- Visibility 153 Views
- Downloads 12 Downloads
- DOI 10.18231/j.ijca.2021.076
-
CrossMark
- Citation
Comparison of Dexmedetomidine with Fentanyl and Pentazocine – Promethazine in patients undergoing dilation and curettage in monitored anesthesia care
- Author Details:
-
Akanksha Aggarwal *
-
Divya Mahajan
Introduction
Conscious sedation is a technique of providing analgesia, sedation and anxiolysis while keeping in mind that rapid recovery is ensured without adverse effects. [1], [2], [3], [4] Conscious sedation is given with the prime goals of rapid and safe establishment of procedural condition for performing therapeutic or diagnostic procedures while ensuring fast, predictable recovery with minimal postoperative events. Dexmedetomidine being a selective α2 adrenoceptor agonist has sedative, amnestic, sympatholytic and analgesic effects.[1] It has been used in a number of clinical trials as effective and safe substance. Dexmedetomidine provides an excellent analgesia, conscious sedation in patients who seem to be asleep, however can easily be awaken. There is no respiratory depression which makes dexmedetomidine one of the freely used medication in anesthesia. These characteristics of dexmedetomidine make it suitable for sedation and analgesia during the perioperative period. Its use as a premedication, as an adjunct for general and regional anesthesia and as a postoperative sedative and analgesic are similar to those of the benzodiazepines.[5]
Pentazocine was the first of opioid analgesic and antagonist to have widespread use. Pentazocine is a synthetic analgesic class which shows both agonist and weak antagonist activity at the opioid receptors.[6], [7] The physiologic effects of pentazocine are similar to morphine and it has one third of morphine’s analgesic potency. Pentazocine depresses myocardial contractility, but increases myocardial oxygen demand as it increases peripheral resistance, blood pressure and the plasma catecholamine level. Despite weak antagonist action, it precipitates opioid withdrawal reactions. It is expected that it would have a ceiling effect on visceral pain and respiratory depression. Adverse reactions seen include potential for psychotomimetic effects such as confusion, disorientation, hallucinations, depression and dysphoria. Doses causing sedation have been seen to be associated with diaphoresis and dizziness.[8]
Pentazocine has been used for day care sedation procedures in doses approximating 0.5 mg/kg, usually to a maximum of 30 mg. In these doses it can have a duration of action of 1 hour. This study attempted to investigate whether Dexmedetomidine with Fentanyl combination is an effective alternative modality to pentazocine with promethazine as sedation in regards to hemodynamic stability and recovery for patients undergoing Dilatation and curettage.
Materials and Methods
After Ethical Committee approval and written informed consent from patients, a randomized controlled trial was conducted at tertiary care center. 50 patients, aged 18-60 years of age were taken who were undergoing diagnostic and therapeutic D and C with American Society of Anesthesiologist (ASA) Grades I and II. Exclusion criteria included patients with ASA physical status Grade III and more, baseline oxygen saturation (SpO) <90%, patients with comorbid conditions such as diabetes mellitus, hypertension (HTN) or hepatic or renal insufficiency. Patients who had a known allergy to these drugs, difficulty in communication (due to language problem or deafness) and with a history of egg or soya bean allergy were also excluded. Preoperative anaesthesia check-up was done. In operating room, venous access was established on the nondominant hand of every patient by 18G/20G cannula and intravenous (IV) fluid was started. Baseline parameters recorded were heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MAP), respiratory rate (RR) and SpO2%. These were again recorded immediately after the loading dose (0 min) and then at 2, 5 and 10 min during the procedure and then after completion of the procedure.
Sample Size: 50 Patients divided to two groups, each group contained 25 patients: Group (D + F): After Pre–operative vital data was recorded as a baseline values, patient received Fentanyl 1 μg/kg, then dexmedetomidine loading dose 1 μg/kg over 10 min and followed by 0.5 μg/kg/hr infusion till completion of surgery. Dexmedetomidine was diluted in preservative free normal saline. Group (P+P): After preoperative hemodynamic data was recorded as baseline values, patient was administered Pentazocine 0.5mg/kg (max 30mg) and then Promethazine 12.5mg slow intravenous bolus. Surgical procedure was started when Ramsay sedation score[4] 3 was achieved. If not achieved Propofol was given as intermittent bolus doses till RSS 3 is achieved.
