- Visibility 29 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijca.2020.085
-
CrossMark
- Citation
A comparative evaluation of age based formula and ultrasonography to predict endotracheal tube size in paediatric patients
- Author Details:
-
Preeti Gehlaut
-
Mayuri Golhar *
-
Sanjay Johar
-
Prashant Kumar
-
Ravi Nain
Introduction
Paediatric airway is a challenging due to developmental anatomical variations. Paediatric airway is funnel-shaped and cricoid cartilage is the narrowest portion in contrast to the cylindrical shaped adult airway, where the narrowest portion is the glottis.[1]
Optimal sized ETT selection is of utmost importance in paediatric patients because both over and under sized tubes can cause complications like air leak, aspiration, insufficient ventilation, oedema, ulceration, necrosis of subglottic region, post-extubation stridor and subglottic stenosis.[2], [3]
Various formulae based on age, weight, height and finger diameter have been used traditionally to determine appropriate sized ETT in paediatric patients. However, these methods are not always suitable because the size of the airway varies considerably between patients and the smallest diameter cannot be reliably predicted by height or weight.[4]
Recently, USG has come up as an excellent, non-invasive, portable and real time imaging modality for airway management. With the help of USG, the anatomical structures in the supraglottic, glottic and subglottic regions can be visualised and prediction of appropriate size ETT is possible.[5], [6]
Keeping this in mind, a prospective observational study was planned to investigate the reliability of ultrasonography for determination of endotracheal tube size in paediatric patients and its comparison with age based Motoyama formula in terms of outer diameter determination of endotracheal tube.
Materials and Methods
After approval from Institutional ethics committee, and written informed consent from parents or guardians, 64 pediatric subjects aged between 2-12 years belonging to American Society of Anaesthesiologists Physical Status I & II, scheduled for surgeries under general anaesthesia with endotracheal intubation were enrolled in study.
The patients having anticipated difficult airway, any anatomical deformity of upper airway, presence of scar, ulcer or mass in the neck, previous surgery in the neck, upper respiratory tract infection were excluded.
All the patient underwent pre-anaesthetic evaluation with detailed history and general physical examination. Patients were kept nil per oral for 6 hours for solids and 2 hours for clear fluids prior to surgery.
On the day of the surgery, patient was taken into the operating room and routine monitoring was established for heart rate (HR), electrocardiography (ECG), pulse oximetery (SpO2), non-invasive blood pressure (NIBP) and end tidal CO2 (EtCO2) and baseline readings were recorded.
General anaesthesia was induced as per the discretion of attending anaesthesiologist. After loss of consciousness and confirmation of bag and mask ventilation, loading dose of neuromuscular blocking agent, injection atracurium 0.5mgkg-1 was given and patient was ventilated for 3minutes, using close circuit. The ultrasonography of subglottic space was performed with temporary cessation of respiration and this apnoea interval was also noted.
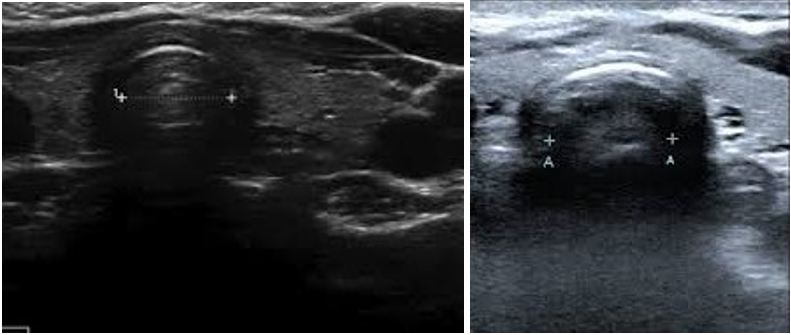
The subglottic diameter was estimated with high resolution B-mode ultrasonography (USG) with a linear array transducer (frequency 6-13 MHz, depth 6 cm, M-Turbo Sonosite ultrasound machine) positioned in the midline of neck, with the patient’s head extended and neck flexed (the sniffing position). The transverse air column diameter at the cephalic half of the cricoid cartilage that is narrower than the caudal part was measured.[7] ([Figure 1])
The ETT with the nearest OD corresponding to the measured subglottic diameter was chosen, recorded and patient was then intubated using direct laryngoscopy. ETTs from same manufacturer were used to prevent bias due to difference in size of outer diameter of ETTs from different manufacturers. If resistance was encountered while passing the tube through the larynx, a tube one size smaller (−0.5 mm ID) was selected and recorded.
