Introduction
Pain during positioning in patients with fracture femur, results in improper position for sub arachnoid block (SAB) and making SAB difficult even in patients with normal spine. Providing adequate pain relief not only increases comfort in these patients, but has also been shown to improve positioning for SAB. Drugs like opioids, midazolam, ketamine or peripheral nerve block like FNB (Femoral nerve block), 3-in-one block, fascia iliaca block have been used to provide analgesia. Peripheral nerve blocks are popular for providing pain relief following fracture and surgery.1, 2, 3, 4, 5, 6 But there are very few studies where peripheral nerve blocks has been given for pain relief to improve the positioning. Among the peripheral nerve block, FNB is easy to perform because landmarks are easy and nerve is usually superficial.7
Fentanyl is a more potent with rapid onset and short duration of action with less respiratory depression, nausea and vomiting. We compared the analgesia provided by FNB and intravenous fentanyl prior to positioning for SAB in patients undergoing surgery for femur fracture. The primary aim was to compare the analgesic effect provided by FNB and intravenous fentanyl and secondary aims were to see sedation score, hemodynamic changes and complications, if any.
Materials and Methods
This open labelled prospective, clinical study was carried out after taking permission from the Institutional ethics committee for human research and written informed consent of patients. We included 60 patients aged 18-70 years of either sex, of ASAPS/ EASAPS – I, II, III, posted for fracture femur surgery under SAB and likely to have pain while positioning and patient able to understand visual analogue scale (VAS) score for assessment of pain. A thorough pre-operative assessment was carried out which included history, examination, and investigations (complete hemogram, renal functions, blood sugar levels, chest X-ray, and electrocardiogram). Patients with contraindications to SAB, allergy to amide local anaesthetics or fentanyl, history of alcohol abuse, morbid obesity with multiple fractures, patients’ refusal and unable to understand VAS score or use of analgesics 8 hours before the performance of SAB were excluded from the study. All the patients were kept nil by mouth for at least 6 hours. Inside the operation theatre, multipara monitor was attached and baseline vital parameters were noted. An intravenous line was secured with 18 G cannula and preloading started with injection ringer lactate 10ml/kg intravenously over a period of 20 minutes. All the patients received injection glycopyrrolate 0.2mg intravenously and injection ondansetron 4mg intravenously before the procedure. Patients were assigned into two groups alternately in - group FNB and group FENT. In group FNB, patients received the FNB guided by a peripheral nerve locator 10 min prior to positioning. Entry point was infiltrated with 1 ml of 1% lignocaine and then a 50 mm 22gauge insulated needle (Stimuplex, B Brawn) was introduced 1 cm lateral to the femoral artery and 1.5 cm below the inguinal ligament. When a stimulating current of 0.3–0.5 mA elicited a quadriceps contraction, 20 ml of 1.5% lignocaine with adrenaline (1:200000) was injected (15 ml 2% lignocaine plus 5 ml distilled water) incrementally after a negative aspiration. All the blocks were given by the same experienced person. In group FENT, intravenous fentanyl 1µg/kg was given for positioning before SAB. If any patient in either group reported pain scores ≥4 during positioning, injection fentanyl 0.5 μg/kg intravenously was to be given every 5 min until the pain score decreased to <4 or maximum dose of 2 μg/kg was given (whichever first). If pain score of <4 could not be achieved, then patient was to be excluded from the study.
