- Visibility 30 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijca.2021.035
-
CrossMark
- Citation
Comparing efficacy of ibutilide and amiodarone for cardioversion in atrial fibrillation after coronary artery bypass grafting- A prospective and randomized study
- Author Details:
-
Mukesh Godara *
-
Pradeep Kumar Goyal
-
Sonu Kumar Goyal
-
Dharmendra Carpenter
Introduction
AF is a supraventricular tachyarrhythmia diagnosed through irregular atrial activities and disappearance of atria mechanical function. In electrocardiogram (ECG), AF appears as quick vibrating waves replaced by P-waves and often accompanied by quick and irregular ventricular response. During AF, multiple foci can serve as pacemakers with rapid irregular firing resulting in randomly irregular atrial depolarization at a rate of 350-450 per minute. The electrocardiogram is notable for an uneven irregular baseline without any recognizable P wave due to the chaotic atrial depolarization and normal QRS complexes.[1] AF is a relatively common arrhythmia that may be observed in otherwise normal subjects and also in those patients with rheumatic heart disease, ischemic heart disease, thyrotoxicosis and hypertension.[2], [3] A frequent postoperative complication of most types of cardiac surgeries, AF occurs in wide range of incidence between 10 and 60% in those undergoing CABG procedures.[4], [5]
The occurrence of postoperative AF has been associated with prolonged length of stay; ICU admission; a greater need for re-intubation; persistent congestive heart failure (CHF); stroke and increased overall costs. Typical conditions associated with AF include hypotension caused by rapid ventricular response, myocardial infarction and death. Additionally patients with AF are older adults with co-existing conditions [6], [7] such as compromised ventricular functions, hypertension, diabetes mellitus, renal insufficiency, peripheral vascular disease, a history of congestive heart failure or myocardial infarction, dyspnoea and cerebrovascular problems.[8], [9], [6], [7], [10], [11], [12], [13], [14] So AF in postoperative CABG patients has to be managed properly to decrease both patient morbidity and health care cost. During the perioperative period, management of patient experiencing AF is often times difficult as occurrences vary in degree of intensity and frequency. Various pharmacologic measures have been proved to be effective for treatment of AF apart from electrical cardioversion.
Ibutilide fumarate is a methane sulfonilide antiarrhythmic agent which belongs to class III antiarrhythmic agents and is approved for the conversion of atrial fibrillation and atrial flutter to sinus rhythm. Ibutilide prolongs the refractory period at the atrial and ventricular levels by activating a slow inward sodium current.[15], [16]
Amiodarone is another class III antiarrhythmic agent which is structurally benzofuran derivative and was initially introduced as an anti-anginal drug. Amiodarone prolongs repolarization and refractoriness in the SA node, in atrial and ventricular myocardium, in the AV node and in His-purkinje system.
Currently amiodarone is being used as a treatment of AF in most of the cardiac centres worldwide. But as the literature suggest the ibutilide also has promising results in the treatment of atrial arrhythmia with reduced rate of complications. So considering the paucity of information regarding comparative effects of ibutilide in postoperative CABG patients this study was carried out to compare the efficacy of Ibutilide and Amiodarone for Cardioversion in Atrial Fibrillation after CABG.
Materials and Methods
After the approval of institutional ethics committee (IEC) and taking informed consent 80 postoperative CABG patients, who developed AF, were randomly allocated to two groups. Sample size is calculated at 80% study power and alfa error of 0.05 assuming standard deviation of 405 minutes in mean time to conversion of atrial fibrillation to sinus rhythm in ibutilide group as found in reference study. (Bernard et al.)[17] For minimum detectable mean difference of 300 minutes in time to conversion from atrial fibrillation to sinus rhythm, 29 patients in each group are required as sample size for present study which is further enhanced and rounded off to 40 patients in each group as final sample size expecting 20% dropouts or attrition. Randomization was done using computer generated random numbers which were then sealed in opaque envelopes.
One group (n=40) received ibutilide 0.008mg/kg over 10 minutes at the onset of atrial fibrillation. After 10 minutes if sinus rhythm was not achieved the same dose of 0.008 mg/kg was repeated over 10 minutes. If sinus rhythm was achieved within 4 hrs of second dose then the patients were watched for any side effects or recurrence of atrial fibrillation. If sinus rhythm was not achieved in 4 hrs of second dose, the patient was administered bolus amiodarone 5 mg/kg over 30 minutes followed by 0.3 mg/kg/hr for next 24 hrs. Other group (n=40) received amiodarone 5 mg/kg over 30 minutes at the onset of atrial fibrillation. This was followed by amiodarone 0.3 mg/kg /hr for 24 hrs if sinus rhythm was achieved. Baseline vital parameters (pulse rate, systolic and diastolic blood pressure), ECG, SpO2 were recorded.
