Introduction
In present situation strategy of decision among provincial sedative procedures for elective cesarean areas is spinal sedation. The vitally unfriendly impact is the rate of hypotension. Post spinal hypotension during medical procedure is rely upon diminished vascular opposition, diminished cardiovascular result, gauge volume status, standard fringe vascular tone. Parturient with low fringe vascular tone even before spinal sedation blood volume being caught in the furthest points. Spinal sedation cause thoughtful bar would additionally increment blood pooling. Accordingly, expanded chance of creating hypotension in parturient with low pattern vascular tone after spinal sedation.1
For observing parturient we use screens showing pulse, BP, ECG & Masimo Signal Extraction Technology based perfusion record. In the fringe vascular tissue, the proportion of pulsatile blood stream to non-pulsatile blood stream is known as a Perfusion record 2-4 Perfusion file can likewise use to evaluate perfusion elements.2, 3, 4
The spinal sedation produces differential dispersion of blood stream to hindered or unblocked region. 5 Increase in perfusion file esteem tells expanded fringe perfusion by spinal sedation actuated vasodilatation of impeded region. While inverse to it, decline in perfusion file esteem shows vasoconstriction or shift of blood from the checked site.5
Pregnancy increment ladies' aversion to general (GA) & neighborhood sedatives (LA). 8 Many examinations show high benchmark Perfusion record esteem has been related with higher occurrences of spinal prompted hypotension in cesarean conveyances under spinal sedation.1 In parturient with critical hypotension after sub arachnoid block, perfusion list was increment all the more rapidly & get higher worth contrast with normotensive parturient. 9 So Perfusion list can be a decent early indicator of post spinal hypotension.1
Accordingly, this study was attempted to connect the connection between level of hypotension & PI & assess perfusion record (PI) as an early indicator of post spinal sedation prompted hypotension.
Materials and Methods
After getting approval from Committee of Institutional Ethics this prospective observational study was conducted from June 2018 to June 2019. Informed & written consent was obtained from every parturient who came for caesarean section.
Parturient included in our study, age between 18 to 35 years & American society of Anaesthesiologist Physical Status (ASA) Class I or Class II.
Parturient excluded in our study having ASA class III or IV, pre term, post term, parturient with pre-eclampsia, placenta-praevia, gestational diabetes, cardio vascular or cerebro vascular disease & case who are came in contraindications to spinal anaesthesia.
Standard monitoring with electrocardiography for ecg & heart rate, automated noninvasive blood pressure (NIBP) for baseline blood pressure & pulse oximetry (SpO2) for PI & saturation was performed. At the left index finger of hand & toe of foot the perfusion index was measured by using a pulse oximeter probe (Masimo) in all parturient in supine position. Because it was a double-blinded study, the baseline haemodynamic parameters were recorded by an first anaesthesiologist who was not stay in the intraoperative monitoring of the parturient in the supine position. To rule out aortocaval compression effect on the baseline value we use left lateral table tilt of 15° before sub arachnoid block to end of the surgery. Intra venous line secure with 18G cannula in the left upper limb & prehydrate with 500 ml Ringer lactate. Till the cleaning & draping of the patient foetal heart rate was monitored. A second anaesthesiologist who was unknown the baseline values give spinal anaesthesia under all aseptic precaution in sitting position at L3–L4 or L4–L5 interspinous space by using 25G Quincke spinal needle with 2ml of injection hyperbaric bupivacaine 0.5%. Oxygen was attached by use of face mask at 4 L/min to parturient after returned to supine position. By use of a cold swab level of sensory block was checked 5, 10 & 15 min after spinal injection before starting surgery. Parturient were excluded from our study if T6 sensory block level was not achieved & managed according to advised protocol. Heart rate (HR), Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Mean arterial pressure (MAP), perfusion index (PI), saturation (SpO2) & respiratory rate(RR) were recorded at 2 min intervals upto 10 min & then 5 min intervals till the end of surgery after the SAB by the same anaesthesiologist who given SAB.
A diminishing in SBP > 20% from benchmark were characterized hypotension & treated with 100 ml of Ringer lactate & IV bolus of 3 mg infusion mephenteramine & HR <50 beats/min were characterized bradycardia & treated with IV bolus of 0.6 mg infusion atropine. As uterotonic infusion oxytocin 10 units was given at a pace of 200 mU/min as a different imbuement following child extraction. Parturient were barred from the review requiring extra oxytocin or extra careful/sedative intercessions. The frequency of sickness, retching & opposite incidental effects on the off chance that noticed were recorded.
Parturient information were investigated by Mann Whitney U test & autonomous example t test. Relapse investigation with Karl Pearson relationship technique was finished to evaluate the connection between's different boundaries with baselines PI & Receiver Operating Characteristic (ROC) bend was gotten for hypotension to correspond with the gauge PI. Measurable importance was characterized as P<0.05.
