Introduction
Spinal anaesthesia being widely used because of its fast onset with effective sensory and motor blockade compared to general anesthesia it is easy to perform and also has a good muscle relaxation property with added advantages like preventing airway manipulations, pressor response from intubation, nausea, vomiting, sore throat, excessive sedation and polypharmacy compared to general anesthesia.
Spinal anesthesia is a preferable technique for lower abdominal surgeries as it provides effective sensory and motor block with rapid onset, attenuation of stress response and less thromboembolic episodes. Bupivacaine is most commonly used spinal anesthetic agent. Bupivacaine (1-butyl-2', 6'-pipercoloxylidine) is an aminoamide which was first synthesized in the laboratories of Bofors Nebel-Pharma, Sweden and first described by Af Ekenstam et al in 1957.1 The molecular structure of bupivacaine is a highly protein-bound compound containing a chiral center on the piperidine ring, resulting in two optically active stereoisomer [i.e., levorotatory (S-) and dextrorotatory (R+) configurations]. However, since its introduction into clinical practice in the early 1960s, bupivacaine has been marketed at 50:50 racemic mixtures of the two enantiomers.
Due to the adverse cardiac effects of racemic bupivacaine, several studies have been performed in order to find anesthetic compounds to take its place. (S-) bupivacaine (levobupivacaine) has been recognized to have less cardiovascular and central nervous system toxicity.2, 3 Epidural levobupivacaine has the advantage of decreased cardiotoxicity in cases of accidental intravascular injections.4, 5 It is currently known that levobupivacaine and racemic bupivacaine have similar analgesic potencies for epidural and spinal anesthesia, brachial plexus blocks, and local infiltration; however, levobupivacaine tends to induce more sustained sensory and motor block.6, 7, 8
Both anesthetics share many pharmacokinetic properties. Therefore, preliminary clinical experience reveals that the efficacy of both local anesthetics is more or less equal.9, 10 Volunteers were recruited to assess the clinical profile of spinal bupivacaine and levobupivacaine. Several published studies have compared solutions of 0.5% isobaric bupivacaine and levobupivacaine without an adjunct in spinal anesthesia via different surgical techniques: hip/knee replacement, urological, lower abdominal, and lower extremity surgery.11, 12 More recently, the toxicity of levobupivacaine has reassessed to determine its potential benefits for clinical use. Compared to plain solutions, hyperbaric solutions are expected to provide a more predictable block with fewer side effects i.e. high block, hypotension, nausea, vomiting, and pruritus.13 However, the relevant literature about the choice of baricity of intrathecal solutions is inconsistent and lacks data about their relative benefits and adverse effects. As of today only very few studies had been conducted in India comparing the efficacy between bupivacaine and its isomer and so the present study was done to evaluate the efficacy between 0.5% isobaric Levobupivacaine and to 0.5% racemic Bupivacaine.
Aim
To compare and evaluate the efficacy between 0.5% isobaric Levobupivacaine and 0.5% racemic Bupivacaine in spinal anesthesia among the patients undergoing lower abdominal and lower limb surgeries.
Materials and Methods
A prospective comparative study was conducted for a period of one year at our hospital under the department of anesthesia. The study was started after getting the approval from the institutional ethical committee. Based on purposive sampling 200 subjects were selected for the study and were divided into two groups. The patients were selected in the age group between 20 and 60 years with ASA physical status 1 or 2. Patients who were posted for elective lower limb and lower abdominal surgeries were included in the study and patients with ASA score 3 or 4, aged below 20 or above 60 and patients having hypersensitivity to the drugs given through spinal anesthesia were excluded from the study. Informed consent was obtained from all the study subjects before the start of the study. The study subjects were randomly allocated into two groups of 100 each. Group B subjects received 3ml of 0.5% intrathecal hyerbaric Bupivacaine (15 mg) and group L patients received .5% intrathecal Isobaric Levobupivacaine (15 mg). All the patients had a pre-anesthetic work up with a detailed history, general and systemic examination and the routine blood examination. All the patients received a pre-anesthetic medication of 0.5 mg alprazolam and 150 mg ranitidine with few sips of water. Subjects were monitored non-invasively for blood pressure, peripheral oxygen saturation (SpO2), and electrocardiography evaluations. Spinal anesthesia was performed using a 24-gauge Quincke needle with a midline approach at L3-4 (determined by palpation of the bony landmarks). Injection was done slowly (at least 10 seconds) without Barbotage’s technique by the previously mentioned anesthesiologist, who was blind to the type of local anesthetic. The surgical procedure was started 20 min after initiation of the spinal injection or as soon as an analgesic level at T10 was established. Otherwise, general anesthesia was applied.
