Introduction
Major abdominal surgeries are associated with moderate to severe pain which needs to be treated aggressively in the post-operative period and unmanaged pain may turn to chronic pain.1, 2
Following the first documentation of TAP block by Rafi et al.3 Continuous bilateral TAP block provides analgesia comparable to a thoracic epidural in patients undergoing abdominal surgeries.4
The ideal local anesthetic (LA), its dose, volume, and concentration for ultrasound-guided TAP block are not well defined in the literature.5
Materials and Methods
This study was conducted at a tertiary care center from December 2017 to November 2018 over a period of one year. Prior ethical permission was taken from the institutional ethical committee (No. NHMECJ/JPR/2017/07, dated 13.10.2017). This prospective, randomized, double-blind comparative study included 100 American Society of Anaesthesiologists (ASA) physical status I and II patients, bodyweight >50 kg, aged 18–65 years of either sex who had undergone various elective lower abdominal surgeries under spinal/general anesthesia.
Ropivacaine may achieve similar potency as compared to bupivacaine at higher doses for surgical anesthesia in peripheral nerve blocks.6 The equi-effective doses have been established to be Ropivacaine 0.5% and Bupivacaine 0.25%.7
We conceived this study to compare the analgesic efficacy of 0.5% Ropivacaine and 0.25% Bupivacaine in ultrasound-guided TAP Block in patients undergoing lower abdominal surgeries. Our primary objective was to assess the Pain score and duration of analgesia provided by the block. We also studied the total analgesic consumption in 24 hours postoperatively and complications associated with TAP block, if any.
Patients who had local pathology at the site of injection, patients belonging to ASA grade III or above, pregnant females, patients with bleeding disorders, and those who did not cooperate or refused to participate in the study were excluded. Patients with a history of drug abuse or those on medications for chronic pain were also excluded from the study.
After a thorough pre-anesthetic check-up, patients satisfying the eligibility criteria were selected. Patients were explained about the study protocol and written informed consent was taken from each of the 100 enrolled patients for participation in the study. Demographic data like age, gender, weight, body mass index (BMI) and ASA grade were recorded. Numeric Rating scale (NRS) 0–10 was also explained to the patients. Randomization was done by using computer generated random number sequence that were allocated using sequentially numbered opaque sealed envelopes. The patient and the outcome assessor were blinded in the study to avoid bias.
Patients were randomized on the day of surgery into one of the two groups A or B with 50 patients in each by using a computer-generated random number table. Patients in both the groups received USG guided TAP block with either of the following drugs: 0.5% Ropivacaine or 0.25% Bupivacaine after the completion of surgery. The block was performed either on one side or both sides depending on the surgical procedure and extent of abdominal wall incision.
All the patients were kept fasting for an optimal period. On arrival in the operating room, the standard ASA monitors were attached and baseline readings were noted. One peripheral intravenous cannula was secured and intravenous fluid was started. The patients were given spinal or general anesthesia based on the decision of consultant anaesthesiologists and the type of surgery.
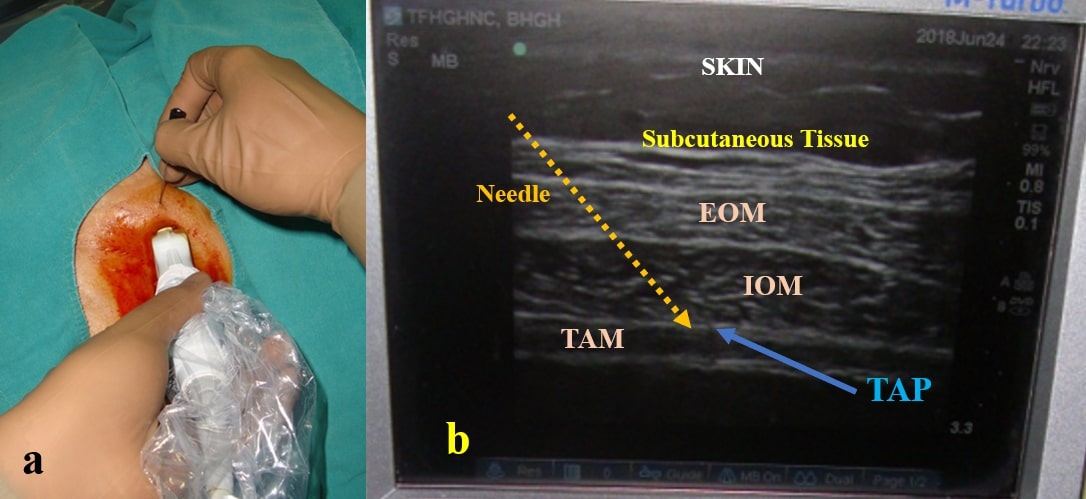
After completion of the surgery, all the patients received USG guided TAP block under aseptic precautions in the supine position. The blocks were performed by an experienced anesthesiologist. The linear probe (8-13 MHz, SonoSite, M-Turbo) of the USG machine (M-Turbo®, MicroMaxx, FujiFilm SonoSite Inc., USA) was used to identify the transversus abdominis plane. TAP Block was performed with a 22G Quincke’s spinal needle at the midaxillary line (Figure 2). Patients in group A received 20 ml of 0.5% Ropivacaine Hydrochloride (Ropin, Neon Laboratories Ltd., India) and patients in group B received 20 ml of 0.25% Bupivacaine Hydrochloride (Anawin, Neon Laboratories Ltd., India).