After confirmation of correct placement of ETT, the air leak test was performed to confirm the appropriate ETT size and find out the clinically best fit ETT, for every patient.
The air leak test was performed while maintaining the patient’s head and neck in neutral position. A closed circuit was connected to the ETT and flow rate was set to 5Lmin-1, with a closed adjustable pressure limiting valve allowing the circuit to fill up and pressurize to a circuit pressure of 30 cmH2O. Then the flow meter was closed fully and fall in pressure was noted for 10 seconds, when the pressure equilibrates to a new value at the end of 10 seconds.
This new value of circuit pressure at the end of 10s was used to decide whether the used ETT was of appropriate size or not. It was considered appropriate, if the circuit pressure equilibrates to 10–20 cmH2O after 10s, ETT was considered large, if the circuit pressure equilibrates at >20cmH2O and size was considered as small if it equilibrates to <10 cmH2O after 10s.
If the tube size was found small or large, it was changed to next ETT by 0.5mm difference and leak test was repeated to confirm the appropriate size. Cuff pressure of the ETT was maintained between 18-20 cmH2O using aneroid manometer.
Following observations were recorded heart rate, SpO2 and NIBP and EtCO2 throughout the procedure and recorded at baseline level, after induction, after endotracheal intubation and at ten minutes intervals, thereafter, Subglottic tracheal diameter measurement in millimetres (mm) using USG, Internal diameter of the ETT selected corresponding to the outer diameter measured from USG (ETTUSG), Clinically best fit ETT, actually used (ETTA), as determined by the air leak test, No. of times ETT change required in each patient, Total time needed for USG scanning to measure the tracheal diameter, in seconds (Ttotal). Size of ETT calculated in each patient as per age based formula[8] Motoyama formula: ID (mm) = (age)/4+3.5 (ETTM), a comparison of ETT size estimated by USG, age-based Motoyama formula and that finally used clinically was done, based on the above recorded observations.
Based on power of the study being 80% and confidence interval (CI) of 95%, considering a clinically meaningful difference of 0.5 and standard deviation of 1 (double of the clinically meaningful difference), sample size was 62 as calculated in a previous study. We have considered a sample size of sixty four patients in our study.
The data analysis was performed using IBM SPSS version 20.0 software. Quantitative variables were expressed as mean±sd and compared across follow-ups using paired t-test. A p-value < 0.05 is considered statistically significant.
Results
Comparable pattern was seen in the demographic and physical characteristics of all 64 patients ([Table 1]).
| Frequency n = 64 | |
| Mean age ± SD | 5.95±3.22 year |
| Male:Female | 43:21 (67% males and 33% females) |
| Mean Weight ± SD | 18.77±8.75kg |
| Mean Height ± SD | 113.19±17.15 cm |
| BMI ± SD | 13.78±2.82 kg/m2 |
Haemodynamic parameters HR, NIBP(systolic), NIBP(Diastolic), Spo2 and EtCo2 when compared at different times, no significant changes were observed after ET intubation and at other time points. ([Table 2])
| Baseline | After Induction | After ET intubation | After 10min | After 20min | After 30min | |
| HR ± SD | 97.47 ±7.54 | 104.66 ±7.8 | 111.28 ±6.81 | 101.48 ±4.37 | 97.34 ±4.3 | 97.13 ±5.74 |
| SBP ± SD(mmHg) | 111.91 ±3.04 | 108.59 ±2.54 | 115.98 ±3.67 | 110.27 ±3.48 | 109.16 ±3.48 | 113.97 ±4.88 |
| DBP ± SD(mmHg) | 77.47 ±3.25 | 73.48 ±3.9 | 81.66 ±3.26 | 76.88 ±2.28 | 75.47 ±2.97 | 80.84 ±2.82 |
| Spo2 ± SD | 100 ± 0 | 100 ± 0 | 100 ± 0 | 100 ± 0 | 100 ± 0 | 100 ± 0 |
| EtCo2 ± SD(mmHg) | 35.42 ±1.88 | 36.09 ±2.43 | 37.98 ±2.57 | 37.83 ±1.92 | 37.84 ±3.4 | 37.31 ±1.25 |
Mean of size of endotracheal tube diameter as calculated by using age based Motoyama formula was 4.86±0.82 mm.