Intraoperatively, the patients received 2 mL/kg/hr 0.9% saline solution. After spinal injection, the patients were turned into a supine position with a pillow under their head. Oxygen (2-3 L/min) was given via a face mask. Sensory blockade was assessed by the pinprick test on each side of the midclavicular line and motor blockade was assessed based on a modified Bromage scale (0=no motor block, 1=inability to raise extended legs, 2=inability to flex knees, and 3=inability to flex ankle joints). These tests were performed on the 1st, 3rd, and 5th min, then every 5 min up to the 30th min, and then every 10 min until the end of the operation.
Postoperatively, the testing was done on the 5th and 10th min and every 10 min until the sensory and motor variables became normal. Postoperative quality of analgesia was evaluated with visual analogue scale (VAS) — from 0 to 10 where 0 defines no pain and 10 defines the worst pain ever suffered. Patients who had a VAS score ≥4 were given i.m. 75 mg diclofenac and the time of analgesic administration was recorded as the time for postoperative analgesic requirement. The hemodynamic variables and SpO2 were recorded one hour before spinal anesthesia (immediately before the saline infusion) and on the 1st, 3rd, and 5th min, every 5 min up to the 30th min, and then every 10 min until the end of the operation. Postoperatively, all hemodynamic variables were recorded on the 5th and 10th min and every 10 min for 90 min. Hypotension was defined as a decrease in systolic blood pressure >30% from baseline and was treated with 5 mg intravenous (IV) ephedrine. Bradycardia was defined as a heart rate <45 bpm and was treated with 0.5 mg IV atropine. Nausea/vomiting were recorded and 10 mg IV metoclopramide was administered for treatment. If the sedation score was 1, supplementary sedation was provided with 2 mg i.v. midazolam.
All the data were entered and analysed using SPSS version 21. The parametric variables between the two groups were analysed using student T test and for the non-parametric variables chi-square test was used to derive the statistical inference considering p<.05 as statistically significant.
Results
The demographic details of the study subjects were tabulated in Table 1. It is seen from the table that the majority of the study subjects in both the groups were in the age group between 30 and 40 years with a mean age among bupivacaine group was 38.6 years and Levobupivacaine group was 39.4 years and male : female ratio among both the groups was 1.5: 1. The mean height and the body surface area between the two groups did not show a statistical significant difference and the mean duration of surgery in both the groups ranges between 60 – 65 mins.
There were no significant differences between the two groups in the quality of sensory and motor block as shown in Table 2. The peak block height of the levobupi-vacaine and bupivavacine group was T4 and average in both groups were T9. .68% of patients in group L and 44% of patients in group B achieved a maximum sensory blockade of up to T8 dermatomal level. No statistically significant difference was seen in the onset of sensory, motor blockade and the duration of complete motor blockade. Complete motor blockade was eventually achieved in 98 patients in the levobupi-vacaine group (98%) and 96 patients in the bupivacaine group (96%). Only highest level of sensory block showed slightly statistical difference. No patient had anesthesia rated as failure or unsatisfactory by the operating surgeons. For assessment of pain with VNPS at the start of the operation when 0 is no pain and 10 is the worst imaginable pain. There were rated VPNS score, with 0 at the time the operation started in both groups. None of the seventy patients required supplement analgesics during the operative procedure. There was neither significant difference in recovery of sensory and motor, time to S1 sensation recovery. No evidence of postural hypotension after recovery of dorsiflexion of the great toe in all the hundred patients.