Figure 2
a): Aseptic technique of usg guided TAP block. b): Ultra sound image showing the transversus abdominis plane
Following the performance of the TAP block, patients’ heart rate(HR), noninvasive blood pressure(NIBP), and oxygen saturation (SpO2) were recorded at 0, 10, 20, 30 minutes till 1 hour in the recovery room. The vitals were also observed in the postoperative ward at 1, 2, 4, 8, 12, 18, 20 & 24 hours. Hypotension was defined as a 20% decrease in systolic blood pressure from the baseline. Bradycardia was defined as HR < 60 beats/min. Tachycardia was defined as HR > 100 beats/min.
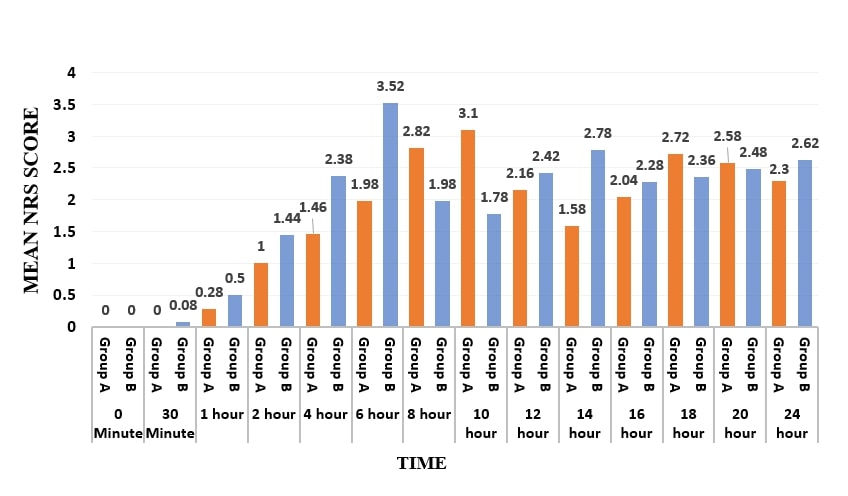
The patient's perception of pain was assessed using NRS (0–10), with 0 being no pain at all and 10 being the worst pain imaginable. NRS score was measured at 0 min, 15 min, 30 min, 1hr, and then every second hourly till 24 hours. All the assessment and appropriate intervention was done by an anesthesiologist who was blinded for the drug given in the block.