Results
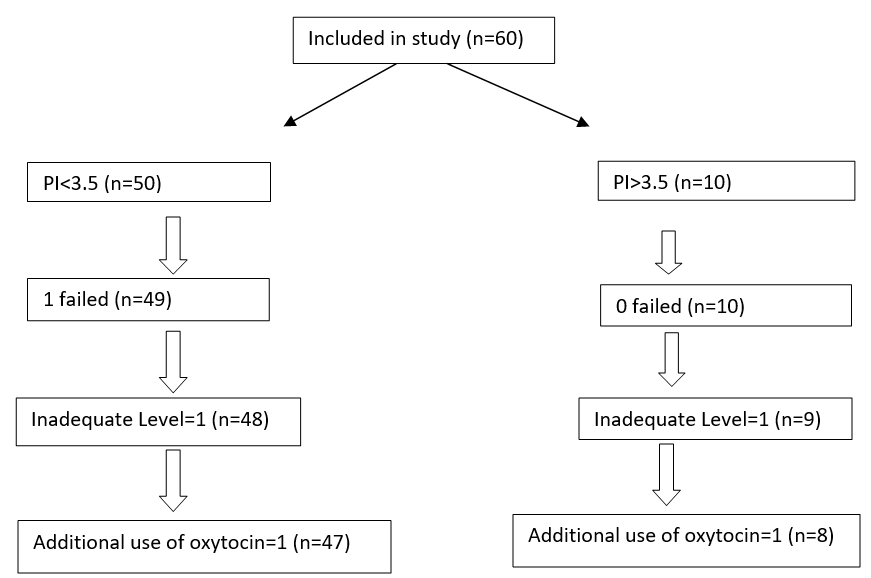
Out of 60 parturient two (2) parturient exclude due to developed inadequate level of the spinal blockade, one (1) parturient was exclude due to failure of spinal anesthesia block, & two (2) parturient exclude due to the use of additional oxytocin, because drug could influence the vitals of the parturient. A total of 55 subjects were analyzed.
Out of 55 parturient, spinal anesthesia was given at L3-L4 interspinous space in 25 parturient & L4-L5 interspinous space in 30 parturient & out of 55 parturient, final dermatome level of sensory blockade at 15 min after spinal anesthesia, was at T4 level in 17 parturient & at T6 level in 38 parturient.
ROC Curve analysis –The ROC curve is created at various threshold settings by plotting the true positive rate (sensitivity) against the false positive rate (1 − specificity). The best possible prediction is 100% specificity (no false positives) & 100% sensitivity (no false negatives). The diagonal line divides the ROC space in two space, points below the line represent bad results (worse than random), points above the diagonal represent good classification results (better than random).
In our review Area Under the ROC Curve = 0.701 with P esteem = 0.015. The standard PI limit was not set in stone by the ROC examinations that foresee hypotension. (Figure 2)
At the point when we anticipated hypotension by benchmark boundaries like Baseline PI at finger & toe there was no critical variety in Baseline PI at finger (r = 0.131; p > 0.05).
hows that out of 8 parturient (15%) had high standard PI (PI>3.5), 7 (87%) parturient foster hypotension, though out of 47 parturient (85%) had low pattern PI (PI≤3.5), 12 (25%) parturient foster hypotension. Benchmark PI foresee hypotension with a particularity of 97% (95% CI 85-close to 100%), responsiveness of 37% [95% certainty spans 16-62%], positive prescient worth of 87%, & negative prescient worth of 74%. (P < 0.05)
2 shows that parturient with high & low standard PI, systolic pulse diminished altogether after spinal infusion. However, more prominent reduction in systolic pulse at 5-10 min & 25 min in parturient having high benchmark PI had after spinal infusion than parturient having low standard PI. (P < 0.05) (Fig - 2)
Percent decline in mean blood vessel pressure (MAP) essentially connect to benchmark PI, which was affirmed by Multiple direct relapse examination. (r = 0.436; P < 0.05) (Figure 4)
Parturient standard pulse (AUC = 0.446, P esteem = 0.513), level (AUC = 0.455, P esteem = 0.589) & weight (AUC = 0.603, P esteem = 0.212) couldn't anticipate hypotension.
Table 1
At baseline perfusion Index 3.5 & prediction of hypotension
|
Baseline PI |
Hypotension |
||
|
Present |
Absent |
Total |
|
|
>3.5 |
7 (True Positive) |
1(False Positive) |
8 |
|
≤3.5 |
12 (False Negative) |
35(True Negative) |
47 |
|
Total |
19 |
36 |
55 |
Table 2
Distribution of systolic blood pressure (mm of Hg) in parturient having baseline PI >3.5 & ≤3.5
Discussion
It is a well-known fact that sub arachnoid block is the most common method of administering anaesthesia in lower segment caesarean section. The most common complication of sub arachnoid block is hypotension.6
In the present study, parturient having baseline PI values more than 3.5 the incidence & severity of hypotension was higher. The ROC curve showed that baseline PI was suitable parameter for detecting parturient at risk for post spinal hypotension during LSCS. It differentiate parturient who developed post spinal hypotension versus those who did not. For predicting post spinal hypotension in parturient undergoing lower segment caesarean section, it provide a new baseline PI value of 3.5 as the utmost point with a sensitivity of 37% & specificity of 97%.