Statistical analysis: Quantitative data were expressed as mean± standard deviation (SD). Qualitative data were expressed as frequency and percentage. Independent-samples t-test of significance was used when comparing between two means. Chi-square test of significance was used in order to compare proportions between two qualitative parameters. P-value <0.05 was considered as significant.
In the recovery room, MAS[9] of patients were recorded every 5 min by anesthesiologist along with any adverse effect such as restlessness, shivering, nausea, vomiting, abdominal discomfort and respiratory depression. On achieving MAS of 9-10, patients were discharged. In the case of any adverse events in the recovery room such as nausea, vomiting, abdominal discomfort and respiratory depression, the patients were observed in the hospital for at least 12 hours.
Results
Two groups were comparable in terms of demographics and baseline vitals ([Table 1]).
|
Baseline Parameter |
Group D+F |
Group P+P |
P Value |
|
Age (Years) |
39±11 |
40±10 |
0.73 |
|
Weight (Kg) |
56±9 |
54±10 |
0.46 |
|
ASA Grade I (N) |
19 (76%) |
17 (68%) |
0.53 |
|
Pre OP HR (per min) |
94±11 |
91±9 |
0.29 |
|
Pre OP RR (per min) |
17±3 |
16±4 |
0.32 |
|
Pre OP SBP (mmHg) |
124±17 |
132±18 |
0.11 |
|
Pre OP DBP (mmHg) |
86±13 |
82±14 |
0.30 |
|
Pre OP MAP (mmHg) |
104±12 |
102±14 |
0.59 |
|
SpO2 (%) |
98±2 |
98±2 |
1.0 |
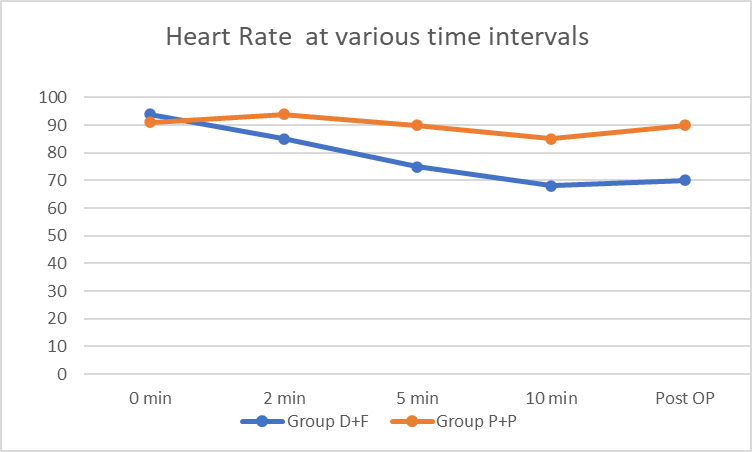
Group (D+F) had significantly (P < 0.05) lower HR after infusion of loading dose at 2, 5 and 10 min during procedure and immediately after procedure ([Figure 1]) ([Table 2]).
