Introduction
Post operative nausea and vomiting (PONV) continues to be a common complication of pregnancy as pregnant women are always considered full stomach. PONV during spinal anesthesia for elective cesarean delivery may occur in upto 66% of patients.1 PONV is a leading cause of admission after planned ambulatory surgery and may lead to dehydration, bleeding, surgical wound complications, and aspiration of gastric contents. The usual drugs used for prevention or treatment of this have adverse effects such as intense sedation, dystonic reactions, restlessness and extrapyramidal symptoms.2 Chewing gum has been prospectively evaluated as a therapy to reduce postoperative nausea and vomiting in breast and laparoscopic surgery.3 Postulated mechanisms of its effect surround the principle of ‘sham feeding’, which stimulates bowel motility via cephalic- vagal stimulation.3 Chewing gum has also been linked to lower cortisol concentrations, improve stress and anxiety, and more positive mood in the research setting.4
Materials and Methods
This was a Prospective Randomized Trial done from May to June 2018 in the Department of Anaesthesiology and Critical Care, Vani Vilas Hospital, Bangalore Medical College and Research Institute, Bangalore. The study was approved by the Institutional Ethics Committee and registered with CTRI/2019/05/026011. A total of 120 patients were screened and 100 patients were included in this study. The patients who gave written informed consent with ASA-I or ASA-II posted for elective caesarian delivery were included in the study. The other inclusion criteria were patients between 19-35 years of age and with full term singleton pregnancy. Patients with essential hypertension, pre-eclampsia, diabetes, anemia, heart disease, multiple pregnancy, fetal distress, abruptio placentae/placenta previa, any contraindication to spinal anaesthesia, known allergy to local anesthetics, unable to chew gum or complaining of gum or dental problems and who could be exposed to any intra-operative and post-operative complications were excluded from the study.
Pre-operative evaluation was done a day before scheduled surgery. After explaining the procedure, the patients were advised overnight fasting. Spinal anesthesia was given to all patients in left lateral position with 2ml of 0.5% bupivacaine heavy in L3 L4 space. The patients were randomly assigned into two equal groups of fifty each.
Based on the observer’s assessment, when a score of five in alertness/sedation was achieved and the patient was not sleeping in between observations, patients in Group I were given one strip of sugar free gum to be chewed for 30 minutes every eighth hourly.
Table 1
The observers’ assessment of alertness/sedation score
Patients randomized to Group-II received Inj. Ondansetron 4mg intravenously immediately after cesarean section. Rescue anti-emetics i.e Metaclopramide 10mg IV / Dexamethasone 4mg IV/ Prochlorperazine 12.5mg IV/ Droperidol 0.625mg IV/ Promethazine 6.25mg IV were planned to be used if the first-line therapy was not fully successful.
The primary outcome measures were the number of episodes of nausea or vomiting immediately after surgery and at 6th, 12th, 18thand 24th hour post-operatively. The secondary outcome measures included: 1) The relief of PONV as graded on a four-point verbal descriptive scale, 2) Five point Likert scale for acceptability, 3) Use of rescue medication for the first 24 hours after surgery 4) Sedation, as assessed with RAMSAY sedation scale and 5) Time to first flatus.
Statistical analysis
Random allocation of patients in the ratio of 1:1 was done using simple randomization technique. A targeted convenience sample of 100 patients (50 in each arm) was taken to guide a future large randomized controlled trial. The normal data was summarized using the Mean ± SD and compared using Student’s unpaired two-tailed t-test. Categorical data was summarized using the number and compared using the chi-square test or Fisher’s exact test where applicable. Pearson's ‘r’ correlation was used to assess correlation of treatment and responses on Likert scale. A value of p <0.05 was considered statistically significant. Statistical analysis was done using SPSS 16.0.
Results
There was no statistical difference found between the baseline characteristics i.e. Age and gestational age (Table 2) confirming inclusion of a homogenous population. One patient in chewing gum group and 15 patients in Ondansetron group had episodes of nausea at 6th hour postoperatively, whereas one patient in chewing gum group and seven patients in Ondansetron group had PONV at 12th hour. However, rescue medication was not required for these patients. It was observed that there was statistically significant difference between the two groups at 6th and 12th hour where the maximum number of events of PONV had occurred.
