion capacity, during TAVI operations.
Transapical transcatheter aortic valve implantation (TA-TAVI) is a minimally invasive procedure used to treat aortic stenosis in individuals at high risk for cardiac surgery.54 Cox by near-infrared spectroscopy offers the possibility of non-invasively determining cerebral oxygen balance, which recent data suggests may even reflect complete oxygen balance.12
A variety of clinical conditions that are often seen during cardiac catheterization have the potential to disrupt the balance between cerebral oxygen supply and demand. In most studies in the review, NIRS responded immediately to arrhythmias and circulatory arrest and identified an incomplete cerebral recovery, despite seemingly restored hemodynamics.55, 56, 57 Defibrillation threshold testing (DFT) has shown a direct correlation between the reperfusion interval duration and postoperative cognitive impairment. So, rSo2 should be used instead of hemodynamic variables to determine the time between induced arrhythmias.58
Alassar et al.59 compared the evidence and mechanisms of neurological injury between AVR and TAVI in a single-center, prospective study of 127 patients in the UK and concluded that cerebral desaturations (defined as a drop to 80% of baseline rSo2 values, or absolute rSo2 values of less than 50%), as indicated by NIRS monitoring, occurred in two-thirds of patients going through aortic valve replacement (AVR) and one-third of patients going through TAVI. As a result, NIRS has proven to be useful in clinical applications.
Pediatric cardiac surgery
Children with developing brain difficulties caused by genetic defects are among the paediatric patients undergoing heart surgery (organic mental and functional disorders). Patients with genetic defects often have developmental issues, regardless of their heart surgery history. It is difficult to differentiate between congenital and surgically caused brain damage when brain function is not measured prior to surgery. Brain damage is often linked to congenital cardiac problems, hypoplastic left heart syndrome, aortic coarctation, and transposition of the great arteries in patients. In these circumstances, postpartum brain damage may develop owing to a variety of processes, including cerebral hypoxia, hypoperfusion caused by diminished heart function, increased central venous pressure due to intracardiac shunting, and systemic cyanosis.
The watershed region sensitive to hypoperfusion in healthy newborns is the parasagittal cerebral cortex, but in preterm infants it is the periventricular white matter.42 If a child has a deep hypothermic circulatory arrest (DHCA) for more than 40 minutes, he or she is more likely to suffer brain damage.42 Hypotension, low cardiac output, and hypoxia following surgery are all substantial risk factors for brain injury.60 Unlike adults, practically all of the circulating blood volume in infants is exposed to the bypass's synthetic surface during cardiopulmonary bypass. The resulting inflammatory response and exposure to reactive oxygen species occur on a much larger scale, increasing the risk of newborn brain injury.42
Even if global circulation must be temporarily halted, regional low-flow cerebral perfusion with rSO2 monitoring minimises the risk of brain injury in this vulnerable population. According to Austin et al.,61 the surgical team has direct control over a broad range of factors during cardiopulmonary bypass, including the procedures they use and the vital balance between the supply of oxygenated blood and the brain's metabolic requirements.
Neurophysiologic assessment offers additional input to effectively manage cardiopulmonary support so that all the variables may be individually addressed and rapidly familiar to address variations in oxygen supply-demand equilibrium. Since the early days of cardiac surgery, good cerebral ischemia detection has been achieved via EEG monitoring.62 Even while there is growing worry regarding the potential worsening of neurologic and cognitive conditions as a consequence of cardiopulmonary bypass, it has not yet received general support among cardiac surgeons or anesthesiologists. The cerebral oximeter has proven invaluable because of its ability to distinguish between EEG slowing caused by ischemia and that resulting from excessive anaesthesia. In the past, insufficient oxygen delivery results in synaptic depression due to cerebral venous desaturation; in the latter, anesthetic depression of synaptic function reduces the EEG but increases oxygen saturation because of reduced metabolic demand.61 The authors used TCD and NIRS for neurophysiological monitoring in a retrospective study including 250 juvenile patients with congenital heart disease. They found that therapies based on a 50% decrease from baseline in peak flow velocity on TCD or a 20% relative reduction from baseline in rSo2 resulted in fewer postoperative neurologic sequelae and shorter hospital stays.
In a second retrospective study of 50 newborns undergoing surgery for hypoplastic left heart syndrome, 11 suffered 18 adverse events.63 These individuals had a lower mean rSO2 during the first 48 hours following surgery as compared to patients who had no adverse effects. Because the left hemisphere is less oxygenated than the right hemisphere during regional low-flow cerebral perfusion, NIRS oxygen monitoring may be used in paediatric cardiac surgery to evaluate the safe duration of DHCA and the danger of left hemisphere hypoperfusion.42 A decrease in perioperative NIRS oxygen saturation has been connected to post-operative neurological and other disorders. Depending on the clinical scenario, the absolute values may vary greatly. Between children and adults, there are several morphological and physiological differences. For example, newborns' skulls and scalps are thinner because they are less developed than those of adults. These features imply that children's NIRS readings are less affected by extracranial blood flow.42
The use of NIRS during the perioperative phase of closed heart paediatric cardiac surgical operations such as the Blalock-Taussig shunt (BTS), coarctation of the aorta, and vascular rings has received significant support from Lamba et al. During BTS surgery, its use as a supportive monitor, which can detect underflow and overflow across the shunt, and also reveals any vascular anomalies left undetected by echocardiography. Real-time rSO2 monitoring lets doctors find problems and act on them quickly, which can improve the outcome.64 Chengode and Menon recommended NIRS to detect critical cerebralhypoxia in a review of neonatal cardiac surgery.65
Socioeconomic impact of perioperative cerebral injury
The risk of perioperative mortality after cardiovascular surgery is raised by six to eight times, and the possibility of death within ten years is increased by three times. Postop delirium is associated with an increased risk of mortality after cardiovascular surgery. Patients with documented POCD are less productive at work than those who do not have documented POCD, and their general health is worse after discharge. POCD was connected to worse general health and reduced job productivity in a 5-year follow-up study of 261 people who underwent cardiac surgery with cardiopulmonary bypass.66 A review of controlled studies reveals that responding to cerebral desaturation events using the information from cerebral oximetry paired with an interventional algorithm has been associate with reduced instances of cerebral desaturation in surgery,67 less acute kidney injury,68 lower occurrence of stroke, less need for prolonged postoperative ventilation, shorter time on ventilation, shorter hospital length of stay,69 fewer patients requiring blood transfusion, and fewer units of blood transfused.70
Conclusion
There has only been a few published Indian research on the use of NIRS oxygenation monitoring during cardiovascular processes. The current preliminary global evidence, based on studies and case reports, shows that NIRS delivers a quick depiction of cerebral oxygen saturation and that it might detect variations that could not be predicted from standard hemodynamic monitoring. More research is required to determine the effectiveness of NIRS oxygenation monitoring in enhancing neurological outcomes following cardiovascular surgery. This research should include an analysis of the evidence currently available regarding the baseline values of NIRS oxygenation monitoring in clinical practice in a larger Indian population.