After administration of drugs all patients were monitored for any rhythm or vital changes. Vital parameters were noted at onset of AF (0 min),10min., 30min, 60min,120min,180min, 240min, 24hrs and at conversion to sinus rhythm. ECG was recorded at the onset of atrial fibrillation, just after conversion to sinus rhythm, 4 hrs after drug administration and at 24 hrs after drug administration.
Statistics
Unpaired t-test, Paired t-test were used for analysis of continuous variables; while Nominal/Categorical variables were analysed by using Chi square test / Fisher exact test. P value <0.05 was taken as significant. MedCalc.16.4 version software was used for all statistical calculation.
Results
There were no significant statistical differences between the groups with respect to demographic data and patient characteristics. Base line vitals were comparable in both the groups and were statistically insignificant. The time of onset of atrial fibrillation was comparable in both group and was statistically insignificant.
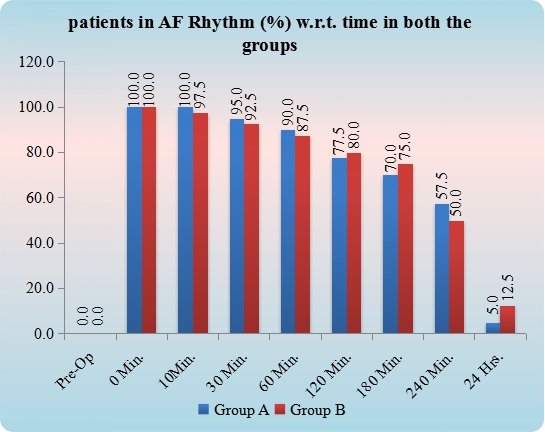
The mean time of conversion to sinus rhythm in group A was 382.85 minutes and in group B was 492.30 minutes. These data for conversion time in both groups were statistically insignificant. (p value= 0.235). The cardioversion rate at 4hrs in group A was 42.5% and in group B was 50%. At 24 hrs cardioversion rate in group A was 95% and in group B was 87.5%. These results were statistically insignificant. (p value > 0.001 at 4 hrs and 24 hrs)
|
S. No. |
Parameters |
Group A N=40 |
Group B N=40 |
P value |
|
1 |
Mean Age (Yr) |
58.93 ± 9.49 |
59.40 ± 8.27 |
0.812 |
|
2 |
Mean Weight (Kg) |
72.73 ± 7.9 |
70.78 ± 7.7 |
0.267 |
|
3 |
Gender |
|
|
0.422 |
|
Male |
29 (72.50) |
33 (82.50) |
||
|
Female |
11 (27.50) |
7 (17.50) |
||
|
4 |
Ejection Fraction (%) |
48.5± 8.40 |
47 ±7.91 |
0.414 |
|
5 |
POD of onset of AF (mean ± SD) |
1.78 ± 0.89 |
1.65 ± 0.92 |
0.539 |
|
S.No |
Vitals |
Group A (N= 40) Mean ± SD |
Group B (N=40 ) Mean ± SD |
P value |
|
1 |
Heart Rate (per minute) |
75.18 ± 7.07 |
73.80 ± 4.69 |
0.308 |
|
2 |
Systolic Blood pressure (mm Hg) |
119.35 ± 8.84 |
122 ± 8.25 |
0.170 |
|
3 |
Diastolic Blood pressure (mmHg) |
79.85 ± 5.31 |
78.80 ± 5.39 |
0.383 |
|
4 |
Mean Arterial Pressure (mmHg) |
93.02 ± 5.82 |
93.2 ± 6.03 |
0.891 |
|
5 |
Respiratory rate (per minute) |
17.24 ± 1.50 |
17.33 ± 1.23 |
0.729 |
|
6 |
SPO2 (%) |
99.5 ± 0.51 |
99.55 ± 0.50 |
0.659 |
|
Outcome variable |
Group A (N=40) |
Group B (N=40 ) |
P value |
|
Cardioversion rate at 4 hrs |
42.5% |
50% |
>0.001 |
|
Cardioversion rate at 24 hrs |
95% |
87.5% |
>0.001 |
|
Cardioversion Time (min) (MEAN ± SD) |
382.85 ± 335.03 |
492.30 ± 470.14 |
0.235 |
|
Increased requirement of inotropes (% of total patients) |
0 |
5 |
0.494 |
|
Increased requirement of ventilation |
None |
none |
NA |
|
Outcome variable |
Group A (N=40) |
Group B (N=40 ) |
||
|
Q-T Interval (in min) |
Baseline |
AT 24 hrs |
Baseline |
AT 24 hrs |
|
402.28 ± 13.75 |
401.83 ± 12.86 |
402.03 ± 15.90 |
401.2 ± 15.50 |
|
|
P value = 0.275 |
P value =0.071 |
Throughout the perioperative period the heart rate and mean arterial pressure were comparable in both the groups. Preoperative MBP in both groups were comparable. (p value= 0.891). Initially fall in MBP in both groups was observed but this was statistically insignificant. MBP recovered in both groups with the progression of study and was comparable and statistically insignificant all the time. (p value > 0.001).
