Introduction
There are few studies done under ultrasound guidance for transversus abdominis plane block (TAP block) with 0.375% Ropivacaine and dexamethasone. Current study is designed to strengthen and add to existing body of literature on this topic that Dexamethasone when added as an adjuvant to Ropivacaine in ultrasound guided transversus abdominis plane block enhanced the duration of analgesia and decrease total rescue analgesic requirement as compared with Ropivacaine alone without causing any major systemic side effect. We did this study in our institute on patients posted for lower abdominal surgeries.
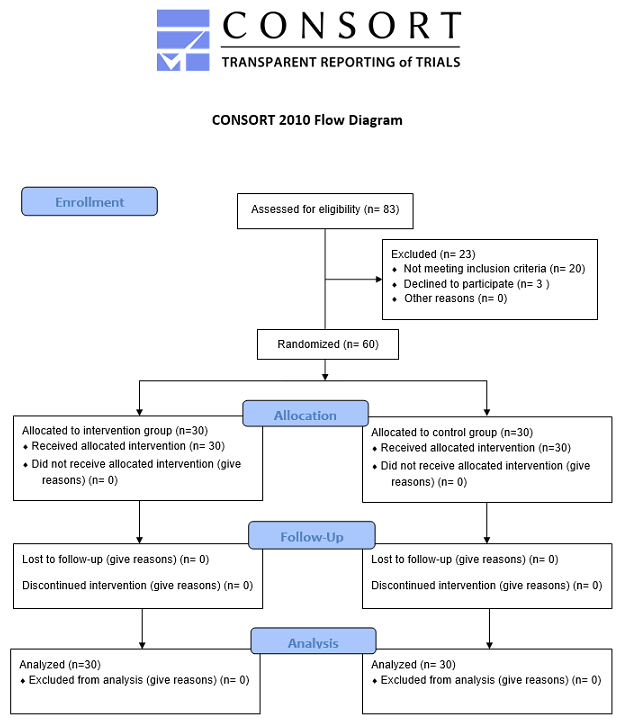
Materials and Methods
Following approval from the hospital ethics committee 60 ASA I or II patients of age 18-65 years undergoing lower abdominal surgeries were recruited to a prospective, randomized, double-blind, controlled study. Total 60 patients were divided into 2 groups of 30 each. Period of study was from May 2019 to June 2020.
Randomization was done by using computer generated random number sequence that were allocated using sequentially numbered opaque sealed envelopes. The patient and the outcome assessor were blinded in the study to avoid bias. Exclusion criteria included patients who were not able to provide consent for procedure or not willing to participate in the study, with known allergy to study group drugs, local pathology at the site of injection, on anticoagulation therapy or inherited or acquired coagulopathy, taking medicine for chronic pain, ASA class III or above, serum creatinine more than 1.2mg/dl and patients of diabetes mellitus.
Routine investigations (CBC, RFT, PT/INR, Blood sugar, Chest X-ray, ECG) and other specific investigations required, pertaining to the procedure and patient were done. The procedure was explained to the patients and written informed consent was taken.
On arrival in the operation theatre, each patient’s baseline heart rate, noninvasive blood pressure, electrocardiogram, respiratory rate and oxygen saturation were recorded and noted. An intravenous cannula was secured and appropriate IV fluid was started.
Anesthetic technique of ultrasound guided transversus abdominis plane block
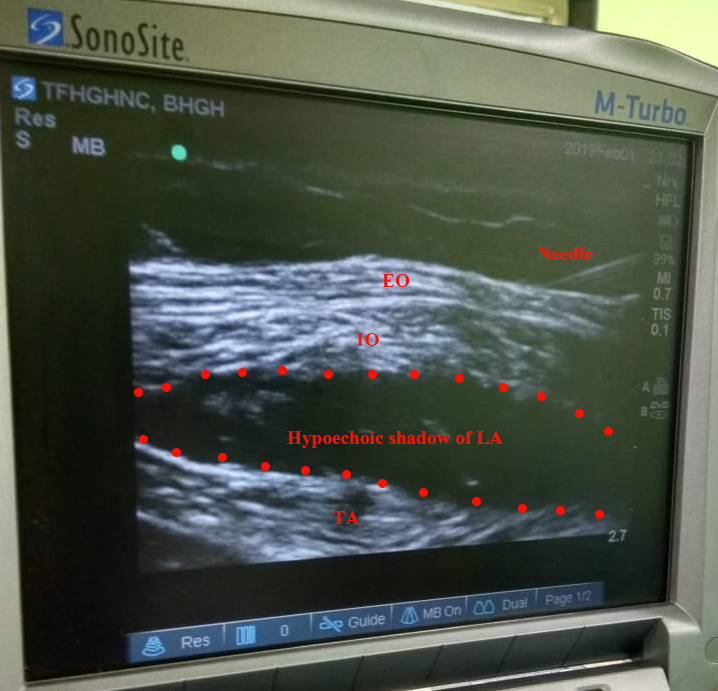
Patient was given spinal anesthesia with 0.5% hyperbaric bupivacaine for the surgery. After the completion of surgery, under all aseptic precautions transversus abdominis plane was identified using SonoSite M-Turbo ultrasonography machine with a linear probe of 6-13 Mhz frequency. From superficial to deep, the following structures are appreciated: skin and subcutaneous fat, external oblique, internal oblique, and Transversus abdominis muscles with their investing fascia & after ensuring full asepsis TAP Block was given using mid axillary approach in-plane technique for which 22 G Quincke’s needle was used.
