Introduction
Monitored anesthesia care is a specific service used for diagnostic or therapeutic procedure providing sedation and analgesia while preserving spontaneous breathing with intact airway reflexes. Presently MAC is the first choice in 10-30% of all surgical procedures.1 The main purpose of MAC is to provide patient a good pain free procedure, sleep like sedation and satisfaction at the end of surgery. Communication between patient and anaesthesiologist care team serves a tool for monitoring sedation levels and to offer verbal assurance; it can also improve patient co-operation. Patient co-operation is essential during MAC2 and therefore MAC may not be so suitable for very apprehensive patients for whom other anesthetic technique would be a better alternative which can be found out during preoperative visits. MAC should also be preferred in patient with cardiovascular, respiratory, renal and hepatic instability as a good alternative to GA. Intraoperative monitoring during MAC should be effective, non-invasive and economical.3 It should give us continuous monitoring of patient circulation, ventilation, oxygenation. Capnography accurately detects apnea during MAC procedures,4 serves as a specific tool to detect hypoxemia more quickly than SpO2 probe. An ideal sedative agent should have rapid onset easy titration, high clearance with lack of major cardiovascular and respiratory depression.5 Also it should have quick context sensitive half life so patient awakens quickly soon after the infusion stops. Ideally a sedative drug should have good amnesia, analgesia, anxiolysis and rapid recovery. Propofol and benzodiazepines have long been used as drugs for MAC but these drugs have a serious drawback that is respiratory depression.6 Ketamine is a effective agent for procedural sedation with no serious adverse effects but there is a significant incidence of recovery agitation requiring treatment with a benzodiazepine.7 Midazolam and fentanyl combination significantly increases the risk of hypoxemia and apnea in patients.8 Review of MAC cases in the ASA closed claims database confirms that significant morbidity and mortality can occur of respiratory depression because of sedative drugs miscalculated relatively or overdose. Respiratory compromise was associated with large claims and 41% of those claims were related to death or permanent damage.9 The side effects of various drugs were overcome by introduction of a novel α2 agonist called dexmedetomidine. It has been used as a sole anesthestic agent in patient with compromised respiratory state.
A good surgical field is achieved if no or minimal bleeding and a good sympatholytic state is achieved. Also if the patient has less anxiety then the patient experiences less pain thus an anxious patient requires more anesthetic agent to attain a better hemodynamic and stable anesthesia. Dexmedetomidine is novel sedative agent used for MAC in wide range procedures including fiberoptic bronchoscopy, dental procedures, plastic surgery, ENT, ophthalmic surgeries, neurosurgery, vascular surgeries. It reduces opioid requirement and stress response to surgery ensuring a stable state.10 So going through various literatures there are no dictum on any fixed maintenance dose of dexmedetomidine and has been widely used at range of 0.2 – 0.7 µg/kg/hr titrated to achieve target levels. Main aim of our study was to conclude a optimally safe maintenance dose with stable hemodynamics, adequate sedation and minimal side effects.
Materials and Methods
This prospective, comparative, randomized, double blinded study was held after institute ethical committee approval. 70 patients ASA I –III aged 18-65 years of either sex for surgeries under local anesthesia with written informed consent from all participants. Patients excluded from the study are those allergic to local anesthesia, severe uncontrolled hypertension and hypotension, heart blocks, recent angina /MI and pregnant patients. Randomization was done using computer generated random number and patient divided into two groups on the basis of number allotted to them. The drug solution for infusion was prepared by another anesthesiologist and the volume was kept constant at 50 ml in infusion pump in both groups. The investigator conducting the case, the patients were all blinded to the group assignment. Data was collected by a blinded observer who was also unaware of the group division. The drug infusion to be infused during the study was prepared by adding 49 ml of NS with 1 ml (100 mcg) of dexmedetomidine hydrochloride and infusion was given through a infusion pump according to patient weight with a loading dose of drug followed by a maintenance dose by the same infusion pump till the end of surgery. 70 patients received a loading dose of dexmedetomidine 1 mcg/kg over 10 minutes followed by group A receiving maintenance dose of 0.2 mcg/kg/hr and group B receiving maintenance dose of 0.4 mcg/kg/hr. All patient received LA infiltration at incision site with injection xylocaine 2% with adrenaline (1: 200,000) at dose not exceeding 7 mg/kg before surgery following 10 minutes of loading dose of dexmedetomidine.
