- Visibility 276 Views
- Downloads 48 Downloads
- Permissions
- DOI 10.18231/j.ijca.2021.069
-
CrossMark
- Citation
Correlation of skin epidural distance and posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient: A prospective randomised study
- Author Details:
-
Akhilesh Gupta
-
Farhat Singh
-
Rajani Mandhyan
-
Anshu Gupta *
Abstract
Background: Lumbar epidural block is a commonly used procedure for providing anaesthesia, post-operative analgesia in all groups of patients irrespective of age, sex, weight and height of the patients. The knowledge of posterior space is important in view of the fact that this is the space where drugs for epidural anaesthesia/ analgesia are used. The knowledge of variability of this space with physical parameters of the patient, help us in reducing the incidence of total spinal anaesthesia.
Materials and Methods: Two hundred adult patients in the age group of 20-60 years requiring subarachnoid block were chosen for the study. Using 22G Quincke spinal needle, epidural space was identified and skin epidural distance was measured. Proceeding the spinal needle further, causes needle to lie in subarachnoid space. The skin subarachnoid distance was measured. The difference between skin-subarachnoid distance and skin epidural distance denoted the posterior epidural space width. Its correlation with physical parameters was studied.
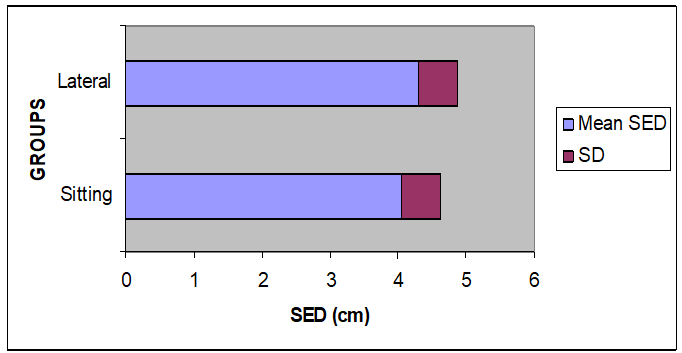
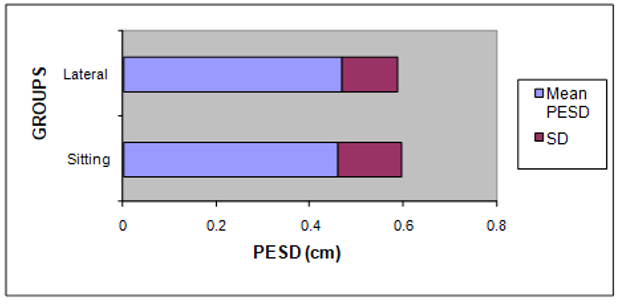
Result: Mean skin epidural distance was 4.30 ±0.57 in lateral position and 4.05 ± 0.57 in sitting position, the difference being statistically significant. (P= 0.002). There was positive correlation between skin epidural distance with weight, BMI and abdominal girth of the patient. Mean posterior epidural space depth was 0.468+14 cm in lateral position and 0.459+0.14 cm in sitting position, the difference being statistically insignificant. There was a positive correlation between posterior epidural space depth and height of the patient.
Conclusion: The skin epidural distance varies with weight, BMI, abdominal girth and position of the patient. The posterior epidural space depth varies with the height of the patients.
Introduction
In present day anaesthesia practice, lumbar epidural block is a widely used procedure. Knowledge about skin epidural distance and posterior epidural space depth is crucial to avoid accidental dural puncture and consequent headache and other dreadful complications of epidural anaesthesia.[1], [2]
The skin epidural distance (SED) varies at different levels of vertebral column in a same patient. It also varies from patient to patient at the same inter-vertebral level.[3] Various factors like age, sex, weight, height, body mass index (BMI), abdominal girth and position of the patient are known to determine the skin epidural distance.[4], [5], [6]
During placement of epidural needle a false loss of resistance can occur if the epidural needle, after passing into spinous ligament, enters either the prevertebral or the paravertebral space. Injection of local anaesthetic in either of these spaces results in an inadequate block.
Therefore a study was conducted to determine the characteristics and variability of skin epidural distance and posterior epidural space depth in lateral and sitting postures. Also the correlation between these two (i.e., skin epidural distance and posterior epidural space) with age, sex, weight, height, BMI, abdominal girth in lateral and sitting position was also observed.
