- Visibility 153 Views
- Downloads 19 Downloads
- DOI 10.18231/j.ijca.2020.129
-
CrossMark
- Citation
Post-operative subcutaneous emphysema- are anesthesiologists always at fault
- Author Details:
-
Arunkumaar Srinivasan
-
Kompal Jain
-
Rashi Sarna *
Introduction
Subcutaneous emphysema (SE) following general anesthesia is not a very common encounter in our day to day practice. This rare entity is mostly associated with laparoscopic surgeries with a reported incidence of 0.43% to 2.34%.[1] The etiology of SE includes trauma or surgery involving head and neck, chest, penetrating trauma to the gastrointestinal or respiratory system, iatrogenic (during intubation or laparoscopy, barotrauma, improper chest tube placement) and infectious causes.[2] Hereby, we report a rare case of post operative SE after an emergency laparotomy in an American Society of Anesthesiologists(ASA) physical grade I patient, secondary to uncommon iatrogenic cause.
Case Description
A 30- year- old male, body mass index(BMI) of 20.7kg/m2, ASA grade 1 presented to our emergency with the history of pain abdomen and fever since one day. He had no significant medical and surgical history. The patient was diagnosed as a case of perforation peritonitis. Under all aseptic precautions, abdominal drain of size 32 French (Fr) was inserted to a depth of 18 cm left lumbar area under local anesthesia by the surgical team. Airway examination of the patient revealed mouth opening of 3 fingers, mallampati grade 1 and no neck movement restriction. The preoperative investigations were within normal limits. Preoperative vitals were heart rate – 92/min, blood pressure – 118/70 mm Hg and respiratory rate – 15/min.
The patient was taken up for an emergency exploratory laparotomy under general anesthesia after ASA standard monitoring. Modified rapid sequence induction was done. The patient’s trachea was intubated using endotracheal tube of size 8 mm ID (Internal Diameter) and a Macintosh laryngoscope of size 3 in first attempt. The patient had Cormack Lehane grade 1. The patient was maintained with mixture of oxygen, air and sevoflurane. A vertical midline incision was given. Intraoperative peak pressures were between 14-16 mm Hg. Intraoperative course was uneventful with no episode of desaturation and the patient was reversed using injection neostigmine 2.5mg and injection glycopyrrolate 0.2mg intravenously. His trachea was extubated. Patient was comfortable, conscious and vitals were within normal limits. He was shifted from Post Anesthesia Care Unit (PACU) to general ward.
On postoperative day 2, anesthesia call was received in view of clinical SE due to suspected iatrogenic tracheal injury. The patient did not have any respiratory and abdominal complaints. On general physical examination, he was conscious, hemodynamically stable with a saturation of 95% on room air. The crepitus has extended from abdomen to the anterior chest bilaterally (B/L). His auscultatory findings were normal. Abdominal examination also had no evidence of guarding or induration. His arterial blood gas analysis were within normal limits. Chest x-ray demonstrated B/L subcutaneous emphysema with no evidence of pneumothorax. Pulmonary team was consulted for the same and patient underwent Non Contrast Computed Tomography (NCCT) of the chest and abdomen.
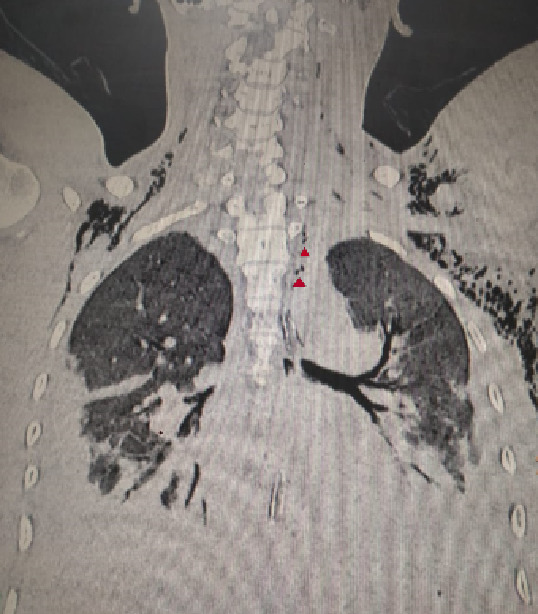
NCCT chest was reported as extensive B/L subcutaneous emphysema extending along the soft tissues of the neck with multiple air foci in the mediastinum with possibility of airway injury. [[Figure 1]] Patient was then planned for bronchoscopy to rule out tracheal injury.