A through pre anesthetic checkup and assessment was done in each patient and recorded in PAC chart. All routine investigations according to hospital protocol were done day before surgery and evaluated. All the patient were counselled about the LA infiltration, Ramsay sedation score and scoring scale before surgery. Patients were explained about the grading of pain with 0= no pain and 10 =worst pain for NRS. An Numerical Rating Scale is more practical than visual analogue score, easier to understand for most people. Surgery expected to last more than 30 minutes including plastic surgery, vascular surgery and ENT surgery done under MAC were included.
On arrival into operation theatre, after confirming adequate fasting, patient vitals (HR, BP, SpO2, RR, RSS) was noted after all monitors being attached. An adequate sized cannula secured and NS was started at 2 ml/kg/hr. No premedication sedative was given. Both group received study drug along local infiltration. Surgery was commenced once adequate analgesia achieved. If inadequate analgesia was noted LA infiltration by surgeon along with injection Fentanyl rescue dose of 1 mcg/kg given which was repeated if required not exceeding 3 doses. If target sedation of 3 by Ramsay sedtion score was not achieved then injection Midazolam 0.01 mg/kg was given and repeated till adequate sedation was achieved with dose not exceeding thrice. The protocol specified to use maximum three rescue doses during the study of each patient. At any point of time if clinically indicated or rescue drug reached its limit, the anesthetic technique changed and study discontinued.
The patient was observed for any other adverse effects during the study period and was treated accordingly– Bradycardia defined by HR < 50/min with hemodynamic instability was treated with Atropine 0.01 mg/kg. Hypotension defined by drop in MAP of 20% from baseline was treated with intravenous bolus of fluids and mephentermine 0.1 mg/kg intermittent bolus dose. Tachycardia treated with titration bolus dose of metoprolol 0.1 mg/kg. Hypertension with >20% MAP from baseline in treated with intermittent titrated bolus dose of labetalol. If bradyapnea <10/min or desaturation of <90% was treated with supplementary oxygen patient was awakened and ask to take deep breaths. Any episode of vomiting was treated with injection ondansetron 0.1mg/kg. Study drug infusion was stopped once the surgery ended with skin closure and assessing all vitals and RSS. Patient was then shifted to PACU and monitored for any adverse effect and treated accordingly. Patient discharged from PACU when Modified alderete score >9 and surgeon was asked to grade their overall satisfaction. Patient was asked to grade their overall satisfaction by Likert scale on post -operative day 1 of surgery or before discharge from hospital.
Statistical analysis were compared between both group A and B for age, sex, ASA grade, type of surgery, side effects, rescue drugs, sedation score, surgeon and patient satisfaction along with all hemodynamics and vital signs (SpO2, PR, RR). Chi square and Fischer exact were used for categorical/nominal variables and presented in percentages. Unpaired ‘T’ test used for liner variables and will be summarized as Mean, SD and Median. While Mann Whiteney and for ordinal variables expressed as median, mean and SD. P<0.05 was taken statistically significant and med calculator 16.4 version was used for statistical calculations.
Results
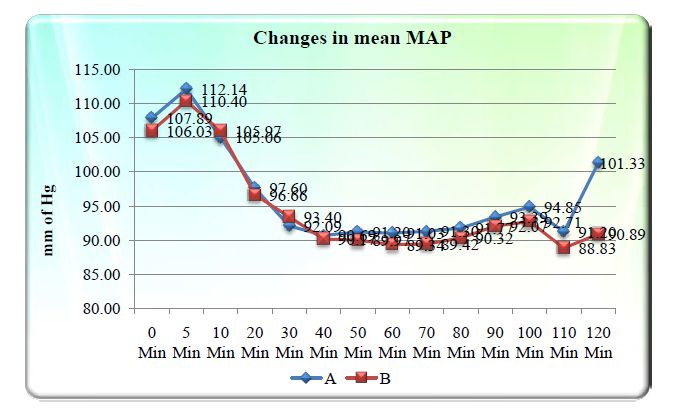
The results showed comparable values between both groups A and B in terms of age group, gender, type of surgery ASA distribution with no significant p values seen. The Mean Arterial Pressure was comparable between both groups A and B with no statistical significance.
Mean Heart Rate was 83 ±12.71 in group A & 81.80 ±11.68 in group B with ‘p’ value of 0.508 at 0 min. Mean HR at 30 minutes in group A was 73.74 ±11.27 and group B was 72.97 ±11.45 &’ p’ value of 0.778. The minimum HR was 48 in both groups at 40 min. Mean HR in group A at 60 min was 69.27 ±11.07 & in group B 66.69± 9.87. There was no statistical significance seen in HR between both study groups A & B.