Mean subglottic diameter as measured using ultrasonography was 7.1±1.12 mm. Mean of outer diameter corresponding to subglottic diameter measured by USG was 7.1±1.07 mm. Mean value of ID corresponding to OD as measured by USG was 5.18±0.74 mm.
Total time taken for each USG scanning was noted and mean time taken by USG was 11.92±1.46 seconds.
Mean of the clinically best fit ETT as determined by air leak test was 5.15±0.68 mm. This value is almost similar to mean of ID corresponding to OD measured by USG and more than mean of ETT size calculated by age based Motoyama formula. Comparison between ETT calculated by USG, by age based Motoyama formula and clinically fit ETT is shown in [Table 3].
| Diameter (mm) | Mean | ±sd |
| Subglottic diameter measured by USG (in mm) | 7.1 | ±1.12 |
| OD of ETT corresponding to USG measured subglottic diameter (in mm) | 7.1 | ±1.07 |
| ID corresponding to OD (in mm) | 5.18 | ±0.74 |
| Clinically best fit ETT used as determined by air leak test (in mm) | 5.15 | ±0.68 |
| ID of ETT calculated by age based Motoyama formula (in mm) | 4.86 | ±0.82 |
| Total time taken for USG (in seconds) | 11.92 | ±1.46 |
The Intraclass correlation coefficient (ICC) between the two measurements (Clinically Best fit ETT and ID corresponding to OD measured by USG) was significantly positive and very high (r = 0.981, p-value < 0.001) which indicates a close concordance between the two measurements.
The mean ID corresponding to OD measured by USG was 5.18±0.74 mm which is not significantly different from that of the clinically best fit ETT where it is 5.15±0.68 mm (p-value < 0.051).
The ICC between the two measurements (Clinically Best fit ETT and age based Motoyama formula) was significantly positive and very high (r = 0.927, p-value < 0.001), indicating a close concordance between the two measurements. However, the mean ID corresponding to clinically best fit ETT was 5.15±0.68 mm which is significantly higher than that of the ID corresponding to Age based Motoyama formula where it is 4.86±0.82 mm (p-value < 0.001). This shows that Motoyama's formula significantly underestimates the ID by 0.32±0.3 mm.
In our study ETT was changed one time in 9 (14%) cases and changed 2 times in 4 cases (6.25%) and majority of cases i.e. 80% did not need change of ETT as shown in table 4 and figure 3.
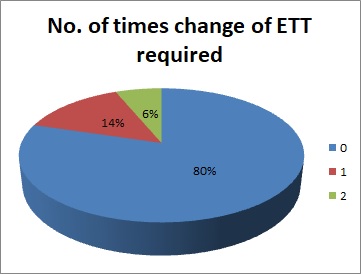
| No. of times change of ETT required | N | % |
| 0 | 51 | 79.69% |
| 1 | 9 | 14.06% |
| 2 | 4 | 6.25% |
| Total | 64 | 100% |
| mean±sd | 0.27 | ±0.57 |
Discussion
ETT size selection in children is very important and has traditionally been done on basis of various physiological formulas and parameters rd formula where ID (mm) = 16+ (age)/4 and for cuffed ETT Motoyama’s formula which is applicable in children aged 2 year or older, where, ID in mm = (age in years)/4+3.5. Methods like x-ray neck, computed tomography (CT) of the neck and MRI of neck have also been tried. Though, MRI has been found to be highly accurate, it is time consuming, costly and not practical in routine anaesthesia practice.[7], [9], [10], [8], [11] Ultrasonography (USG) unlike CT and MRI does not require strict immobility of patient. USG requires training, yet relatively simple to learn.[12] USG is a reliable for evaluation of the upper airway’s narrowest transverse diameter at the subglottic region and may be helpful to estimate the proper size of ETT.
