Introduction
The subarachnoid space depth varies significantly at different levels of the spinal column. There are Individual and inter-individual variations at the same vertebral level. So, a proper pre-puncture estimation of the skin to the subarachnoid space depth happens to be a good guide for proper spinal needle placement. Adequate knowledge of the subarachnoid space depth usually aids in choosing an appropriate size of spinal needle.1, 2
A conventional spinal needle might usually be too long for a thin patient, while it would come short of length for an overweight patient leading to multiple unsuccessful punctures resulting in discomfort of the patient.3, 4 This signifies that a co-relation might exist between physical parameters of individuals like age, sex, height, weight and Body Mass Index (BMI) with that of subarachnoid space depth. By determining this co-relation between the physical parameters (age, sex, BMI) we may succussed in predicting the skin to subarachnoid Space depth.
Materials and Methods
After getting approval from the Institutional Ethics Committee, an informed written consent was obtained from 100 adult patients of either sex, of age between 18 years to 65 years, with American Society of Anaesthesiologist I and II, scheduled for elective surgical procedures using spinal anaesthesia. This present study was conducted in the Department of Anaesthesiology, Saveetha Medical College and Hospital, Chennai from August 2020 to February 2021.
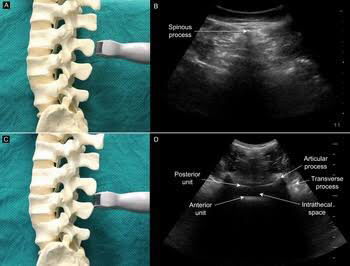
Patient characteristics including name, gender, age, body weight, body height, body surface area (BSA), and body mass index (BMI) were recorded upon arrival to the operating theatre (Table 1). Premedication was given to all patients as per our hospital protocol. All patients were monitored using electrocardiogram, pulse oximetry, and non-invasive blood pressure. A proper I.V line was secured. The patients were placed in sitting position with their back fully flexed and under aseptic precautions ultrasound guided scan was done in the midline of L3-L4 intervertebral space. After obtaining the BAT sign (Figure 1) at the level of the interspinous space, the subarachnoid space depth was measured and the point of entry was marked with a sterile marker.
Figure 1
Ultrasound of spine. Ultrasound probe kept intransverse orientation at the level of spinous process (A) and corresponding image (C). Ultrasound probe kept in transverse orientation at the level of interspinous space (B) and corresponding image showing BAT sign (D)
A 25-gauge Quincke Babcock (3.5 inches) spinal needle was used to puncture the dura through the midline approach. The spinal needle was inserted in the midline as per the direction of the ultrasound probe while doing the scan prior and advanced until loss of resistance was just felt and confirmed by the first appearance of the free flow of cerebrospinal fluid. In patients were there was blood in cerebrospinal fluid and those in whom either the approach of spinal needle was changed from midline to paramedian or the angle of spinal needle was not proper were excluded from the study. The required intrathecal local anaesthetic dose was calculated based upon the surgical requirement and patient characteristics. After giving intrathecal injection, the spinal needle was marked with a help of a sterile skin-marking pen and then grasped between the thumb and index finger abutting the patient's back and removed. The depth of insertion was then measured with a standard scale and noted. Patient were then put in supine position and the level of block was checked. Surgery was proceeded after achieving adequate block.
Craig's and Stocker's formula were calculated individually in all the patients to determine the predicted SSD in the overall population.
Craig's formula: SSD (cm) = 0.03 cm × height (cm)
Stocker's formula: SSD (mm) = 0.5 × weight (kg) +18
The values obtained by Stocker's formula in millimetres was converted to centimetres unit only for the purpose of comparison
Finally, three values were obtained (ultrasound guided depth, stocker’s formula and craig’s formula) were compared to the actually measured depth using the quinke Babcock spinal needle to find out which value correlates closer to the actual sub-arachnoid space depth.
Statistical Analysis and Results
The data obtained was entered in Ms Excel and analysed using SPSS version 19.0(Statistical packages for social Sciences) version 19.0. Mean & SD was calculated for subarachnoid space depth using each formula and also by observed methods. The mean and SD were also calculated for patient characteristics. Independent t-test was done to compare the Mean difference in subarachnoid space depth. Forward stepwise multivariate regression analysis was done to estimate the covariant that might influence skin to subarachnoid space depth.