On postoperative day 3, abdominal drain placed in left lumbar area was removed and the patient started improving. Subcutaneous emphysema resolved completely in a step wise fashion in a day. Repeat CT chest [[Figure 2]] demonstrated resolution of subcutaneous emphysema and tracheal injury was ruled out. Since symptoms were resolved, bronchoscopy was withheld by the pulmonary team. He was discharged home on postoperative day 6. He was followed up for further six months and the patient had no complaints.

Discussion
From the literature, three categories of SE have been described. First by gas producing infection, secondly due to perforated viscus and third due to gas introduced from outside. It includes postsurgical procedure with trauma being the most common cause.[3] Different anesthesia related causes of subcutaneous emphysema includes positive pressure ventilation, traumatic laryngoscopy/intubation causing esophageal/hypopharyngeal perforation, an inappropriately closed pop off valve, faulty anesthesia circuits causing high airway pressures and coughing after closed airway.[4]
In our case, abdominal examination and CT ruled out an abdominal pathology or perforated viscus. Investigations and Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score[5] of less than 5 ruled out any evidence of infection, suggesting the third category of SE i.e gas introduced from outside. Whilst endotracheal intubation is the most frequently encountered cause of iatrogenic tracheal injury, with a reported incidence of 0.005%.[6] Over-inflation of cuff and sudden movement of tube were the most reported causes for tracheal injury. Direct tear caused by the tube was rare.[7], [8], [9] Intraoperatively, he had normal peak pressures with no episode of desaturation and difficulty in ventilation excluding pneumothorax and above mentioned anesthesia causes. He had smooth induction and extubation excluding SE due to coughing against closed airway.
Hence, the ‘apparent’ tracheal injury and the subcutanaeous emphysema were secondary to faulty placement of the abdominal drain in lumbar area which could have probably caused introduction of free air extending into the subcutaneous plane along the retroperitoneal surface and might have clouded the clinical picture. Resolution of SE after drain removal confirmed our diagnosis.
To conclude, it is imperative to perform a differential diagnostic process. Diagnosis can also be recognised by exclusion which can prevent further unnecessary interventions. Our case also describes the differential diagnostic process of postoperative SE including anesthetic and surgical causes.
Conflict of Interest
The author(s) declare(s) that there is no conflict of interest.
References
- D E Ott. Subcutaneous Emphysema—Beyond the Pneumoperitoneum. J Soc Laparoendosc Surg 2014. [Google Scholar] [Crossref]
- N Patel, S K Lazow, J Berger. Cervicofacial Subcutaneous Emphysema: Case Report and Review of Literature. J Oral Maxillofac Surg 2010. [Google Scholar] [Crossref]
- A Macera, L Sirleo, R S Serrrano, M Innocenti, F J C Suarez, C S Rueda. Cutaneous Crepitus is not equal to Gangrene. The Exceptional case of Benign Subcutaneous Emphysema. Acta Sci Orthop 2018. [Google Scholar]
- P H Pan. Perioperative subcutaneous emphysema: Review of differential diagnosis, complications, management, and anesthetic implications. J Clin Anesth 1989. [Google Scholar] [Crossref]
- C H Wong, L W Khin, K S Heng, K C Tan, C O Low. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004. [Google Scholar]
- P Borasio, F Ardissone, G Chiampo. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardio-Thorac Surg 1997. [Google Scholar] [Crossref]
- A Boulemden, P Aifesehi, A Pajaniappane, K Lau, A Bajaj, A Nakas. Subcutaneous drain insertion in patients with post-operative extensive subcutaneous surgical emphysema: a single centre experience. Gen Thorac Cardiovasc Surg 2013. [Google Scholar] [Crossref]
- V Sivarajah, C Jones, A Pittathankal. Radiological evidence of subcutaneous emphysema leading to a diagnosis of retroperitoneal perforated diverticulum. Int J Surg Case Rep 2013. [Google Scholar] [Crossref]
- H Ota, S Fujita, T Nakamura, S Tanaka, T Tono, Y Murata. Pneumoretroperitoneum, Pneumomediastinum, Pneumopericardium, and Subcutaneous Emphysema Complicating Sigmoidoscopy: Report of a Case. Surg Today 2003. [Google Scholar] [Crossref]