The results of USG have been compared with Magnetic Resonance Imaging (MRI) for the purpose of subglottic diameter measurement in 19 adult patients by Lakhal et al and the results were found comparable. They concluded that in young healthy adults, ultrasonography appeared to be a reliable tool to assess the diameter of the subglottic upper airway. Keeping this in mind, a prospective observational study was planned with an aim to assess the narrowest transverse diameter of the trachea at the subglottic region by USG in paediatric patients, to estimate the ETT size and compare it with the existing age based formulae.
In our study a total of 64 patients were enrolled out of which 21% belonged to 2-3 years of age and 19% were aged 3-6 years. The mean age is 5.95±3.22 years. Gupta et al enrolled children aged 3 to 18 years. Their range of age involved both pediatric age group and young adults. Whereas, Sibasaki et al measured the subglottic diameter in patients aged 1 month to 6 years. We chose a more uniform age range as airways are rapidly growing during infancy and challenges are more regarding safely securing an airway.[13], [14]
Mean weight and height of the 64 children recruited in this study was 18.77±8.75 kg and 113.19±17.15 cm, respectively. The hemodynamic parameters were within normal limits throughout the duration of surgery, in all the patients as standard anaesthesia technique was followed.
Rajasekhar et al measured subglottic diameter using USG in awake children aged 6 months to 8 years of age. In their study, ultrasonography was performed by a single experienced operator for every case. In our study, measurement of the subglottic diameter was done after induction of anaesthesia and after administration of neuro-muscular blocking agent, during the apnoea ventilation. We also withheld the ventilation temporarily while making the ‘actual’ measurement and duration of apnoea was noted for all the patients in seconds, so as to avoid any kind of movement while making the measurements.[15] The time required for ultrasonographic estimation was less than one minutes in all patients and the mean time taken by USG was 11.92±1.46 seconds.
In our study, we recorded the number of times change of an ETT was needed based on the leak test to determine a clinically ‘best fit’ ETT. Almost 80% (79.69%) patients didn’t require any change in the endotracheal tube and an appropriate sized ETT was inserted in the first instance as calculated by USG measurements. 14% and 6% patients needed change of ETT one tine and two times respectively as the subglottic diameter was overestimated in these cases by USG measurements. However, mean of the clinically best fit ETT was 5.15±0.68 mm. This value is almost similar to mean of ID corresponding to OD measured by USG and more than mean of ETT size calculated by age based Motoyama formula, which is an age based formula.
The Intraclass correlation coefficient (ICC) between Clinically Best fit and ID corresponding to OD was significantly positive (r = 0.981, p-value < 0.001). ICC between Clinically Best fit and age based Motoyama formula was also significantly positive (r = 0.927, p-value < 0.001). This indicates that there was a close concordance.
Our results correlate to those of Altun et al who found an ultrasound determined best fit ETT in 88% of children in their study. In another study by Shibasaki et al a low incidence of a need to change the tube was reported, as their success rate of placing a correct fitting ETT was 96%.[13], [16]
Limitations of the present study are this was a descriptive study performed in a single hospital setting, so, a larger multicentric prospective study would be able to validate the results. The limitations of ultrasonography should also be considered as it measures the transverse diameter of the trachea at one level which is subject to variations due to pressure on tissues. We did not include the subjects below two years of age because transverse diameter is difficult to measure in these cases and did not include children with difficult intubation or existing anatomical malformations.