The mean RR in group A at 0 Min was 18.31 ±1.39 & group B was 18.60±2.14 with the ‘p’ value of 0.504. The mean RR in group A at 30 min was 14.86±1.73 & group B was 15.46 ±2.24 with the ‘p’ value of 0.214. The minimum RR was 11 in group A & B at 80 minutes. There was no episode of bradyapnea seen in any patient in both groups. There was no statistical significance found between group A & B. There changes for SPO2 was comparable between both groups with lowest SPO2 was 88 in 60 min in group B.
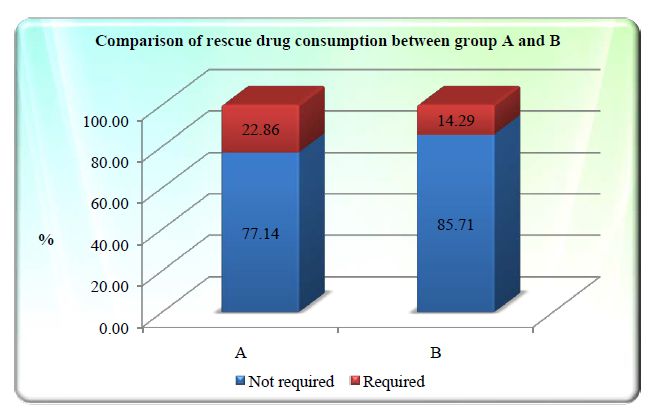
Rescue drug consumption was required in 8 patients (22.86%) out of 35 in group A & 5 patients (14.29%) out of 35 patients in group B. ‘p’ value was 0.54 by Fischer exact test & it is statistically insignificant.
Mean NRS for pain at 30 min in group A was 0.17± 0.75 and group B was 0.20 ±0.68 and ‘p’ value of 0.850. No statistical significance was found between group A and B for pain scoring.
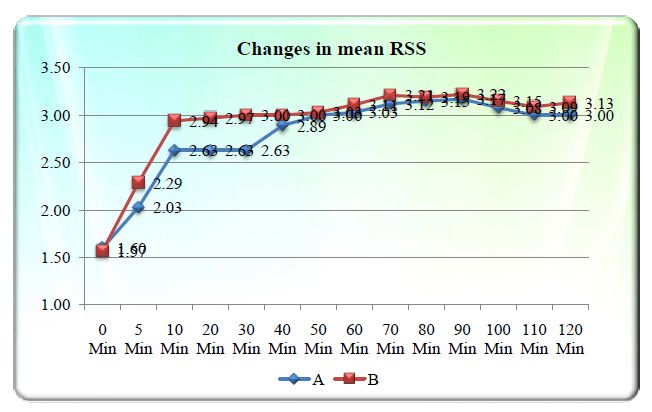
Mean sedation in group A at 0 min was 1.60±0.50 and in group B was 1.57±0.50. Mean sedation at 20 min in group A was 2.63±0.49 and in group B is 2.97±0.17 and p value of 0.014 which was statistically significant. Mean sedation at 30 min in group A was 2.63±0.49 and in group B was 3.0 ±0.00 and p value of 0.007 which was statistically significant. Thus ‘p’ value was statistically significant in 10, 20 and 30 minutes. Target sedation of RSS 3 at 30 min was achieved in 22 patients (62.86%) out of 35 in group A and in 35 patient (100%) in group B. The p value is 0.001 and was highly statistically significant.
Surgeon was very satisfied in 5 patients (14.29%) in group A and 27 patient (77.14%) in group B and satisfied in 23 patients (65.71%) in group A and 4 patients (11.43%) in group B. Surgeon was dissatisfied in 7 patients (20%) in group A and 2 patients (5.71%) in group B. The ‘p’ value was 0.001 and is statistically significant.
Patient satisfaction was comparable between both group A and B. 15 Patients (42.86%) were very satisfied in both group A and B. 10 patients (28.57%) were satisfied in group A and 15 patients (42.86%) in group B. No patients were dissatisfied in any of the study groups. The p value was of 0.264 with no statistical significance found.