Materials and Methods
Ethics: Clearance was taken from Institutional Review Board.
Methodology
Two hundred adult patients between 20-60 years, ASA Grade I or II, scheduled for elective lower abdominal, perineal, orthopedic or plastic/reconstructive surgery under Subarachnoid block were taken up for the study. Patients who had spine deformity, contra-indication for regional anaesthesia were excluded from the study.
The primary objective was correlation of skin epidural distance with position of the patient. The secondary objectives were correlation of skin epidural distance with age, weight, height, BMI and abdominal girth of the patient and correlation of posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient.
The total number of cases was decided as per study conducted by Hamza J et al,[7] so as to detect a difference of 10 percent in the skin epidural distance in lateral vs. sitting position. The number of cases required per group with an alpha error of 0.05 and power of 80 percent was 61.
After taking approval from Institutional review board and written informed consent from the patients, anaesthetic procedure of subarachnoid block (SAB) was explained to them. All patients were advised premedication with Tab. Alprazolam 0.5 mg at night and 2 hours before surgery along with sips of water. Using random numbers table, patients were allocated into one of the following two groups: Group L (SAB with patient in lateral position) and Group S (SAB with patient in sitting position).
Prior to the SAB, the age, height, weight and abdominal girth at the umbilicus were noted. In the operating room, all monitors were attached, baseline parameters measured and intravenous line secured. Subarachnoid block and further observations were performed by an investigator who was blinded to the details of the patient characteristics.
Under all aseptic conditions, skin was locally anaesthetised in L3-L4 interspace using 25G hypodermic needle. A 23 G disposable Quincke Babcock spinal needle of length 10.78 cm (measured with stillette removed) was inserted perpendicular to skin at L3-4 via the midline approach. After passing through the skin and the interspinous ligament, the stillette of the needle was removed. The 5ml glass syringe available in the set was attached to the spinal needle holding 3-5 ml of air. The epidural space was then identified using loss of resistance to air in the syringe. Not more than 2 ml of air was pushed in. The distance from the skin to the hub of the spinal needle at that point of reaching epidural space was marked on the sterile corrugated rubber drain with a sterile blade and designated as D1.The needle was then advanced further to pierce subarachnoid space. The distance from the skin to the hub of spinal needle was marked as D2 on the sterile corrugated rubber drain.
0.5% hyperbaric bupivacaine was administered via spinal needle in subarachnoid space, the volume of drug being decided by the level of surgical anaesthesia required and the duration of surgery. Skin epidural distance and skin subarachnoid distances were calculated by deducting the calculated distances D1 and D2 respectively from the total length of the spinal needle with stillette removed.
Posterior epidural space width which is the distance between the duramater and the ligamentum flavum was calculated by taking a difference of skin epidural and skin subarachnoid distance, also known as Tip to Tip distance.
Skin Epidural space Distance (SED): Length of needle minus D1.
Skin Subarachnoid Distance (SSD): Length of needle minus D2.
Posterior Epidural space depth (PESD): SSD – SED.
The results were subjected to statistical analysis. Descriptive statistics that is mean and standard deviation have been used and t test was applied for continuous variables. Linear regression analysis was performed to calculate pearson correlation with statistical significance. Multiple regression analysis was done to know degree of variability. P<0.05 was considered significant.
Result
Power analysis was performed using sample size of 100 in each group. Alpha error was taken as 0.050. Power of the study is 0.897.
Mean skin epidural distance was 4.30 ±0.57 in lateral position and 4.05 ± 0.57 in sitting position, the difference being statistically significant. (P= 0.002)
There was no significant correlation between skin epidural distance and age or height of the patient in both sitting and lateral position. However, skin epidural distance was found to be significantly correlated with weight, BMI and abdominal girth of the patient in both sitting and lateral position (P <0.05).