Patients in group a received Injection Ropivacaine 0.375% 19ml with 1ml (4mg) Dexamethasone, total 20ml bilateral each side under ultrasonographic guidance. Patients in group B received Injection Ropivacaine 0.375% 19 ml with 1 ml normal saline, total 20ml bilateral each side under ultrasonographic guidance.
Figure 2
Sonographic View of Anatomy. EO-external oblique, IO-internal oblique, TAP-transversus abdominis plane, TA-transversus abdominis

Figure 3
Desired spread of the local anesthetic in transversus abdominis plane. EO-external oblique, IO-internal oblique, LA-local anesthetics, TA-transversus abdominis
Post block hemodynamic monitoring was done with Pulse rate, Systolic Blood Pressure, Diastolic Blood Pressure, Mean blood pressure, Respiratory Rate, Electrocardiogram and SpO2 at 0 minute, 10, 20, 30 minutes till 1 hour in the recovery room.
Hemodynamic effects including bradycardia and hypotension were observed in the respective ward at 1, 2, 4, 8, 12, 18 & 24hrs.
Patients were also monitored for side effects (nausea/vomiting, local anesthetic agent toxicity including numbness/paresthesia, seizures, respiratory depression) in the respective ward at 1, 2, 4, 8, 12, 18 & 24hrs.
Pain evaluation
Numeric rating scale score was used to assess pain intensity at 0min, 15, 30min, 1hr, 2, 4,6, 8, 10, 12, 14, 16, 18, 20 and 24 hr. All the assessment and appropriate intervention was done by duty resident who was blinded for the drug given in the block. Patients were asked to rate their pain on a scale from 0-10, where 0 represents “no pain” and 10 represents “worst possible pain”. Pain relief was estimated from the total number of rescue analgesic ampoule consumed in first 24 hours after surgery.
Rescue analgesic
All the patients were given rescue analgesia at numeric rating scale score of >3. Injection Diclofenac sodium aqua each ampoule containing 75 mg I.V was used as rescue analgesic. Patients consuming more than 3 analgesics ampoule in the first 24 hours were considered as incorrect placement of drug or failed block and were not included in the study and not considered for statistical analysis. Total number of rescue analgesic ampoule used were calculated for both the group in first 24 hours.
Patient satisfaction
Patients were asked to score their level of satisfaction with the postoperative pain relief up to 24 hours on a four-point scale.
1 = totally dissatisfied
2 = moderately dissatisfied
3 = reasonably satisfied
4 = totally satisfied with pain relief.
Patient satisfaction score was recorded for both the groups at 24 hours postoperatively after surgery and analyzed & compared statistically.
Sample size is calculated at 80% study power and alpha error of 0.05 assuming Standard Deviation of 7.6 hours in duration of analgesia in ropivacaine with dexamethasone group based on previous study.1
For the minimum detectable mean difference in duration of analgesia of 6.1 hours as found in reference study,1 25 patients in each group are required as sample size, which is enhanced and rounded off to 30 patients in each group as final sample size for present study expecting 15% dropouts/ loss to follow up/ attrition.
Unpaired T- tests was used for analysis of normal distribution unpaired numerical variables while categorical variables/nominal variable was analyzed by using Chi- square tests/ Fisher- exact test. Data found to be not normally distributed, numerical variables and unpaired were analyzed using Mann- Whitney U test. P- Value <0.05 was considered as significant. Medcalc 16.4 version software was used for all statistical calculations.
Results
A total of 60 adult consented patients scheduled for lower abdominal surgery were randomized in two equal groups of 30 patients. The ultrasound guidance overall improves the quality of the block and avoid complications as spread of local anesthetic can be visualized in the plane. None of the block failed. No complications and side effects were noted.