Table 1
Surgeon satisfaction between Group A and Group B
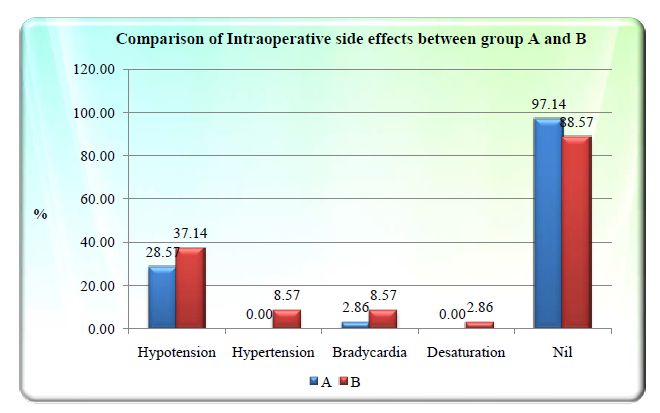
Bradycardia was noted in 1(2.86%) patient in group A and 3(8.57%) patient in group B. Hypotension noted in 10(28.57%) in group A and 13(37.14%) pt in group B. There was no significant p value found between group A and B for intraoperative side effects.
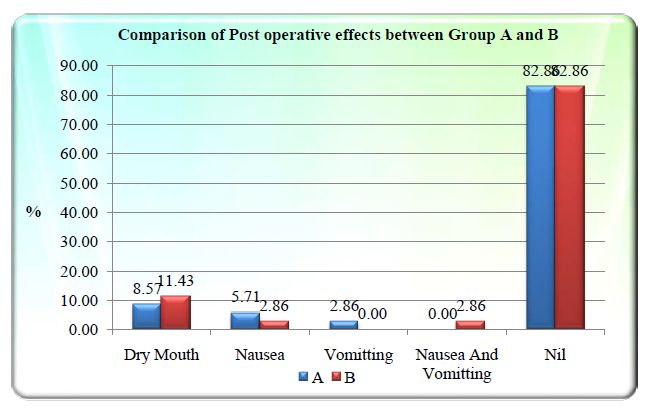
Dry mouth, nausea and vomiting was noted in postoperative side effects. There was no statistical significant p value found between two groups A and B for postoperative side effects.
Discussion
Dexmedetomidine has been safely and effectively used in various surgery under MAC. Dexmedetomidine has replaced many sedative drugs in MAC, GA and regional anesthesia since its advent due to its unique property of rapid arousability, minimal or no respiratory depression. An additional property of dexmedetomidine that have popularized the drug in recent times in ENT, vascular, plastic surgery, neurosurgery is providing good bloodless surgical field adding to surgeon’s satisfaction levels.
In hemodynamic changes in our study
There was a transient increase in Mean arterial pressure from baseline values after loading dose at 5 minutes in both the groups and then started to decrease continuously and maximum lowest MAP seen at 60 minutes of infusion. Thus there was a transient increase of MAP was followed by decrease in MAP after 10 minutes of infusion. The MAP between group A and B was comparable during the whole study time between both groups. Hall JE et al.11 studied the response of bolus loading 6 mcg/kg/hr followed by 0.2 and 0.6 mcg/kg/hr which showed a biphasic response with a transient increase in BP within one min of bolus followed by maximum decrease in MAP significantly at 60 min. This increase in BP was attributed to direct effects of α2-adrenoceptor stimulation of vascular smooth muscles. The decrease in BP caused by inhibition of sympathetic outflow that overrode directs effects of dexmedetomidine. Thus similar trend of MAP rise and fall was seen in our study.
The mean heart rate showed a decreasing trend from baseline with maximum decrease in HR at 60 and 90 minutes. The lowest HR was 47 in group A and 48 in group B at 60 min which did not require any active rescue drug therapy. Kawaai H et al.12 studied the comparison of dose 0.2 µg/kg/hr vs 0.4 µg/kg/hr of dexmedetomidine following loading dose of 6 µg/kg/hr. There was significant decrease of HR from baseline and this bradycardia effect is postulated to be a baroreceptor mediated reflex event secondary to MAP increase caused by activation of α2B receptors on peripheral vasculature. There is no significant cardiovascular variations seen between both the study group. Saad A et al.13 in his study starting a loading dose of 0.5-1 mcg/kg over 10 mins followed by maintenance 0.2-0.4 mcg/kg/hr titrated to effect. Out of 41 cases 11 cases had low BP with low heart rates requiring to discontinue and stop infusion with pressor medications. No patient in our study group had such serious hemodynamic instability as seen in the above study. The lower HR and MAP in our study may have contributed to better bloodless surgical field contributing to overall surgical conditions.