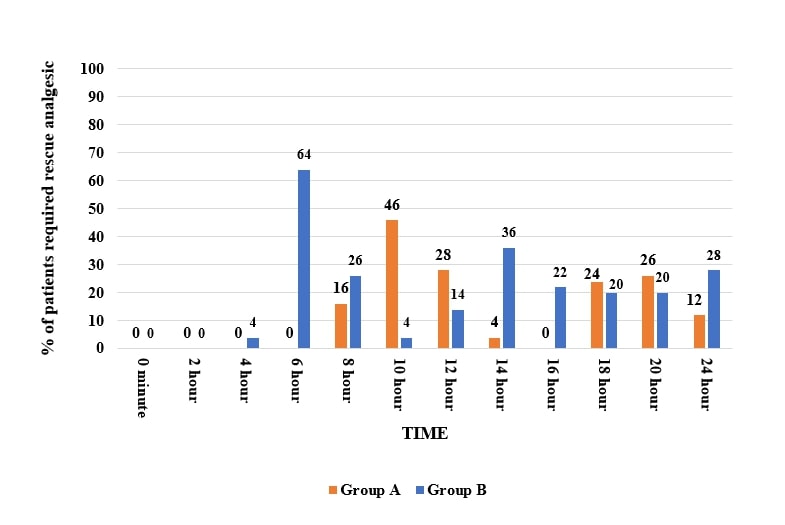
Pain relief was estimated from the total number of rescue analgesics consumed in the first 24 hours after surgery. Rescue analgesia was given at the NRS score of >3. The total duration of analgesia was defined as the time from commencement of block to the patient's first request for rescue analgesia (VAS>3). Injection Diclofenac sodium (Dynapar AQ, Troikaa Pharmaceuticals Ltd, Ahmedabad) 75 mg IV infusion was given as rescue analgesia. After consumption of two doses of intravenous Diclofenac, infusion of Tramadol Hydrochloride 100mg along with intravenous Ondansetron 4mg was given as the third dose of analgesic. Patients consuming more than 3 analgesics in the first 24 hours were considered as a case of block failure and were thus not considered for statistical analysis.
All patients were monitored for side effects like nausea, vomiting, and LA systemic toxicity. Patient satisfaction score was also collected regarding the postoperative pain relief in the first 24 hours following surgery. Patients were asked to score their level of satisfaction on a four-point Likart’s scale: 1= totally dissatisfied, 2= moderately dissatisfied, 3= reasonably satisfied, 4=totally satisfied with pain relief.
The sample size was calculated at 80% study power and an alpha error of 0.05 assuming a standard deviation of 5.13 hours in the duration of analgesia as found in the reference study.7 For the minimum detectable mean difference in duration of analgesia of 3 hours, 45 patients in each group were required. Considering the potential drop-outs and 10% attrition rate, 100 patients were included in our study.
All statistical calculations were done using computer programs Microsoft Excel 2019 (Microsoft Corporation, NY, USA) and SPSS version 25 (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA). Categorical data, i.e., ASA grade, type of surgery, and the incidence of adverse events were presented as percentages and proportions. These data were compared in two groups, and the difference in the proportion was inferred by Pearson's chi-square test. Demographic data (age, weight), duration of surgery, NRS score, the total duration of analgesia were expressed as mean ± standard deviation. These data were compared between the two groups, and the statistical tests were conducted using student's t-test, chi-square test, or fisher's exact test whichever was applicable. For significance, P < 0.05 was considered as significant for both types of data.
Results
We recruited 50 participants in each group and there were no dropouts. Thus, final data analysis was performed on 100 patients (Group A = 50 patients, Group B = 50 patients).
Both the groups were comparable in terms of demographic profiles (age, gender, ASA grade, and body weight). (Table 1)
Table 1
Demographic profile
Most of the patients are in <30 years age group (38%). Both groups included patients for similar types of surgeries and no statistically significant difference was observed(p=0.304). (Table 2)
Table 2
Types of surgery
No statistically significant difference was observed in hemodynamic variables before and after the performance of the TAP block in between two groups. (Table 3)
Table 3
Pre block and post block vitals
The total duration of analgesia was longer in group A as compared to group B. (Table 4)
Table 4
Rescue analgesics used within the first 24 hours and duration of analgesia
The total number of analgesic doses used was higher in group B as compared to group A.(p<0.001) (Table 4) In group B 42% of patients required Tramadol as 3rd rescue analgesia. None of the patients needed more than 3 rescue analgesics within the first 24 hours.
Mean NRS score was higher for group B at 2nd, 4th, 6th, and 14th hour with a p-value of <0.001 whereas in group A higher score was observed at 8th and 10th hour following the performance of the block. A statistically significant difference in the pain scores was observed at different time intervals between the two groups (Figure 3)
The rescue analgesic consumption in most patients of group A was at 10th hour and of group B was at 6th hour following the performance of ultrasound-guided TAP block. The difference was found to be statistically significant at different time intervals 6th, 10th,14th & 16th hour. (p< 0.001). (Figure 4)
In group A 56% patients were totally satisfied whereas in group B 64% were reasonably satisfied with the pain relief. Chi-square test was applied between the groups and was statistically significant. No patient was found to be totally dissatisfied in both groups.
None of the patients experienced any complications like local anesthetic systemic toxicity (LAST), liver trauma, bowel perforation, local infection, hematoma, or femoral nerve palsy.