|
|
Pearson correlation |
P value |
r 2 value |
|
Age |
-0.087 |
0.389 |
0.007 |
|
Weight |
0.464 |
<0.001 |
0.216 |
|
Height |
0.138 |
0.172 |
0.019 |
|
BMI |
0.44 |
<0.001 |
0.193 |
|
Abdominal Girth |
0.544 |
<0.001 |
0.296 |
|
|
Pearson Correlation |
P value |
r 2 value |
|
Age |
0.031 |
0.756 |
0.001 |
|
Weight |
0.403 |
<0.001 |
0.162 |
|
Height |
0.167 |
0.098 |
0.028 |
|
BMI |
0.332 |
<0.001 |
0.110 |
|
Abdominal Girth |
0.412 |
<0.001 |
0.170 |
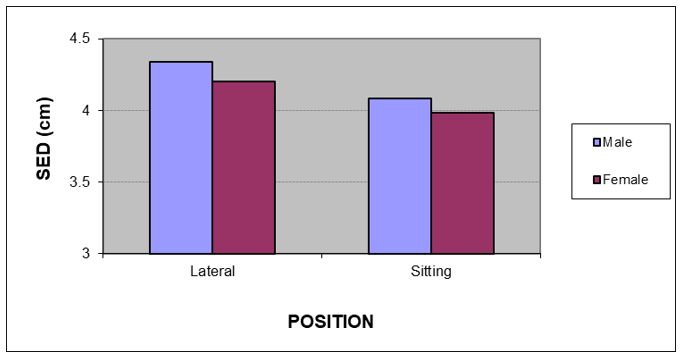
The skin epidural distance was more amongst males in comparison to females in both lateral and sitting positions, but the difference was not statistically significant, P value 0.293 (P: >0.05)
Mean PSED was 0.468+14 cm in lateral position and 0.459+0.14 cm in sitting position, the difference being statistically insignificant.
There was no significant correlation between posterior epidural space depth and age, weight, BMI or abdominal girth of the patient in both sitting and lateral position. However, posterior epidural space depth was found to be significantly correlated with height of the patient in both sitting and lateral position (P< 0.05)
|
|
Pearson Correlation |
P value |
r 2 value |
|
Age |
-0.052 |
0.61 |
0.002 |
|
Weight |
0.087 |
0.338 |
0.008 |
|
Height |
0.246 |
0.014 |
0.061 |
|
BMI |
-0.022 |
0.825 |
0.001 |
|
Abdominal Girth |
0.134 |
0.183 |
0.018 |
|
|
Pearson Correlation |
P value |
r 2 value |
|
Age |
-0.012 |
0.903 |
0.0001 |
|
Weight |
0.156 |
0.122 |
0.024 |
|
Height |
0.307 |
0.002 |
0.094 |
|
BMI |
0.001 |
0.989 |
0.000001 |
|
Abdominal Girth |
0.088 |
0.383 |
0.008 |
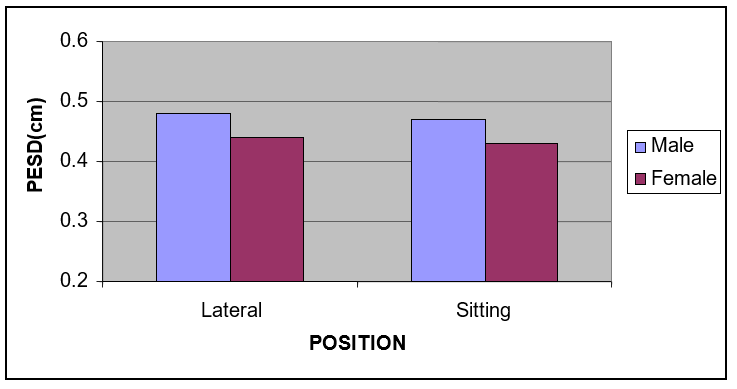
The posterior epidural space depth was more amongst males in comparison to females in both lateral and sitting positions, but the difference was not statistically significant (P >0.05).
Discussion
The present study was performed to measure the skin-epidural distance and posterior epidural space depth in an attempt to correlate these distances with age, sex, weight, height, BMI, abdominal girth and position of the patient, with the hope that the incidence of post dural puncture headache (PDPH) may be reduced by guidelines that would emerge from the study.
In our study we have chosen loss of resistance (LOR) technique as there are less chances of dural puncture with LOR technique than with hanging drop. This is in accordance with a study conducted by V.L.H Hoffmann et al.[8] which found out that the chances of dural puncture are less with LOR technique. This is because there was a greater width of epidural space when LOR technique is used, due to air injection, though air injected is small in volume.