Thereafter, a SAB was performed in lateral position in either the midline or paramedian approach at the L2/3 or L3/4 level, with 2-4ml of hyperbaric bupivacaine according to the anesthesiologist’s decision. Pain assessment for positioning the patient for SAB was done using VAS score, time taken to achieve position, quality of position, patient acceptance and additional doses of fentanyl requirement during positioning. Patients were also observed for sedation score, pulse rate, systolic blood pressure(SBP), diastolic blood pressure(DBP), oxygen saturation (SpO2), respiratory rate before analgesia, 10 min after analgesia, during position and following SAB throughout the surgery (at 1, 3, 5, 10, 15, 30, 45, 60, 75 and 90 minutes) and complications, if any. VAS score was assessed before analgesia, 10min after analgesia and during positioning. VAS score before analgesia was assessed by asking whether patient had pain while shifting the patient to operation theatre or changing position from supine to sitting or vice a versa. Time taken to achieve position was defined as time taken from the beginning of lateral positioning to end of SAB in seconds. Quality of patient positioning for SAB was recorded by a performer with scores 1-3.(Appendix-1).8
Appendix-1 Quality of patient positioning
Score 1 - satisfactory, able to give position with difficulty.
Patient acceptance was noted as yes or no. (by patient himself/ herself). Patients were also observed for complications or side effects like respiratory depression (RR<10/minute or SpO2 <92%. It was treated with 100% Oxygen.), nausea, vomiting, muscle rigidity, hematoma, pruritus, bradycardia (pulse rate less than 60/minute or 20% decrease in pulse rate of pre-procedure value). It was to be treated with injection atropine 0.6 mg iv. Hypotension (systolic blood pressure less than 80mm Hg or fall in SBP of 20% of pre-procedure value was considered as hypotension and was to be treated with oxygen, intravenous fluids and ephedrine 5mg).
Sample size estimation was performed using software “MedCalc” for Windows, version12.5 (MedCalc Software, Ostend, Belgium), using the parameter “quality of position” from the reference study.9 Quality of position in group FNB was 2.66±0.606 and in group FENT was 1.96±0.85. Taking alpha error as 0.05 and beta error as 0.1, the calculated minimum sample size came to 24 in each group. We studied 30 patients in each group. Observed data were entered into Microsoft Excel 2010 and statistical analyses were performed using MedCalc for Windows, version 12.7.5.0 (MedCalc Software, Ostend, Belgium). Qualitative data were analyzed using “Chi-square test” and quantitative data were analyzed using paired and unpaired t-test. A ‘p’ value of <0.05 was considered statistically significant.
Results
The two groups in our study were comparable to each other with respect to age, weight, sex and ASAPS (P>0.05) (Table 1).
Table 1
Demographic data
From Figure 1 VAS score before giving analgesia in both the groups were comparable. (P= 0.84). VAS score 10 minutes after giving analgesia and during positioning was less i.e.1.97±0.56 in group FNB and 2.87±0.35 in group FENT, which was statistically very highly significant (P < 0.0001).
Table 2 gives the assessment of effective positioning for SAB in group FNB and group FENT by assessing time taken to perform SAB, quality of positioning and patient satisfaction. Here, it is to mention that none of the patient in either group required additional dose of fentanyl.
Table 2
Comparison of effective positioning for SAB
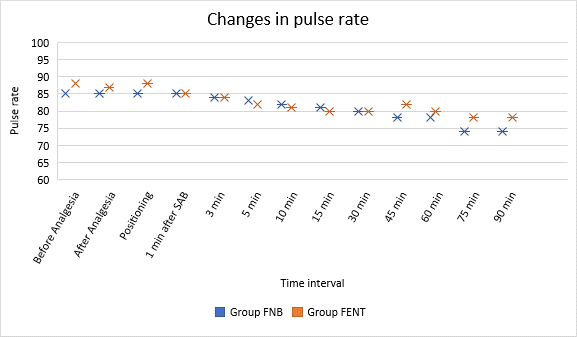
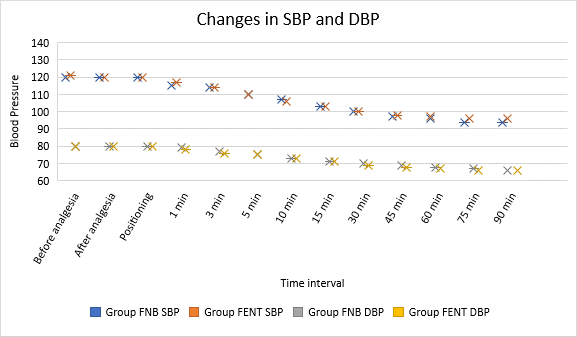
In group FENT 16 (53.33%) patients had sedation score 0 i.e. awake and alert throughout the study and rest all had sedation score 1, i.e.14 (46.67%) drowsy, but responds to verbal stimulus, while in group FNB all 30 patients (100%) had sedation score 0. SpO2 and respiratory rate remained normal during study period and thereafter. In group FNB and FENT, there was no change in mean pulse rate, systolic blood pressure and diastolic blood pressure during the study period (p>0.05) but there was a gradual decrease 3 minutes after giving subarachnoid block and remained lower thereafter which was statistically significant(p<0.05).