The demographic data based on mean age, mean weight, gender and ASA grade were comparable in both the groups and were statistically insignificant. Base line hemodynamic parameters were comparable in both the group and were statistically insignificant.
Table 1
Demographic parameters
Percentage of surgeries are shown in y axis and type of surgeries in x axis of two group.
Mean NRS score is shown in y axis and different time interval in hours along x axis.
Table 2
Comparison of pain score on numeric rating score (NRS) at various time
It is evident from the graph that group B having more pain in NRS score than group A however the difference is only statistically significant at 1hr (P= 0.017), 2hr and 4hr (P < 0.05).
Table 3
Comparison of total analgesic ampoule consumption & durationof first rescue analgesic used
Duration of need of rescue analgesic is comparatively more in group A (12.44±1.60h) vs group B (10.69±1.79h) with significant P value <0.001.
Total analgesic ampoule consumption is comparatively less in group a (1.27±0.64) vs group B (1.63±0.56) with significant P value of 0.024. That is 95.25±48 mg diclofenac sodium in group a vs 122.25±42 mg diclofenac sodium in group B considering 1 ampoule of diclofenac sodium aqua containing 75mg drug.
Discussion
Different concentrations of different local anesthetic agents have been tried since many years in TAP Block but no well-defined dose and concentration of local anesthetic agent has been found yet. Different studies compared different concentrations of local anaesthetic agents with different adjuvants to study the quality of block.
In our randomized study we compared the analgesic efficacy of 0.375% Ropivacaine 19ml and 4mg Dexamethasone that is 1ml total 20ml each side with 0.375% ropivacaine 19ml and normal saline 1ml total 20ml each side in lower abdominal surgeries.
There was no significant difference in the baseline parameter like age, weight, sex, ASA grade, type of surgeries among both the groups. The hemodynamic parameter in term of heart rate, diastolic and systolic blood pressure, respiratory rate, oxygen saturation both pre and post block were similar in both the groups which signifies that the drug combination does not have any significant effect on the hemodynamic parameter of the patients in both groups.
The numeric rating scale (NRS) score when compared in our study between the two groups was found significantly low at 1hr,2hr, 4hr stating additive effect of dexamethasone with ropivacaine in decreasing the pain score significantly compared to ropivacaine with saline group. Till 1 hr NRS score was insignificant possibly due to effect of spinal anesthesia. Mean NRS score was comparatively low in group received ropivacaine with dexamethasone at certain time compared to ropivacaine with saline group throughout 24hrs observation but statistical significance was not found after 6th hr till 24th hr probable explanation may be as rescue analgesic were given in both the groups when NRS score >3 and pain was not allowed to rise in NRS scale in both the groups.
Similar finding was seen by Deshpande JP et al.1 where dexamethasone with ropivacaine in TAP block significantly reduced the VAS score and statistically significant at 4,6,12 hr.
Sachdeva J, Sinha A et al.2 also found similar result in their study where VAS score was significantly lower at 2hr, 4hr, and 12hr.
Pain scores
Numeric Rating Scale (NRS) (0-10) is a tool for pain measurement and is having wide spread use due to its ease of application. It can be substituted for visual analogue scale in acute pain measurement.3 We experienced difficulty in eliciting VAS pain scores in our patients, so we used NRS Scale to assess pain. NRS is simple to use and valuable in assessing response to the intervention.
The primary objective of our study was to compare the postoperative analgesia provided by the block in two groups and we found that 19ml Ropivacaine (0.375%) with 4mg Dexamethasone total 20ml each side in TAP block provided longer duration of analgesia in postoperative period as compared to Ropivacaine (0.375%) with normal saline in term of duration of first rescue analgesic used.
Similar finding was found in study of Gupta A et al.4 where time to first rescue analgesic was significantly more in dexamethasone with ropivacaine 0.375% group compared to ropivacaine 0.375% with normal saline group and their mean duration to first rescue analgesic used in both the group is prolonged than our study. This probably can be due to more volume used in the block as 25ml + 1ml adjuvant each side compared to total 20 ml each side in our study.
M Raghu et al.5 did a similar study with 0.375% ropivacaine with and without dexamethasone and found time of first rescue analgesic used is significantly prolong in dexamethasone group compared to normal saline group, though mean duration of first rescue analgesic used in both the group is less compared to our study.
Sachdeva J et al2 did a similar study with 0.2% ropivacaine 40 ml B/L with and without dexamethasone 8mg in TAP block and found significant prolongation of duration of first rescue analgesic in dexamethasone group but their overall duration of first rescue analgesic in both the group is less compared to our study. This demonstrate that ropivacaine 0.375% provide prolonged duration of analgesia than ropivacaine 0.2% in TAP block.