The skin epidural distance in our study varied from 2.89 to 5.92 cm with the mean of 4.30 ± 0.57cm in lateral and 4.05 ± 0.57 cm in sitting position. 85 percent of the patients in lateral and 80 percent in sitting position had distance in the range of 3.5-5 cm.
This is similar to skin epidural distance measured via loss of resistance technique by various authors. Chen K P et al.[9] and Watts R W et al.[10] found distance from skin as 4.6 ± 0.6 cm and 4.6 ± 1.7 cm respectively. Sang Chul Lee et al[11] found mean skin epidural distance as 4.75 ± 1.7 cm using 22G spinal needle.
In our study, there was a positive correlation of skin epidural distance with weight, BMI and abdominal girth of the patient.
In a study by Adegboye MB et al[6] the mean skin epidural distance was 4.60±0.83 cm with a range of 3cm-8cm. The distance was significantly influenced by BMI and weight with both having positive correlation and P value of 0.001 and 0.004 respectively similar to our study.
There was significant positive correlation (r: 0.464 in lateral and 0.403 in sitting) between skin epidural distance and weight of the patient in both lateral and sitting positions (P <0.001). Wong JO et al,[3] Susan K et al,[12] Bevacqua BK et al,[13] Shiroyama K et al,[14] Upton PM et al[15] and Sang Chul Lee et al[11] also found similar significant correlation of skin epidural distance with weight in various populations of patients.
Parekh A et al[16] studied the correlation between skin-epidural space distance with weight, age, and height in paediatric patients. Segal S et al[17] studied the correlation with skin epidural distance with weight in parturients. The mean distance from skin to lumbar epidural space was 5.4 cm. When tested in a multiple regression model, both body mass index and ethnicity significantly influenced the distance from skin to lumbar epidural space in parturients.
The anatomical layers through which the needle passes on its way to the epidural space include skin, subcutaneous tissue, supraspinous and interspinous ligaments and the ligamentum flavum. The subcutaneous tissue is the most variable of these layers. Therefore, fat occupying and enlarging the subcutaneous tissue may account for most of the variation in distance from skin to the epidural space with the weight of the patient
There was a significant correlation (r: 0.44 in lateral and 0.332 in sitting position) between BMI and skin epidural distance (P<0.001). Stamatakis E et al,[18] Chen KP et al[9] and Bahk JH et al[19] and Ravi KK [5] also showed a positive correlation with BMI. Watts RW et al[10] found a significant correlation between skin epidural distance and BMI in their non-obese patients and attributed it to distribution of fat. However, in obese patients of Watts RW et al,[10] the skin epidural distance correlated poorly with BMI. They hypothesized that the greater body mass is distributed disproportionately to areas other than the lower lumbar region in the obese and morbidly obese patients. As most of our patients were non-obese, the correlation between skin epidural distance and BMI was significant.
Skin epidural distance in our study also found to be correlated (r: 0.544 in lateral and 0.412 in sitting position) significantly with the abdominal girth of the patient (P<0.001). Bahk JH et al[19] also found significant correlation. The increase in skin epidural distance with abdominal girth occurs because increased abdominal girth indicates a distribution of fat around the abdomen and lumbar region. The needle thus has to traverse greater distance before reaching epidural space.
There was no significant correlation of skin epidural distance with the height of the patient (P: 0.172 in lateral and 0.098 in sitting position). Wong JO et al,[3] Susan K et al,[12] Lau HP[20] and Watts RW el al[10] also found no significant correlation with height of the patient. Chen KP[9] however found significant correlation of skin epidural distance with the height.
Of the two postures used for performing the block, the skin epidural distance was found to be significantly more in lateral position than in sitting position (P: 0.002). The most probable cause of this difference is stretching and thus thinning of the tissues in the needle path in sitting position, a finding substantiated by Hamza et al[7] as well.