Figure 1 shows the comparison of the heart rate from baseline to a period of 180 mins. It is observed that there was a fall in heart rate among the bupivacaine group patients in the first 15 mins of spinal anesthesia and this fall had shown a statistical significant difference in comparison with levobupivacaine group but later on there was no significant difference in the pulse rate between the two groups. The blood pressure comparison between the two groups over a period of time was represented as a line diagram in Figure 2 and Figure 3. It infers that both the systolic blood pressure and the diastolic blood pressure had shown a statistically significant fall in the bupivacaine group during the first 15 mins after the infusion of spinal anesthesia in comparison with the patients who had received levobupivacaine but later on the blood pressure was maintained almost similar in both the groups. The oxygen saturation values did not show a statistical significant difference between the two groups both at the initial and later stages, it was almost similar in both the groups (Figure 4). Among the various side effects reported in both the groups the incidence of hypotension and bradycardia was more among the bupivacaine group than that of the levobupivacaine group and the difference was found to be statistically significant (p<.05), whereas the incidence of nausea, vomiting or respiratory depression did not show a statistical significant difference between the two groups (Table 3).
Table 1
Demographic profile of the study subjects
Table 2
Comparison of sensory and motor blockade between the two groups of our study subjects
Figure 1
Line diagram showing the comparison of pulse rate between Group B (hyperbaric bupivacaine) and Group L (isobaric levobupivacaine)
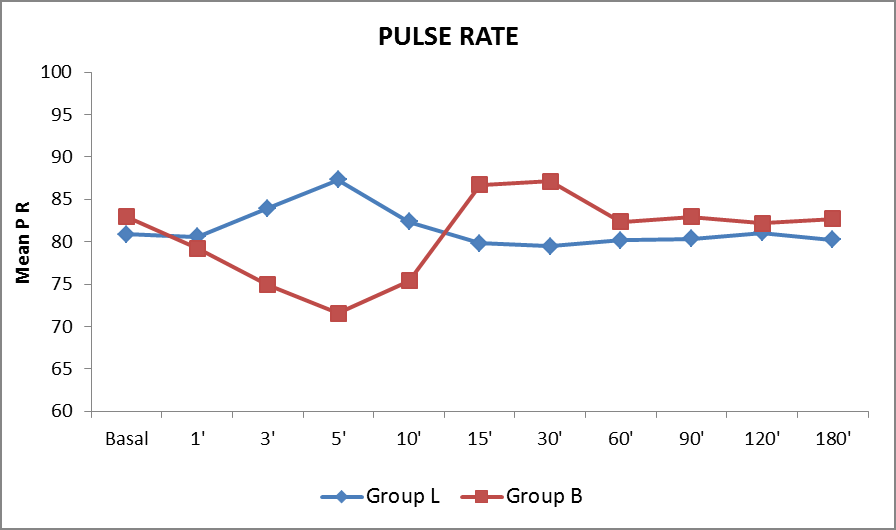
Figure 2
Line diagram showing the comparison of systolic BP between Group B (hyperbaric bupivacaine) and Group L (isobaric levobupivacaine)

Figure 3
Line diagram showing the comparison of diastolic BP between Group B (hyperbaric bupivacaine) and Group L (isobaric levobupivacaine)

Figure 4
Line diagram showing the comparison of oxygen saturation between Group B (hyperbaric bupivacaine) and Group L (isobaric levobupivacaine)

Discussions
Sub arachnoid block is a commonly employed anaesthetic technique for performing surgeries of the lower abdomen and lower limb. It is a safe, economical and easy to administer technique which also offers a high level of post anaesthesia satisfaction for the patient. The technique is simple, has rapid onset and is reliable. The risk of general anaesthesia including mishaps due to airway management is avoided by this technique. Bupivacaine is a local Anaesthetic used routinely for spinal anaesthesia because of its high potency and minimal neurologic symptoms. Levobupivacaine is increasingly popular in replacement of bupivacaine because of its equipotency with lower cardiovascular and central nervous system side effects. It has very similar pharmacokinetic properties to those of racemic bupivacaine, several studies supported the notion that its faster protein binding rate reflects a decreased degree of toxicity.14 Hence the present study was conducted to assess the anaesthetic potency and hemodynamic effects of intrathecally administered Levobupivacaine compared with intrathecal administered racemic Bupivacaine in patients coming for surgeries of lower abdomen and lower limb. The equipotent ratio between Levobupivacaine and Bupivacaine is considered to be 0.97.15 Since hyperbaric Levobupivacaine is not available in the market, we chose isobaric 0.5% Levobaupivacine 15 mg and isobaric 0.5% Bupivacaine 15 mg as as an equipotent dose for this study. In our study majority were middle aged among group L and B and the male: female ratio was 1.5: 1 among both the groups with their mean height