Similar result was also found in study done by Gnanasekar N et al6 with 0.25% ropivacaine 20 ml with and without dexamethasone stating ropivacaine 0.375% provide prolonged duration of analgesia compared to 0.25% ropivacaine.
Deshpande JP et al1 did a study with 20ml ropivacaine 0.5% with and without 4mg dexamethasone in TAP block B/L side for total abdominal hysterectomy and found significantly prolonged duration of first rescue analgesic used in dexamethasone group compared to normal saline group. Their overall mean duration of first rescue analgesic used is slightly prolonged compared to our study and almost comparable. This demonstrate that ropivacaine 0.375% with 4mg dexamethasone is almost comparable to duration of TAP block with ropivacaine 0.5% with dexamethasone.
Chen Q et al.7 did a meta-analysis and demonstrated mean difference of 2.98hr on duration of analgesia after TAP block with addition of dexamethasone to local anaesthetics which is similar to the finding of our study.
The rescue analgesic used in our study is diclofenac aqua 1ml ampoule containing 75mg of drug and used when NRS pain score >3 in both the group. This is unique and used in comparison to similar studies where predominantly opioids were used in form of either tramadol, fentanyl or morphine2, 5, 6 to avoid postoperative nausea or vomiting related to opioid analgesic.
We found less total analgesic requirement in first 24 hours with addition of dexamethasone 4mg to ropivacaine 0.375% in TAP block. Mean ampoule of diclofenac aqua required as rescue analgesic in dexamethasone and ropivacaine group was 1.27±0.64 which is equivalent to 95.25±48 mg considering 1 ampoule of diclofenac aqua containing 75mg drug. Mean ampoule of diclofenac aqua used in ropivacaine and saline group was 1.63±0.56 which is equivalent to 122.25±42 mg.
Similar findings were seen in the study conducted by Gupta A et al.,4 Deshpande JP et al.,1 Sharma UD et al.,8 Sachdeva et al 2 where tramadol were used as rescue analgesic and found significant reduction in total analgesic used when dexamethasone was added with ropivacaine compared to when ropivacaine used with normal saline in TAP block. Raghu M et al5 used fentanyl as rescue analgesic in their study also found less rescue analgesic used postoperatively with use of dexamethasone and ropivacaine. Gnanasekar N et al6 found reduced use of morphine as rescue analgesic with use of dexamethasone with ropivacaine in their study.
We did not find any adverse event related to TAP block like needle injuries to viscera or intravascular drug deposition.
No adverse drug reaction of ropivacaine 0.375% or dexamethasone when used as additive in TAP block and similar finding was also found in other studies.6, 9, 10
So our study demonstrated that 0.375% Ropivacaine with dexamethasone provided longer duration of analgesia as compared to 0.375% Ropivacaine with normal saline by prolonging need of first rescue analgesic and reducing total analgesic consumption in the postoperative period over first 24 hours.
The study was not without limitations. The analgesic efficacy of TAP block has been demonstrated for up to 48 h in some previous studies, whereas in this study patients were assessed for 24 h. The time to regression of spinal anaesthesia is different in different individuals that could have added to the analgesic efficacy of TAP block in the first few hours postoperatively.
Some potential complications of dexamethasone such as delayed wound healing, hyperglycaemia, and adrenal suppression were not evaluated. However, previous studies have demonstrated that a single small dose of dexamethasone is not associated with significant side effects. Sensory distribution of nerve blockade was not assessed and it may be possible that patients will be able to detect numbness in the abdominal wall. There is some loss of local anesthetic injection in the intramuscular plane due to pressurized injection, which cannot be prevented and may affect the effective volume consumed for TAP Block.
Conclusion
Transversus Abdominis Plane block is an easy and effective method of pain control for lower abdominal surgery in the postoperative period without any significant adverse effects. Our study demonstrated that Injection (Ropivacaine 0.375% + Dexamethasone 4mg) in Transversus abdominis plane block provided longer duration of analgesia as compared to Injection (Ropivacaine 0.375% + Normal saline) after lower abdominal surgeries and is better than 0.2% and 0.25% with almost comparable to 0.5% in term of need for first rescue analgesic. It also decreased postoperative total analgesic consumption in 24 hours.
Transversus Abdominis Plane Block can be used as one of the important multimodal analgesic technique which is effective in providing postoperative analgesia after lower abdominal surgeries with minimal or no side effects and easy to perform, thereby decreasing systemic analgesic consumption in the postoperative period and their potential side effects.