Posterior epidural space is the area of concern for the anesthesiologist as it is the space in which epidural catheters are inserted and epidural drug is being given. The measurement of skin epidural distance will prevent many complications like accidental dural puncture and headache. Also, measurement of posterior epidural space depth (PESD) and its correlation with various physical parameters of the patient help to determine the distribution, onset of action and absorption of the anaesthetic solutions used in the epidural space, and will therefore lessen the complication rate of epidural anaesthesia. Variability in the posterior epidural space will also affect the successful application of combined single dose spinal and catheter epidural anaesthesia.[5] Therefore, knowledge about the range of posterior epidural space gains special significance when choosing the length of spinal needles used for subarachnoid portion of the anaesthesia. Despite the importance of epidural space depth, little is known about the magnitude and range of values encountered and its correlation with various physical parameters.
The mean posterior epidural space width as derived from our study varied from 0.28-0.97 cm, with mean of 0.468 ± 0.12 cm in lateral and 0.459 ± 0.14 cm in sitting position. 83 percent in lateral and 88 percent of patients in sitting position had posterior epidural space depth in the range of 0.31-0.6 cm. The distance had been calculated by various authors both clinically and radiographically by employing different techniques.
Bevacqua BK et al[13] used 17 G Tuohy needle to pierce duramater after measuring skin epidural distance. They found that the mean posterior epidural depth varied from 2 – 2.5 mm with the mean of 6.9 ± 4 mm.
The depth of the posterior epidural space showed a significantly positive correlation with the height of the patient (P: 0.014 in lateral and 0.002 in sitting position). It was unrelated to other patient characteristics such as weight, BMI and abdominal girth that had shown significant correlation with skin epidural distance. No significant correlation of posterior epidural space depth was found with age similar to skin epidural distance. The posterior epidural space depth was comparable amongst males and females (P: 0.216 in lateral and 0.17 in sitting position).
Hoffmann et al[8] showed positive significant correlations between the epidural space width and the patient's height, weight-to-height ratio and body mass index. Sang Chul Lee et al[11] however showed no correlation of posterior epidural depth with any of the physical parameters. The mean posterior epidural space depth in our study was comparable in sitting and lateral position (P: 0.639).
Taman HI et al[21] in Egyptian population, Prakash S et al[22] and Hazarika R et al[23] in Indian population studied the correlation of skin subarachnoid distance with age, sex, weight and BMI of the patients. They observed that there is positive correlation with skin subarachnoid distance with sex and BMI of the patients. None of them have correlated posterior epidural space depth with the physical characteristics of the patient.
Conclusion
Familiarity with expected depth of entrance into epidural space and depth of posterior epidural space for given physical parameters of a patient can be of some extra help during performance of central neuraxial blocks. The findings of this study are a step in that direction.
Source of Funding
None.
Conflict of Interest
The author declares no conflict of interest.
References
- Savolina E, Pandya J, Greenblatt S, Conover S. Anatomy of the human lumbar epidural space: New insights using CT-Epidurography. Anesthesiology. 1988;68:217-20. [Google Scholar]
- Sutton D, Linter S. Depth of extradural space and dural puncture. Anaesthesia. 1991;46:97-8. [Google Scholar]
- Wong J, Chang C. The distance from the skin to the epidural space in general population. Ma Zui Xue Za Zhi. 1990;28:63-8. [Google Scholar]
- Bala M, Chhikara M, Deepika, Kaur K, Bansal T, Naz S. Correlation of distance from skin to lumbar epidural space with age and height of patients. Int J Adv Med. 2020;7:1846-9. [Google Scholar]
- Ravi K, Kaul T, Kathuria S, Gupta S, Khurana S. Distance from Skin to Epidural Space: Correlation with Body Mass Index (BMI). J Anaesthesiol Clin Pharmacol. 2011;27:39-42. [Google Scholar]