When we predicted hypotension by baseline parameters like Baseline PI at finger of hand & toe of foot there was no significant variation in Baseline PI at finger (r = 0.131; p > 0.05). So, we used baseline PI at toe in our study.
Many haemodynamic parameters have been studied as predictors of hypotension. Some researchers like Toyoma S et al,1 Duggappa DR et al.7 have done studies for prediction of post spinal hypotension in caesarean section by using perfusion index.1 The Perfusion index used as a new parameter to evaluate the circulatory state & relative assessment of the pulse strength at the monitoring site. It was derived from the plethysmographic waveform. It was calculated by –3
AC represent the throbbing part of infrared sign, the light which was consumed by the throbbing blood vessel stream. DC addresses the non-pulsatile part of infrared sign, the light which is consumed by the skin, different tissues & non-pulsatile measure of blood at the vascular site.
Subsequently, perfusion elements can evaluate by utilization of perfusion record. Perfusion file is being use as a painless strategy to distinguish the improvement of post spinal hypotension.2, 3, 4
PI esteem shows the strength of the infrared (940nm) signal getting back from the checking site its worth reaches from for powerless heartbeat 0.02% to solid heartbeat 20%. That demonstrates the strength of the IR (infrared) signal getting back from the checking site.8
Decline in foundational vascular obstruction alongside expansion in cardiovascular result is a physiological change in pregnancy.9 Fall in the resting tone will prompt vasodilatation & ascend in the pulsatile part of perfusion record & cause an ascent in values. The sympathectomy after spinal sedation will impede the thoughtful nerves & loss of vascular tone made hypotension due expanded pooling blood in legs. Higher perfusion list values tell about increment pulsatile part in decline vascular tone vessals. Parturient with ease off fringe vascular volume before spinal sedation mean high gauge perfusion list are supposed to have more gamble to foster post spinal hypotension.
In a review, Mowafi HA et al4 showed that perfusion file had the option to identify thoughtful bar following epidural sedation utilizing 2% lignocaine with adrenaline. Ginosar Y et al3 saw that either skin temperature or MAP for the improvement of epidural prompted sympathectomy, PI was a high level & more delicate marker.
Yokose M et al10 showed that for post spinal hypotension in parturient PI had no prescient worth. This distinction was because of different logical contrasts, definitions, colloids co-stacking, & estimation of gauge Perfusion Index esteem.
Toyama S et al.1 concentrated on the relationship between's benchmark perfusion file & hypotension in 35 parturient. They showed a positive relationship ROC bend with AUC = 0.87. Duggappa DR et al.7 concentrated on 126 parturient in two gathering. Bunch 1 having 57 parturient PI < 3.5 & bunch 2 having 63 parturient PI > 3.5. They showed a positive connection & region under ROC bend = 0.848. A critical relationship between's number of episodes of hypotension & benchmark PI (rs 0.416, P < 0.001). The occurrence of hypotension is more in parturient having PI more than 3.5 (Group I 10.5% & Group 2 71.42%) (P < 0.001). At an endpoint 3.5 pattern PI foresee hypotension with 69.84% responsiveness & 89.29% particularity.
George J et al.11 tracked down in 30 parturient 66.7% rate of hypotension. There was critical connection between's fall in SAP from benchmark & standard PI (r = 0.368, P < 0.05). The ideal endpoint of PI was viewed as 3.6 with 80% awareness & 60% particularity.
In our review, we look at in Indian populace, the benchmark PI more than 3.5 & frequency of hypotension were essentially connecting with a worth r = 0.436 (P < 0.05), a tracking down near the concentrate by Toyama S et al.1
Toyama S et al.1 found for a most extreme place of benchmark PI esteem 3.5 with 81% responsiveness & 86% explicitness, to foresee hypotension, while in our review, 97% particularity & 37% awareness for a most extreme worth of 3.5 of the gauge PI. In our review, spinal sedation was utilized to accomplish a block level of T6, spinal epidural method was utilized in the concentrate by Toyama S et al.1 They utilized infusion phenylephrine to treat hypotension while we utilized infusion mepheteramine 3mg bolus.
A few impediments in this review. Preferably perfusion file ought to have been contrasted & intrusive blood vessel pulse. We have contrasted perfusion record & painless pulse. NIBP measure circulatory strain with a delay. Nonetheless, blood vessel cannulation was improper for each elective cesarean area. Patient nervousness, patient development, temperature at the estimating site & aortocaval pressure impact in recumbent position can likewise influence the pattern esteem. In this review, we recorded gauge PI values with 150 remaining sidelong table slant & without patient development. To ease tension all parturient were advised prior to taking them activity theater for cesarean segment. Fundamental vascular opposition estimation likewise intrusive & superfluous for the simple cesarean area.
Since PI is rely upon the vascular tone of vessels. Job of PI in anticipating post spinal hypotension in conditions where the tone of these vessels is impacted is dubious. More exploration studies with respect to PI use in parturient should be finished before it was acknowledged as a widespread painless device to foresee post spinal hypotension.