being identical. All these parameters were kept identical in both the groups to avoid variations in intraoperative and post-operative outcome of the patients. In the present study we found that there was no statistical significant difference in sensory and motor blockade among the bupivacaine and levobupivacaine groups. The majority of the clinical studies that have compared levobupivacaine and bupivacaine have discovered few differences between them and report that both anesthetics perform similarly.16, 17, 18 In a randomized, double-blind prospective study, Glaser et al compared isobaric solutions (3.5mL of 0.5% levobupivacaine; 3.5mL of 0.5% bupivacaine) in 80 patients undergoing elective hip replacements found no clinical differences and concluded that both drugs were equipotent and offered similar durations, onset times, and degrees of motor and sensory blockades.19 After comparing 3mL of 0.5% spinal bupivacaine and levobupivacaine for hip surgery, Fattorini et al. found that there were no significant differences in spinal blockade characteristics.20 Sathitkarnmanee et al conducted a study with 70 patients to compare 0.5% isobaric levobupivacaine (3mL) versus 0.5% isobaric bupivacaine (3 mL) for elective lower limb and lower abdominal surgery with spinal anesthesia and found no significant differences in the quality of motor and sensory blockades between both groups.21 Lee et al. compared the efficacy of 2.6 mL of an isobaric solution of 0.5% levobupivacaine with 0.5% racemic bupivacaine in TUR surgery, and observed that there were no significant differences in quality of sensory and motor block or hemodynamic change.15
In the present study there was reduction in both systolic blood pressure and diastolic blood pressure in both the groups but the magnitude of fall was more in group B than in group L. The pronounced fall in blood pressure was more from 1st minute after spinal injection up to 15 minutes after the injection in group B. The incidence of hypotension was more in group B (52% patients) compared to group L (16% patients) which had shown a statistically significant difference between the two groups. Our results were in par with the study conducted by M Mantouvalou, et al22 on one hundred-twenty ASA I-III patients in which he observed that 42.5% patients of Bupivacaine group had hypotension compared to 17.5% patients of Levobupivacaine group and a similar study done by F. Erdil et al also noted that there was significant hypotension following spinal anaesthesia in Bupivacaine group (30% patients) compared to levobupivacaine group (10% patients).23
Bradycardia was a notable observation in our study, 30% patients in group B had bradycardia compared to 8% patients of group L. Mantouvalou, et al22 in their study observed that 12.5% of patients in Bupivacaine group had bradycardia whereas 10% patients in levobupivacaine group had bradycardia. This was also a noted feature in the study conducted by F. Fattorini et al24 and few more studies had provided the evidence that levobupivacaine is less cardiotoxic and neurotoxic than bupivacaine25, 26 but a study done by Monica del etal had quoted that there was no differences between both agents for hemodynamics and incidence of side effects.27
Conclusion
The results of the present study indicate that 3 ml of 0.5% isobaric levobupivacaine and 0.5% hyperbaric of racemic bupivacaine show equally effective potencies for spinal anesthesia, both regards to the onset time and duration of sensory and motor blockade and also for two segment sensory block regression time. Bupivacaine group patients required more often the use of vasoactive drug ephedrine and of a sympathomimetic drug atropine when compared to Levobupivacaine. So Levobupivacaine with the same potency and lesser cardiovascular side effects could be considered as a better alternative for bupivacaine.