- Adegboye M, Bolaji B, Ibraheem G. The Correlation Between Body Mass Index On The Length From Skin To Lumbar Epidural Space In Nigerian Adults. J West Afr Coll Surg. 2017;7:113-27. [Google Scholar]
- Hamza J, Smida M. Parturient’s position during epidural puncture affects the distance from skin to epidural space. J Clin Anesth. 1995;7:1-4. [Google Scholar]
- Hoffmann V, Vercauteren M, Vreugde J, Hans G, Coppejans H, Adriaensen H. Posterior epidural space depth: safety of the loss of resistance and hanging drop techniques. Br J Anaesth. 1999;83:807-9. [Google Scholar]
- Chen K, Poon Y, Wong C. The depth to the epidural space. Ma Zui Xue Za Zhi. 1989;27:353-6. [Google Scholar]
- Watts R. The influence of obesity on the relationship between body mass index and the distance of the epidural space from the skin. Anaesth Intens Care. 1993;21:309-10. [Google Scholar]
- Lee S, Kim S. The Width of the Epidural Space Measured during Spinal Anesthesia. Korean J Anestheisol. 1993;26:520-6. [Google Scholar]
- Palmer S, Abram S, Maitra A, Colditz J. Distance from the skin to the lumbar epidural space in an obstetric population. Anesth Analg. 1983;62:944-6. [Google Scholar]
- Bevacqua B, Haas T, Brand F. A clinical measure of the posterior epidural space depth. Reg Anesth. 1996;21:456-60. [Google Scholar]
- Shiroyama K, Izumi H, Kubo T, Nakamura R. Distance from the skin to the epidural space at the first lumbar interspace in a Japanese obstetric population. Hiroshima J Med Sci. 2003;52:27-9. [Google Scholar]
- Upton P, Carrie L, Reynolds K. Epidural insertion: how far should the epidural needle be inserted before testing for loss of resistance?. Int J Obstet Anesth. 1992;1:71-3. [Google Scholar]
- Parekh A, Dias R, Dave N. Correlation between skin-epidural space diatance with weight, age, and height in paediatric patients. Indian J Anaesth. 2019;63:143-6. [Google Scholar]
- Segal S, Beach M, Eappen S. A multivariate model to predict the distance from the skin to the epidural space in an obstetric population. Reg Anesth. 1996;21:451-5. [Google Scholar]
- Stamatakis E, Moka E, Siafaka I, Argyra E, Vadalouca A. Prediction of the distance from the skin to the lumbar epidural space in the Greek population, using mathematical models. Pain Pract. 2005;5:125-34. [Google Scholar]
- Bahk J, Kim J, Lee J. Computed Tomographic study of lumbar (L3-4) epidural depth and its relationship to physical measurements in young adult men. Reg Anesth. 1998;23:262-5. [Google Scholar]
- Lau H. The distance from the skin to the epidural space in a Chinese patient population. Ma Zui Xue Za Zhi. 1989;27:261-4. [Google Scholar]
- Taman H, Farid A, Abdelghaffar W. Measuring skin to subarachnoid space depth in Egyptian population: A prospective cohort study. Anesth Essays Res. 2016;10:468-72. [Google Scholar]
- Prakash S, Mullick P, Chopra P, Kumar S, Singh R, Gogia A. A prospective observational study of skin to subarachnoid space depth in the Indian population. Indian J Anaesth. 2014;58:165-70. [Google Scholar]
- Hazarika R, Choudhury D, Nath S, Parua S. Estimation of Skin to Subarachnoid Space Depth: An Observational Study. J Clin Diagn Res. 2016;10:6-9. [Google Scholar]
How to Cite This Article
Vancouver
Gupta A, Singh F, Mandhyan R, Gupta A. Correlation of skin epidural distance and posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient: A prospective randomised study [Internet]. Indian J Clin Anaesth. 2021 [cited 2025 Oct 15];8(3):361-366. Available from: https://doi.org/10.18231/j.ijca.2021.069
APA
Gupta, A., Singh, F., Mandhyan, R., Gupta, A. (2021). Correlation of skin epidural distance and posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient: A prospective randomised study. Indian J Clin Anaesth, 8(3), 361-366. https://doi.org/10.18231/j.ijca.2021.069
MLA
Gupta, Akhilesh, Singh, Farhat, Mandhyan, Rajani, Gupta, Anshu. "Correlation of skin epidural distance and posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient: A prospective randomised study." Indian J Clin Anaesth, vol. 8, no. 3, 2021, pp. 361-366. https://doi.org/10.18231/j.ijca.2021.069
Chicago
Gupta, A., Singh, F., Mandhyan, R., Gupta, A.. "Correlation of skin epidural distance and posterior epidural space depth with age, weight, height, BMI, abdominal girth and position of the patient: A prospective randomised study." Indian J Clin Anaesth 8, no. 3 (2021): 361-366. https://doi.org/10.18231/j.ijca.2021.069