Conclusion
Ultrasonography proved to be a reliable predictor for the assessment of the subglottic diameter of the airway in children to estimate the appropriate endotracheal tube size for intubation as compared to age based formula.
It is a safe, reliable, non-invasive tool for selection of appropriately sized endotracheal tube for clinical use and can prevent trauma to the patient by the repeated attempts on intubation or insufficient ventilation. However, larger size multicenteric trials should be conducted to further validation.
Source of Funding
None.
Conflict of Interest
None.
References
- L Adewale. Anatomy and assessment of the pediatric airway. Paediatr Anaesth 2009. [Google Scholar]
- M Weiss, A Dullenkopf, C Gysin, C.M. Dillier, A.C. Gerber. Shortcomings of cuffed paediatric tracheal tubes † †Declaration of interest. The investigated paediatric cuffed tracheal tubes were ordered from local distributors and partially provided without charges. No financial support was obtained for the presented work. Dr Weiss and Dr Gerber are actually involved in designing a new cuffed paediatric tracheal tube in co-operation with Microcuff GmbH, Weinheim, Germany.. Br J Anaesth 2004. [Google Scholar]
- W L Roy. Intraoperative aspiration in a paediatric patient. Can Anaesth Soc J 1985. [Google Scholar]
- A Randestad, Carl-Eric Lindholm, Peter Fabian. Dimensions of the Cricoid Cartilage and the Trachea. Laryngosc 2000. [Google Scholar]
- Kumkum Gupta, PrashantK Gupta, Manish Jain, Atul Krishan, Bhawna Rastogi, Gouri Garg. Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res 2012. [Google Scholar]
- J Y Bae, H J Byon, S S Han, H S Kim, J T Kim. Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for paediatric patients. Anaesth 2011. [Google Scholar]
- Brent R King, M Douglas Baker, Leonard E Braitman, Jessica Seidl-Friedman, Mark S Schreiner. Endotracheal tube selection in children: A comparison of four methods. Ann Emerg Med 1993. [Google Scholar]
- E K Motoyama, P J Davis, F P Cladis. . Endotracheal intubation. In Smith's anesthesia for infants and children 1990. [Google Scholar]
- Robert C Luten, Robert L Wears, James Broselow, Arno Zaritsky, Theodore M Barnett, Terry Lee. Length-based endotracheal tube and emergency equipment in pediatrics. Ann Emerg Med 1992. [Google Scholar]
- F Cole. Pediatric formulas for the anesthesiologist. AMA J Dis Child 1957. [Google Scholar]
- P A Hudgins, J Siegel, I Jacobs, C R Abramowsky. The normal pediatric larynx on CT and MR. AJNR Am J Neuroradiol 1997. [Google Scholar]
- Paul Raphael, Ershad Thasim, Binu Simon, P Rajagopal. Comparative study on prediction of paediatric endotracheal tube size by ultrasonography and by age based formulas. Int J Res Med Sci 2016. [Google Scholar]
- Masayuki Shibasaki, Yasufumi Nakajima, Sachiyo Ishii, Fumihiro Shimizu, Nobuaki Shime, Daniel I. Sessler. Prediction of Pediatric Endotracheal Tube Size by Ultrasonography. Anesthesiol 2010. [Google Scholar]
- Kumkum Gupta, PrashantK Gupta, Manish Jain, Atul Krishan, Bhawna Rastogi, Gouri Garg. Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res 2012. [Google Scholar]
- M A Rajasekhar, S Moningi, S Patnaik, P Rao. Correlation between ultrasound-guided subglottic diameter and little finger breadth with the outer diameter of the endotracheal tube in paediatric patients-A prospective observational study. Indian J Anaesth 2018. [Google Scholar]
- Demet Altun, Mukadder Orhan-Sungur, Achmet Ali, Tülay Özkan-Seyhan, Nükhet Sivrikoz, Emre Çamcı. The role of ultrasound in appropriate endotracheal tube size selection in pediatric patients. Pediatr Anesth 2017. [Google Scholar]