Table 1
Demographic information of data
Table 2
Frequency and percentage information of age and ASA status
|
S.No |
Variable |
Frequency |
Percentage |
|
1 |
Gender |
||
|
|
Male |
76 |
76 |
|
|
Female |
24 |
24 |
|
2 |
ASA |
||
|
|
I |
65 |
65 |
|
|
II |
35 |
35 |
Table 3
Information of mean difference, 95% confidence interval, P value and correlation coefficient of the different methods used to determine subarachnoid space depth
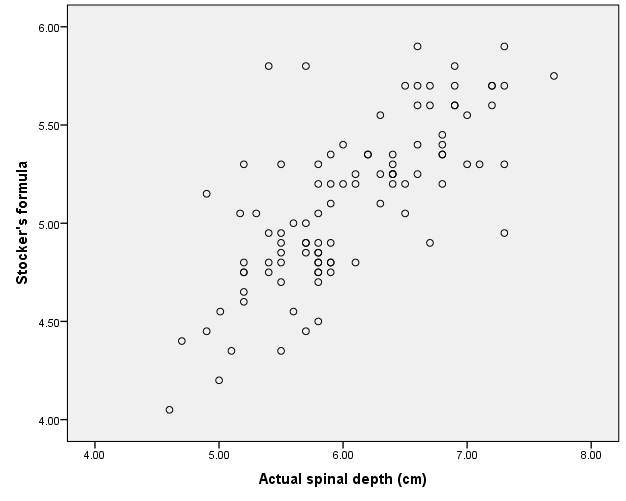
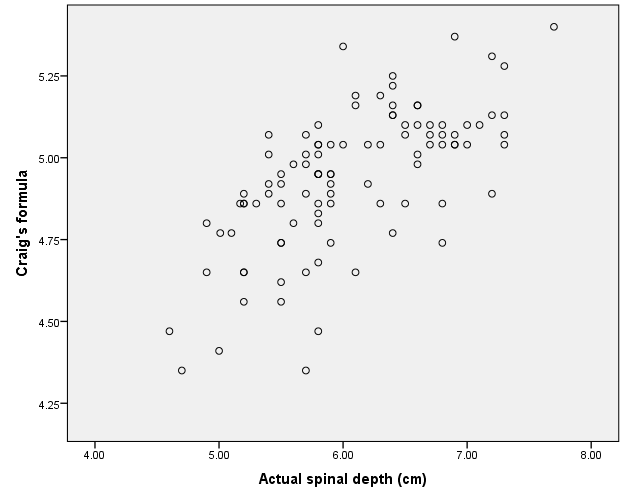
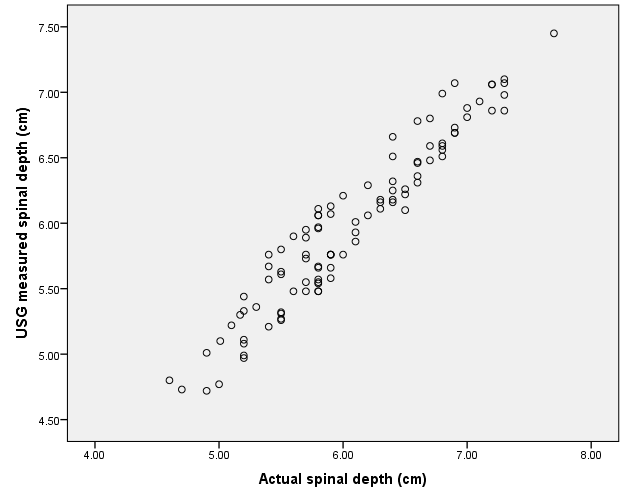
Figure 2
Correlation between actual subarachnoid space depth and ultrasound measured subarachnoid space depth
Discussion
Lumbar puncture is commonly done by anaesthetist for administering spinal anaesthesia.5 A correct placement of spinal needle is generally crucial while giving medications.6 Apart from knowing about the anatomy of spinal cord and technical skill, an estimate of skin to subarachnoid space depth done prior to puncture will usually guide in placing a spinal needle.
Knowledge of subarachnoid space depth will help in choosing a spinal needle of an appropriate length.7, 8 A conventional spinal needle might usually be too long for a thin patient, while it would come short of length for an overweight patient leading to multiple unsuccessful attempts and therefore increases patient discomfort.9
In our study the mean difference of subarachnoid space depth measured using ultrasound was found to be 0.0719 as compared to 0.0947 using stocker’s formula and 1.120 using craig’s formula (Table 2).
The 95% confidence interval of ultrasound guided measurement of subarachnoid space depth is 0.03-0.11 as compared to 0.85-1.04 of stocker’s formula and 1.007-1.23 of craig’s formula.
The P value for all three methods of estimating subarachnoid space depth is <0.05 (i.e; is all three methods provided significant values). The correlation coefficient using ultrasound guided measurement of subarachnoid space depth is 0.958 as compared to 0.736 of stocker’s formula and 0.656 of craig’s formula (Table 3).
All three methods provided significant values (P value < 0.05) but the values obtained via ultrasound measurement of subarachnoid space depth correlated more closely (correlation coefficient of 0.958) to the actual measured subarachnoid space depth. (Figure 2, Figure 3, Figure 4)
The limitation of our study is that the formula derived from our study can be applied only when midline approach is employed with spinal needle insertion done perpendicular to the skin and only in patients with no spinal anomaly. A paramedian approach will increase the needle insertion distance by varying degrees depending on the inclination of the needle. Our study does not include patients who have already undergone previous spinal surgeries and pregnant population undergoing lower segment caesarean section.
Conclusion
Ultrasound measurement of subarachnoid space depth correlates more closely to the actual measured subarachnoid space depth and hence its superior compared to stocker’s and craig’s formula.10 Also, ultrasound of the spine provides us with an accurate landmark for spinal needle insertion, thus helps us in choosing a spinal needle of appropriate length preventing complications related to traditional landmark techniques such as multiple punctures, unsuccessful attempts, patient discomfort, etc.11