None of patients in group A showed increased requirement of inotropes because of deteriorating hemodynamic condition but 2 patients in group B needed to increase the inotropes to stabilize the hemodynamic. This comparison in both groups was statistically insignificant. (p value= 0.494). None of the total 80 patients in both groups required prolonged or increased requirement of mechanical ventilation. Effect of both study drug on QT interval was found to be statistically insignificant. (p value group A =0.275, group B=0.071).
Discussion
Authors have used different dosages of ibutilide and amiodarone for treatment of atrial fibrillation. We selected the dose of 0.008mg/kg for ibutilide at onset of AF and to be repeated after 10 minutes if required, and the dose of 5 mg/kg of amiodarone over 30 minutes at the onset of atrial fibrillation followed by amiodarone 0.3 mg/kg /hr for 24 hrs. (Bernard et al.).[18]
Outcome variable
In our study, we observed that mean time of conversion in both groups was statistically insignificant. (p= 0.235) similar findings were demonstrated by Bernard et al.[18] whereas Dong Xio et al.[17] concluded that the mean conversion time for ibutilide group was significantly shorter than amiodarone group. This may be because they included both AF and atrial flutter (Af) in their study and because of more effectiveness of ibutilide for conversion of Af to sinus rhythm. Kafkas NV et al.[19] also showed that both drugs were equally effective in converting the recent onset atrial fibrillation to sinus rhythm.
At 4 hrs time and at 24 hrs time conversion rate in both groups was statistically insignificant (p= 0.432). Similar results were seen the study done by Bernard et al[18] and Madhuri et al[20] whereas Das M K et al23 showed that conversion rate for ibutilde group was significantly lower(55%) this may be because they included patients with AF of duration >24 hrs and < 3 months and with all type of cardiac surgery like valve surgery, CABG, or combined procedure and patients with LVEF <35% were also included. David R. Vinson et al[21] also showed that at 4 hrs period of acute onset of atrial fibrillation the cardioversion rate of ibutilide was 55%. Daniel J.Pallin et al.[22] showed that when used for AF or Af in emergency department ibutilide was associated with cardioversion rate of 55% at 4 hrs of onset.
Comparison of number of patients requiring increased dose of inotropes because of significant hypotension was statistically insignificant (p=0.494) whereas Bernard ED et al.[18] concluded that incidence of severe hypotension was more in amiodarone group this may be because they studied the patients developing AF within 3 hrs of cardiac surgery which itself may be more prone condition for hemodynamic instability.
In our study comparison of QT interval at baseline with at 24 hrs after drug administration was statistically insignificant, whereas Kathy Glatter et al.[23] observed that QT interval was prolonged after ibutilde administration. This may be because they included the patients who were having the history of long term AF.
During our study time none of our patient developed sustained or non-sustained polymorphic ventricular tachycardia whereas Marcus G Hennersdorf[24] observed in their study that 11% of patients developed non-sustained torsade de pointes tachycardia this may be because they included all the patient in intensive care unit developing atrial fibrillation or flutter irrespective of their primary diagnosis.
Hemodynamic parameters
Baseline values between two groups were comparable at all the times. Time of onset of AF was statistically insignificant. HR increased in both groups at onset of AF which is constant with pathophysiology of AF. HR in both groups was comparable and statistically insignificant at all the times except 120 min, and 240 mins. Mean HR was higher in group B except base line and at conversion to sinus rhythm. SBP, DBP, MBP decreased in both groups after onset of AF but returned near to base line after conversion to sinus rhythm. This fall was attributable to the pathophysiology of AF.
Limitations of the Study
We did our study only during the cardiac intensive care unit, but not in the ward or follow up.
In our study only first 24 hrs duration after onset of atrial fibrillation was monitored.