In group FNB 13.33% of patients and in group FENT 10% of patients showed bradycardia in our study. Both the groups showed hypotension in 16.67% patients. None of the patients showed any complications like nausea/vomiting, pruritus, muscle rigidity, hematoma, block failure in either of the group.
Discussion
From our study, we could say that FNB offered superior analgesia compared to intravenous fentanyl during position for SAB. Of all the deep somatic structures, pain threshold of periosteum is lowest. As a result, most of the patients with femoral fractures are in considerable pain, therefore, they should be given adequate pain management before positioning, and transferring.10 Pain during positioning for SAB results in increased number of attempts, longer duration of painful position and rarely failure to achieve SAB even in patients with normal spine. Thus, correct positioning during SAB becomes the necessity.
Various peripheral nerve blocks like FNB, 3 in one block and fascia iliaca block are being given for analgesia for femur fracture.2, 3, 4, 6, 11, 12, 13, 14, 15, 16, 17, 18 Three in one block and fascia iliaca block produces superior analgesia compared to simple FNB.11, 12, 13, 16, 18 But it takes longer time for the onset of sensory effect and dose of drug required to produce adequate analgesia is more for 3 in one block or fascia iliaca block.4, 6, 7, 13, 19 So there might be chances of exceeding the dose of local anaesthetics as it was to be followed by SAB. There are some studies where FNB had been used to provide analgesia for positioning before giving SAB.7, 8, 9, 14, 20, 21, 22, 23 We selected FNB because it is one of the easiest peripheral nerve block to perform, it’s landmarks are easy as nerve is superficial and provides adequate analgesia even with lesser dose of local anaesthetics.7 The use of a long-acting local anaesthetic instead of lignocaine might have allowed more effective postoperative pain relief, but they may prolong the onset of action. Other studies reported that a five-minute interval was adequate to establish the analgesic effect produced by FNB using 1.5% lignocaine.9 But we waited for 10 minutes to maximize the analgesic effect of fentanyl and FNB. And we thought that a time interval longer than ten minutes could have excessively prolonged the time for anaesthetic procedure. Iamaroon A et al. used bupivacaine for FNB and waited for only 15 minutes due to pressure of surgeons. He confessed that to maximize the analgesic effect of bupivacaine, a time interval longer than 15 minutes would have been chosen.14
In our study, fentanyl 1µg/kg was chosen to obtain potent, short-lasting analgesia with minimal side effects 10 minutes before positioning for SAB. Jadon A et al. also used same dose of fentanyl for positioning for SAB with 100% success rate without any complications.9 Iamaroon A et al. used two doses of intravenous fentanyl 0.5µg/kg with a five-minute interval between doses and lateral position was given for SAB 15 minutes following drug administration. They explained titration of dose of fentanyl may reduce serious side effects like hypoventilation or apnoea especially in elderly.15 Sia S. et al. used a dose of fentanyl 3µg/kg IV and gave position after 5 minutes. They noted fall in oxygen saturation in fentanyl group in their study.8 However, we did not come across such side effects in our study. For giving SAB either lateral or sitting position has been used. Both have been successfully used in various studies. In lateral position there is more chance for overriding of fracture segments but it requires minimum flexion, thereby could have improved patients comfort.8 And also since we were to give intravenous fentanyl which is a sedative and can cause orthostatic hypotension especially in elderly patients, it is better to position the patients in lateral rather than sitting.23 Other authors used sitting position for performing SAB in their studies as they might have thought of it as an easier way to leave traction in place during the procedure.7, 8 While Iamaroon A et al., Yun M J et al. used lateral positioning for spinal anesthesia.14, 17