|
Time |
Group |
HR |
RR |
SBP |
DBP |
MAP |
|
0 min |
D+F |
94±11 |
17±3 |
124±17 |
86±13 |
104±12 |
|
P+P |
91±9 |
16±4 |
132±18 |
82±14 |
102±14 |
|
|
P value |
0.29 |
0.32 |
0.11 |
0.30 |
0.59 |
|
|
2 min |
D+F |
85±8 |
16±2 |
104±14 |
82±11 |
96±10 |
|
P+P |
94±12 |
16±3 |
134±20 |
84±12 |
102±12 |
|
|
P value |
0.003 |
1.0 |
<0.0001 |
0.54 |
0.06 |
|
|
5 min |
D+F |
75±9 |
16±2 |
96±10 |
78±10 |
90±6 |
|
P+P |
90±10 |
15±2 |
138±16 |
88±10 |
104±10 |
|
|
P value |
<0.0001 |
0.08 |
<0.0001 |
0.0009 |
<0.0001 |
|
|
10 min |
D+F |
68±6 |
16±2 |
92±8 |
70±8 |
82±8 |
|
P+P |
85±9 |
15±2 |
140±12 |
90±8 |
106±7 |
|
|
P value |
<0.0001 |
0.08 |
<0.0001 |
<0.0001 |
<0.0001 |
|
|
Post OP |
D+F |
70±10 |
16±3 |
100±14 |
72±11 |
90±10 |
|
P+P |
90±12 |
16±2 |
142±16 |
92±12 |
110±12 |
|
|
P value |
<0.0001 |
1.0 |
<0.0001 |
<0.0001 |
<0.0001 |
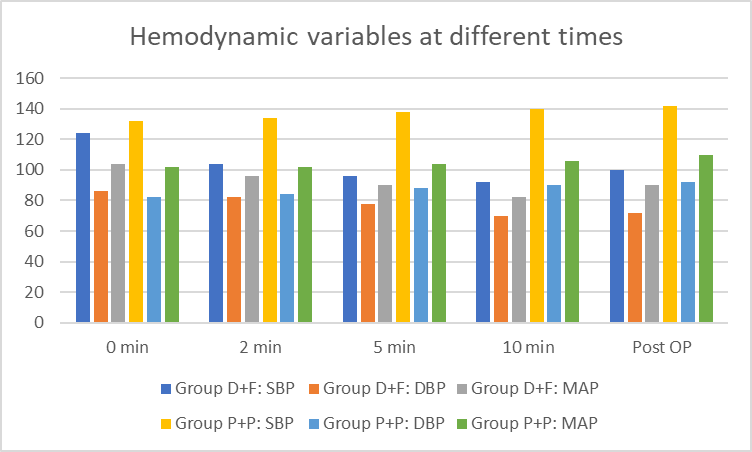
Eight patients (32%) in Group D+F and only one patient (4%) in Group P+P had bradycardia (P < 0.05) but none of the patients required any medication to treat it. Patients in Group P had higher MAP at 2, 5 and 10 min during the procedure and immediately after procedure, and the difference was statistically significant [Figure 2]. In Group D+F, patients had significantly more incidences of hypotension when compared with the Group P+P. SBP, DBP and MAP were also statistically lower in Group D+F at 5 and 10 min and also postoperatively as compared to Group P+P (P < 0.05) ([Figure 2]) ([Table 2]). Statistically significant difference in SBP was also seen at 2 min after loading dose in the two groups. No patient in either group had hypoxia. Requirement of rescue drug (propofol) during the procedure was 9.7 ± 9 mg in Group D and 18.8 ± 9.5 mg in Group P, the difference was not statistically significant. 5 patients (20%) in group P, whereas none in group d had episode of nausea and vomiting intra-operatively or in the recovery room. The recovery was quicker in Group D when compared with the Group P and result was statistically significant. Average time for recovery (MAS 9-10) was 3.2 ± 2.3 min in Group D and 11.3 ± 5.5 min in Group P (P < 0.05).
Discussion
Conscious sedation is a technique to provide analgesia, sedation and anxiolysis while ensuring fast recovery without adverse effects. Conscious sedation is administered with main goals of rapid and safe establishment of satisfactory perioperative condition for the performing therapeutic or diagnostic procedures while ensuring quick predictable recovery with minimal postoperative events. Conscious sedation provides greater flexibility in scheduling procedures so we can maintain higher volume of patients.[3] There is decrease in dependence on the hospital bed availability. There is also a lower incidence of sepsis, respiratory and cardiovascular complications. It requires less preoperative assessment and postoperative medications. Early recovery and ambulation decrease periprocedural morbidity and mortality. Conscious sedation also decreases overall procedural costs. Patients being able to observe the procedure, can communicate with surgeon during the procedure which leads to high patients and surgeon satisfaction. Dexmedetomidine is a selective alpha2 agonist with analgesic and sedative properties.[10] These effects of dexmedetomidine make it suitable for sedation and analgesia during the whole perioperative period. Its use as a premedication, as an anesthetic adjunct for general and regional anesthesia and as a postoperative analgesic and sedative are similar to those of the benzodiazepines. Pentazocine is a benzomorphan derivative that has opioid agonist as well as weak antagonist actions. Using combination of two agents can provide better patient control and allows the use of smaller doses of each single agent avoiding its undesirable effects.