Conclusion
Our study demonstrates that ibutilide is as effective as amiodarone for restoration of sinus rhythm in postoperative CABG patients who developed AF in their postoperative ICU stay. Ibutilide may be superior to amiodarone in terms of hemodynamics and systemic side effects.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- JT Bigger, JC Bennett, F Plum. Cardiac arrhythmias. Cecil textbook of medicine 1996. [Google Scholar]
- LA Pires, AB Wagshal, R Lancey. Arrhythmias and conduction disturbances after coronary artery bypass graft surgery: epidemiology, management, and prognosis. Am Heart J 1995. [Google Scholar]
- LA Mendes, GP Connelly, PA Mckenney, PJ Podrid, LA Cupples, RJ Shemin. Right coronary artery stenosis: an independent predictor of atrial fibrillation after coronary artery bypass surgery. J Am Coll Cardiol 1995. [Google Scholar]
- N Erdil, E Gedik, K Donmez. Predictors of postoperative atrial fibrillation after on-pump coronary artery bypass grafting: is duration of mechanical ventilation time a risk factor. Ann Thorac Cardiovasc Surg 2014. [Google Scholar]
- C Dimmer, R Tavernier, N Gjorgov. Variations of autonomic tone preceding onset of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol 1998. [Google Scholar]
- PJ Stafford, S Kolvekar, J Cooper. Signal averaged P wave compared with standard electrocardiography or echocardiography for prediction of atrial fibrillation after coronary bypass grafting. Heart 1997. [Google Scholar]
- B Olshansky. Management of atrial fibrillation after coronary artery bypass graft. Am J Cardiol 1996. [Google Scholar]
- S Borzak, JE Tisdale, NB Amin. Atrial fibrillation after bypass surgery: does the arrhythmia or the characteristics of the patients prolong hospital stay?. Chest 1998. [Google Scholar]
- S Willems, C Weiss, T Meinertz. Tachyarrhythmias following coronary artery bypass graft surgery: epidemiology, mechanisms, and current therapeutic strategies. Thorac Cardiovasc Surg 1997. [Google Scholar]
- JP Mathew, R Parks, JS Savino. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. JAMA 1996. [Google Scholar]
- E Gaylard. Changing incidence of atrial fibrillation following coronary artery bypass grafting: aretrospective analysis. Br J Clin Pract 1996. [Google Scholar]
- SF Aranki, DP Shaw, DH Adams. Predictors of atrial fibrillation after coronary artery surgery: current trends and impact on hospital resources. Circulation 1996. [Google Scholar]
- E Pehkonen, E Honkonen, P Makynen. Stenosis of the right coronary artery and retrograde cardioplegia predispose patients to atrial fibrillation after coronary artery bypass grafting. Thorac Cardiovasc Surg 1998. [Google Scholar]
- AC Galloway, RJ Shemin, DD Glower. First report of the port access international registry. Ann Thorac Surg 1999. [Google Scholar]
- J Kaplan. . Kaplan's Cardiac Anaesthesia: The Echo Era 2017. [Google Scholar]
- S Dasgupta, I Dave, R Whitehill, P Fischbach. Chemical cardioversion of atrial flutter and fibrillation in the pediatric population with Ibutilide. Pacing Clin Electrophysiol 2020. [Google Scholar]
- D Xiao, D Wenhui. A meta-analysis. Ibutilide versus amiodarone in cardioversion efficiency and safety of atrial fibrillation and atrial flutter. 2011. [Google Scholar] [Crossref]
- EO Bernard, ER Schmid, D Schmidlin, C Scharf, R Candinas, R Germann. Ibutilide versus amiodarone in atrial fibrillation: a double-blinded, randomized study. Crit Care Med 2003. [Google Scholar]
- NV Kafkas, SP Patsilinakos, GA Mertzanos, KI Papageorgiou, JI Chaveles, OK Dagadaki. Conversion efficacy of intravenous ibutilide compared with intravenous amiodarone in patients with recent-onset atrial fibrillation and atrial flutter. Int J Cardiol 2007. [Google Scholar]
- M Nair, LK George, SKG Koshy. Safety and efficacy of ibutilide in cardioversion of atrial flutter and fibrillation. J Am Board Fam Med 2011. [Google Scholar]
- DR Vinson, N Lugovskaya, EM Warton, AM Rome, MD Stevenson, ME Reed. Ibutilide Effectiveness and Safety in the Cardioversion of Atrial Fibrillation and Flutter in the Community Emergency Department. Ann Emerg Med 2018. [Google Scholar]
- DJ Pallin, MS Link. Emergency Department Treatment of Atrial Fibrillation in Canada, Where Cardioversion Is Common. Ann Emerg Med 2017. [Google Scholar] [Crossref]
- K Glatter, Y Yang, K Chatterjee, G Modin, J Cheng, S Kayser. Chemical Cardioversion of Atrial Fibrillation or Flutter With Ibutilide in Patients Receiving Amiodarone Therapy. Circulation 2001. [Google Scholar]
- MG Hennersdorf, SM Perings, C Zühlke, UE Heidland, C Perings, MP Heintzen. Conversion of recent-onset atrial fibrillation or flutter with ibutilide after amiodarone has failed. Intensive Care Med 2002. [Google Scholar]