The α2 agonist have some significant analgesic effects however the analgesic effect of α2 agonist does not approximate the potency of opioids.14 The primary action of pain relief was thought to be substantia gelatinosa of spinal cord at α2C receptors where dexmedetomidine reduces the release of nociceptive neurotransmitters substance P. In our study rescue drug was used in 22.86% in group A and 14.29% in group B. Fentanyl rescue (single) dose was consumed in 2 patient in each group A and B while double dose was used in 1 patient in group A and 3 patient in group B. Midazolam was used in group A as single dose in 4 patients and double dose in 1 patient while no midazolam was consumed by any patients in group B, thus group A and B in terms of midazolam rescue use were not comparable. Padmaja A et al.15 comparing dexmedetomidine maintenance of 0.5 mcg/kg/hr after a loading of 1 mcg/kg/hr against midazolam 0.06 mg/kg concluded that lesser rescue analgesics were required in dexmedetomidine group along with higher sedation score. Hall JE et al.11 observed 20-30% reduction in pain by VAS scores among subjects receiving dexmedetomidine infusions.
Continuous quality improvement is of increasing interest to anesthetist. Patient satisfaction is an important measure of quality of healthcare and use as an outcome measures in interventional and quality improvement studies.16 While surgeon are coworkers and important clients of anesthesiologists, the level of satisfaction should be explored to optimize quality.17 No patients in both groups were dissatisfied with our hospital care while same no of patients of patients in both groups A and B were very satisfied. But there was no statistically significance between both groups for patient satisfaction. Our study showed that surgeon were very satisfied in group B (0.4) compared to group A. The p value was <0.001 and was statistically significant for surgeon satisfaction. The higher surgeon satisfaction might be due to higher sedation causing less movement during surgery leading to less sympathetic activation. Parikh DA et al.18 studied the comparison of dexmedetomidine and Midazolam -Fentanyl group under MAC for Tympanoplasty and found that better surgery and patient satisfaction in dexmedetomidine group than Midazolam and Fentanyl group. Candiotti KA et al.19 in the prospective randomized double blinded multicenter trial with dexmedetomidine found both patients and anesthesiologist satisfaction and comfort better with dexmedetomidine than placebo group. Durmus M et al.20 in his study concluded that dexmedetomidine decreases bleeding, postoperative analgesic requirement, intraoperative requirement with stable hemodynamics response to anesthesia.
Our study intra operative side effects were noted of which hypotension was most common followed by hypertension, bradycardia and one episode of desaturation. All these patients with dexmedetomidine side effects during intraoperative period did not required any immediate emergency rescue therapy and subsided without any aggressive intervention. While in postoperative side effects in our study, dry mouth was the most common side effects followed by nausea and vomiting. There was no statistical significance p value for postoperative side effects between study groups. Bhana KNL et al.21 in his study concluded that hypotension as the most common side effects followed by hypertension, nausea, bradycardia, dry mouth along with other side effects.
Kawaai H et al.12 in his study found no significant changes in RR, MV, ETCO2 with baseline in each group 0.2 and 0.4 mcg/kg/hr. Our study showed no effects of drug on RR with no episode of bradyapnea.
The sedation of Dexmedetomidine has a unique ‘cooperative’ conscious sedation resembling natural sleep. This is mediated by α2 Receptor on locus cereleus of pons in a dose-dependent inhibition of NE release. This unique sedation is complex circuitry sleep which is different from GABA-nergic sedatives.5, 9 This sedative preserves muscle tone with spontaneous respiration and awakening patients on simple commands. Kawaai H et al.12 in his study comparing 0.2µg/kg/hr and 0.4 µg/kg/hr showed that sedation level in 0.4 group reached optimal level earlier than in 0.2 group however sedation level in 0.4 group tended to be higher than 0.2 at 25 and 30 minutes of dexmedetomidine infusion. Sedation in 0.2 group did not reached optimal score at 10 min after dexmedetomidine infusion. In our group B had higher and quicker target sedation compared to group A which is similar to finding in the earlier study mentioned.
OK HG et al.22 studied the comparison of 0.2 and 0.4 µg/kg/hr after a loading dose of l ug/kg over 10 min in spinal anaesthesia, concluded that higher dexmedetomidine maintenance of 0.4 ug/kg/hr resulted in longer and adequate sedation. Sim JH et al.23 in his study concluded that higher loading dose of l mcg/kg/hr over 10 minutes followed by 0.5 mcg/kg/hr lead to faster sedation without any complication. Our study too showed faster achievable sedation with higher maintenance group.
Conclusion
Dexmedetomidine maintenance infusion of 0.4 µg/kg/hr is equally safe as 0.2 µg/kg/hr and has an additional advantage of quicker achievable target sedation and better surgeon satisfaction for surgery, hence can be safely used for maintenance of sedation under MAC. Hypotensive effects of dexmedetomidine on CVS may be beneficial in high risk patients and also causes decreased bleeding thus providing a bloodless surgical field which adds to the overall comfortnes of the surgeon.