Promethazine is used as a sedative and hypnotic during anesthesia and as a premedication for anesthesia. It prevents nausea/vomiting by blocking the action on acetylcholine and adds a bit of mild sedation with pentazocine. Opiates provide analgesia and sedation during surgical procedures. Fentanyl is favored because of its fast onset and short duration of action. Unlike morphine, fentanyl causes minimal cardiovascular depression and therefore, hypotension rarely. Fentanyl binds with stereo specific receptors at sites within the CNS and increases pain threshold, varies pain reception, and inhibits ascending pain pathways. Along with analgesia, fentanyl suppresses the cough reflex and precipitates respiratory depression, drowsiness, and sedation. The half-life of fentanyl is 2-4 hours. In our study, continuous infusion of dexmedetomidine was administered to maintain a steady sedation level.
In our study, we deduced that for heart rate was significantly decreased in dexmedetomidine group. The difference between the two groups being significant from 2 min after loading dose and throughout till post-operative period. Blood pressure decreased in D+F group whereas it increased in P+P group. SBP was significantly different from 2 min after loading dose, DBP and MAP were significantly different from 5 min after loading dose.
In study of Solanki et al.[11] who Compare of the efficacy of dexmedetomidine, pentazocinepromethazine combination in tympanoplasty surgery there was a significant difference between the hemodynamic response and satisfactory sedation in two groups. this agree with our study but the difference between the groups was higher in this study. In study of Khanduja et al.[12] also showed that patients in the dexmedetomidine group required lower use of rescue propofol. In our study there was a significantly lower use of rescue propofol in dexmedetomidine and fentanyl group which agree with study of khanduja et al.
In study of Memon et al [13] they found Intravenous Dexmedetomidine is an excellent drug for surgeries like Tympanoplasty done under onitored anaesthesia care. It not only improves intraoperative anaesthesia but also postoperative analgesia and thereby, improving the outcome of surgery. Our study reports similar findings.
Study of Manoj et al [14] showed that Recovery time, as assessed by modified Aldrete Score was significantly longer in propofol Group (13.93±3.11 minutes) compared to Dexmedetomidine group (5.63±1.40min). In our study also, post-operative recovery time was longer in group P+P than in group D+F.
In the study of Yağan et al [15] also showed that the time for reaching MAS 9 was shorter in the dexmedetomidine group and the difference was statistically significant. This agree with our study.
Conclusion
Dexmedetomidine provides conscious sedation with analgesia without respiratory depression, unlike most analgesic/sedative drugs, such as opioids, benzodiazepines, and propofol. Moreover, degree of satisfaction experienced by patients as well as surgeons was better with dexmedetomidine. Therefore, dexmedetomidine in combination with fentanyl is effective to provide conscious sedation for dilatation and curettage (D&C) procedures in adults and it can be a valuable alternative to pentazocine and promethazine.
Source of Funding
None.
Conflict of Interest
The author declares no conflict of interest.