Various authors reported significantly low pain scores with FNB compare to IV fentanyl.7, 8, 9, 13, 22, 24 Iamaroon et al. did not find any significant difference between FNB and intravenous fentanyl. The probable reason for decreased efficacy of FNB in their study was use of 0.3% bupivacaine and waiting period of only 15 min to position the patient.14 Time taken to achieve SAB was also found to be high in patients who had taken intravenous fentanyl compared to patients who were given FNB which was statistically very highly significant (P<0.0001). Sia S et al. noted a performance time for SAB as 1.8±0.7 min in group FNB and 3.0±1.1min in group FENT.8 Jadon A et al. noted time for anaesthesia as 15.33±1.64 in group FNB and 19.56±3.09 in group FENT (P<0.000049). 10 In patients who received FNB quality of position was excellent in 28 patients and good in 2 patients. But in those who received intravenous fentanyl quality of positioning was excellent in 19 patients and good in 11 patients, (P=0.01). Regarding patient acceptance all the 60 patients in our study said yes with the pain relief method and there was no statistically significant difference in both groups (P>0.05). The 100% acceptance may be because all the fractured femur patients were in great agony before giving analgesia. In various studies the time to perform SAB was shorter in group FNB, with better quality of positioning and patient acceptance compared to IV fentanyl.7, 8, 9, 15, 21, 25 Iamaroon A et al. found out that patient satisfaction was equal in both the groups.14 The good analgesic effect and the paralysis of the quadriceps allowed better patient positioning and a shorter spinal anaesthesia performance time in FNB group.8 None of the patients in either group required additional analgesia during position in our study. Jadon A et al. also suggested that there was no need for additional analgesia in both the groups.9 Salvatore S et al. had given supplemental fentanyl to one patient in fentanyl group even though they used high dose intravenous fentanyl for analgesia(3µ/kg).8 Iamaroon A et al. had given supplemental analgesia to patients in both the group.14 They used incremental dose of fentanyl, two doses of 0.5µg/kg IV at 5 minutes interval, in order to avoid complications like sedation and respiratory depression. But it resulted in increased rate of additional fentanyl requirement in fentanyl group.
The mean pulse rate, SBP, DBP, respiratory rate and oxygen saturation were comparable in both the groups. Bradycardia was observed in 13.33% of patients who received FNB and 10% of patients who received intravenous fentanyl in our study. Hypotension was observed in 16.67% patients from both the groups. Both bradycardia and hypotension we observed were within the clinically normal limits and did not require any treatment.
There are few limitations in our study i.e. In our study all the research participants were aware of their treatment group allocation since it was an open label study and we were comparing analgesic effect of peripheral nerve blockade with an intravenous drug. We considered placebo injection in inguinal area was unjustified.
Use of USG guided block would have given better results with lesser dose of local anaesthetic.
Conclusion
FNB and intravenous fentanyl both provided adequate analgesia, hence satisfactory positioning for SAB with patient acceptance, stable hemodynamics without need for additional analgesia and complications. However, FNB provides better analgesia in terms of lower VAS, excellent positioning and less time for the performance of SAB than intravenous fentanyl. So, we can consider that FNB is comparatively more advantageous than intravenous administration of fentanyl to facilitate the lateral position for SAB in patients undergoing surgery for femur fracture.