Discussion
The results of this randomized, double-blind trial demonstrated that a single-shot ultrasound-guided TAP block provides effective analgesia as a component of multimodal analgesia for patients undergoing lower abdominal surgeries. We observed statistically significant differences between Group A and B with respect to the NRS score, the requirement of rescue analgesics, and the mean duration of analgesia. The quality of analgesia was better and the requirement of rescue analgesics was lower in patients receiving 0.5% Ropivacaine in TAP block as compared to 0.25% Bupivacaine. We did not observe any significant complications in both groups.
In a recent meta-analysis, Peltrini et al. have evaluated the efficacy of TAP block in colorectal surgery and concluded that it provides effective analgesia and reduces postoperative opioid consumption in the first 24 hours without any significant complications.8
Different concentrations of the same LA and/or different local anesthetics have been used in the TAP block. Raghunath et al. observed that 0.5% Ropivacaine provided a longer duration of analgesia as compared to 0.25% Levobupivacaine in patients undergoing lower abdominal surgeries.9 Sinha et al. found that 0.375% Ropivacaine was better than 0.25% Bupivacaine in providing analgesia in patients undergoing laparoscopic cholecystectomies but only up to one hour postoperatively.10 They observed significantly lower pain scores in the Ropivacaine group. But the cumulative rescue analgesic requirement was similar in 24 hours postoperative period. In our study, we observed that 0.5% Ropivacaine provided a longer duration of analgesia and a lesser consumption of rescue analgesic in the first 24 hours as compared to 0.25% Bupivacaine. Similar findings were noted in the study conducted by Sharma et al. comparing the analgesic efficacy of 0.25% bupivacaine with 0.5% Ropivacaine in TAP block.7
We observed that the duration of analgesia was significantly higher in patients who received ropivacaine in the TAP block. Most of the patients experienced good pain relief in the early postoperative period for up to 6 hours in both groups. We used diclofenac sodium and tramadol hydrochloride as rescue analgesics as compared to opioids in other studies. Our findings are similar to the meta-analysis conducted by Baeriswyl et al.11 on ultrasound-guided TAP Block for various abdominal surgeries in adult patients. They observed that ultrasound-guided TAP block reduced intravenous morphine consumption at 6 hours postoperatively irrespective of the type of surgery, timing of injection or block approach adopted.11
The majority of our study population (53%) consisted of patients undergoing lower segment cesarean section (LSCS). TAP block is an effective analgesic technique in postoperative pain management for LSCS to facilitate early ambulation and infant care (breastfeeding, maternal-infant bonding, etc.).12 In our study, we observed a statistically significant between the groups in the total number of rescue analgesics consumed by patients undergoing LSCS. Patients who received 0.25% Bupivacaine in TAP block required more analgesics in the first 24 hours.
The assessment of patient satisfaction is an important tool to monitor the quality of analgesia in the postoperative period. In a retrospective analysis, Kadam et al. observed no significant differences in patient satisfaction scores following TAP block versus LA infiltration in laparoscopic cholecystectomy.13 The assessment was over a telephonic interview and the time varied from 30 to 180 days, which might have chances of bias. We have prospectively assessed the patient satisfaction score using the Likert scale. We found that patients in the Ropivacaine group were more satisfied as compared to the Bupivacaine group.
Although complications are rare with ultrasound-guided TAP block, unintentional peritoneal puncture, bowel hematoma, liver laceration, LAST and accidental femoral nerve palsy are reported in the literature.14 The use of ultrasound helps to identify the correct interfacial plane for LA deposition, needle advancement, and spread of LA; thereby reducing failure rate, and minimizing complications.3 It also helps to avoid intramuscular or intravascular injection of large volumes of LA. In our study, blocks were performed under ultrasound guidance by an experienced anesthesiologist and we did not encounter any technical complication.
Our study has a few limitations. The level of sensory block was not assessed following the TAP block. We did not evaluate the dynamic pain score which needs to be optimized for early mobilization. The serum concentrations of Ropivacaine and Bupivacaine were not estimated. We recommend the use of ultrasound-guided TAP block as a component of a multimodal analgesic regimen for patients undergoing lower abdominal surgeries.
Conclusion
Ultrasound-guided TAP block is a safe, effective, and important component of multimodal analgesia technique for postoperative analgesia in patients undergoing lower abdominal surgeries without any significant adverse effects. In comparison to 0.25% Bupivacaine, TAP block with 0.5% Ropivacaine provided a longer duration of analgesia, better patient satisfaction, and lesser consumption of systemic analgesics.