References
- BC Bloor, DS Ward, JP Belleville, M Maze. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology 1992. [Google Scholar]
- JE Hall, TD Uhrich, JA Barney, SR Arain, TJ Ebert. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg 2000. [Google Scholar]
- K Nii, H Hanada, F Hiraoka, A Eto, T Mitsutake, M Tsutsumi. Usefulness of Consciousness Sedation with Dexmedetomidine and Pentazocine during Endovascular Treatment for Acute Stroke. Neurol Med Chir (Tokyo) 2018. [Google Scholar] [Crossref]
- MA Ramsay, TM Savege, BR Simpson, R Goodwin. Controlled sedation with alphaxalone-alphadolone. Br Med J 1974. [Google Scholar]
- O Inatomi, T Imai, S Bamba, H Hasegawa, H Ban, A Nishida. Safety and Efficacy of Dexmedetomidine Combined with Midazolam and Pentazocine for Sedation During Endoscopic Retrograde Cholangiopancreatography (ercp). Gastroenterol Endosc 2015. [Google Scholar]
- MA Rafee, P Kinjavdekar, HP Aithal. Clinico-physiological and haemodynamic changes during midazolam-ketamine anaesthesia in dogs premedicated with dexmedetomidine with or without pentazocine. Indian J Vet Surg 2016. [Google Scholar]
- P Sethi, S Sindhi, A Verma, KL Tulsiani. Dexmedetomidine versus propofol in dilatation and curettage: An open-label pilot randomized controlled trial. Saudi J Anaesth 2015. [Google Scholar]
- S Sethi, J Singh, I Nath, RK Das, S Nayak, RK Sahu. Haemato-biochemical comparision of xylazine/dexmedetomidine in combination with butorphanol/pentazocine as preanesthetic to ketamine anaesthesia in canine pyometra patients. Pharma Innov 2017. [Google Scholar]
- JA Aldrete, D Kroulik. A postanesthetic recovery score. Anesth Analg 1970. [Google Scholar]
- T Kamibayashi, M Maze. Clinical uses of alpha2 -adrenergic agonists. Anesthesiology 2000. [Google Scholar]
- U Solanki. Comparison of Dexmedetomidine vs. Pentazocine - Promethazine for Tympanoplasty under MAC: A Randomized Double Blind Study. Indian J Anesth Analg 2018. [Google Scholar]
- S Khanduja, A Ohri, M Panwar. Dexmedetomidine decreases requirement of thiopentone sodium and pentazocine followed with improved recovery in patients undergoing laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 2014. [Google Scholar]
- N Memon, RG Pathak. A Comparative Study of Dexmedetomidine Versus Midazolam-Pentazocine for Tympanoplasty Under Monitored Anaesthesia Care. J Med Sci Clin Res 2015. [Google Scholar]
- M Kamal, DG Singariya, K Kumari, D Gupta, B Paliwal, P Bhatia. Comparative Evaluation of efficacy, hemodynamic stability and recovery during conscious sedation with dexmedetomidine or propofol in cardiac catheterization laboratory. J Dent Med Sci 2017. [Google Scholar]
- Ö Yağan, R H Karakahya, N Taş, A Küçük. Comparison of Dexmedetomidine Versus Ketamine-Propofol Combination for Sedation in Cataract Surgery. Turk J Anaesthesiol Reanim 2015. [Google Scholar]
How to Cite This Article
Vancouver
Aggarwal A, Mahajan D. Comparison of Dexmedetomidine with Fentanyl and Pentazocine – Promethazine in patients undergoing dilation and curettage in monitored anesthesia care [Internet]. Indian J Clin Anaesth. 2025 [cited 2025 Sep 05];8(3):396-400. Available from: https://doi.org/10.18231/j.ijca.2021.076
APA
Aggarwal, A., Mahajan, D. (2025). Comparison of Dexmedetomidine with Fentanyl and Pentazocine – Promethazine in patients undergoing dilation and curettage in monitored anesthesia care. Indian J Clin Anaesth, 8(3), 396-400. https://doi.org/10.18231/j.ijca.2021.076
MLA
Aggarwal, Akanksha, Mahajan, Divya. "Comparison of Dexmedetomidine with Fentanyl and Pentazocine – Promethazine in patients undergoing dilation and curettage in monitored anesthesia care." Indian J Clin Anaesth, vol. 8, no. 3, 2025, pp. 396-400. https://doi.org/10.18231/j.ijca.2021.076
Chicago
Aggarwal, A., Mahajan, D.. "Comparison of Dexmedetomidine with Fentanyl and Pentazocine – Promethazine in patients undergoing dilation and curettage in monitored anesthesia care." Indian J Clin Anaesth 8, no. 3 (2025): 396-400. https://doi.org/10.18231/j.ijca.2021.076