Table 2
Demographic characteristics, PONV at different intervals and time to first flatus in the patients
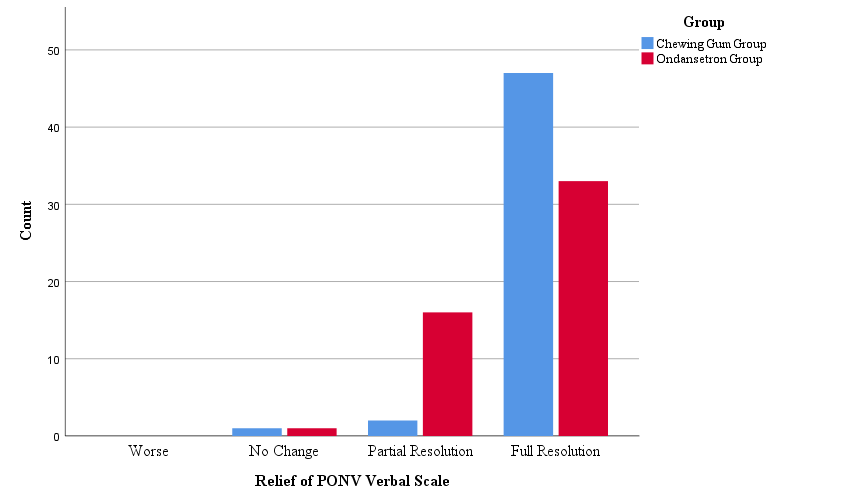
On the scale for relief of PONV, it was observed that there was full resolution of PONV in more number of patients in chewing gum group than in the Ondansetron group (Figure 1).
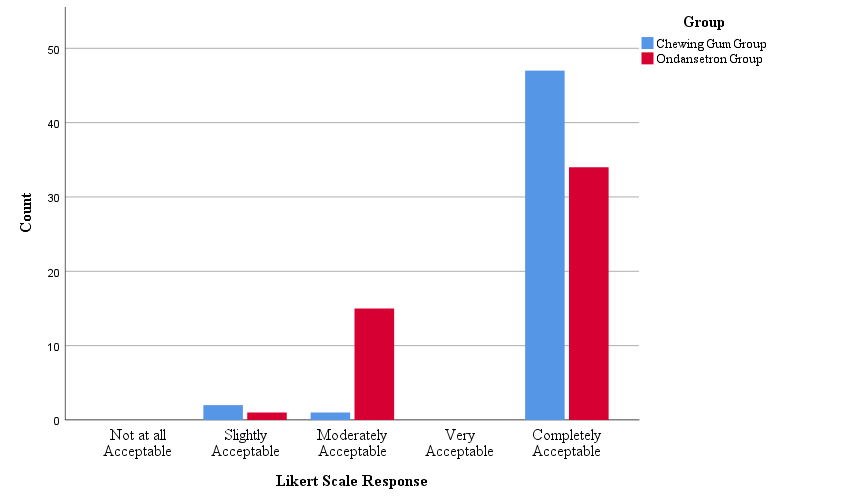
In the Likert scale response, the patients were more comfortable in the chewing gum group than in Ondansetron Group (Figure 2).
All the patients of either groups were at level two on Ramsay sedation scale.
The time to first flatus was shorter in chewing gum group than in Ondansetron group. The difference was observed to be statistically significant (Table 2).
Discussion
PONV during spinal anaesthesia for elective cesarean delivery may occur in upto 66% of patients. The risk factors of emetic symptoms in pregnancy are hormonal changes, smoking habit, age, pain, history of motion sickness or previous postoperative emesis, hypotension, surgical procedure, and anaesthetic technique.5 Our treatment groups were similar with regard to maternal demographic and operating management that considered being risk factors for postoperative emetic symptoms. Therefore, the difference in incidence and severity of nausea and vomiting among the study groups can be attributed to the study drug administration. Our data shows a beneficial effect of gum chewing in terms of better relief of post-operative nausea and shorter mean time intervals to passage of flatus (20.3 versus 29.56 hours) and acceptability.
Zhang, L et al, conducted a meta-analysis on a total of 13 RCTs which included 2233 patients. The results showed that chewing gum after cesarean delivery can effectively shorten the recovery time of bowel sounds, passage of flatus and first defecation.6
Ajuzieogu, O.V. et al conducted a study to evaluate the effect of chewing gum on post-operative ileus in 200 women who underwent cesarean sections and found that there was a statistically significant earlier onset of bowel sounds in the chewing group when compared to the control.7
Perriera, G. et al8 and Ciardulli, A. et al9 both conducted systematic reviews on more than 3,000 women (17 trials) who had just had cesarean section, mostly from Asia and the Middle East. While all the studies demonstrated a consistent improvement in rate of ileus and time to first flatus, they were largely inconsistent in demonstrating complete relief of PONV. They however do suggest that the simplicity, frugality, and safety of chewing gum makes it a viable option to offer women undergoing cesarean section.
Macones, George A. et al. have formulated the Guidelies for ERAS (Enhanced Recovery after Surgery) after cesarean delivery Part 3. They recommend the use of chewing gum in the postoperative period for early return of bowel activity. However, they consider this a weak intervention due to inability to do blinding for chewing gum in the studies reviewed in the meta-analysis.10
Sugar free chewing gum that contains the artificial sweetener sorbitol and other hexitols might be having side effect such as bloating, gas, and abdominal cramps. However, there are no such reports in this study. The intervention in our study is non-invasive, very economical and highly patient compliant. It also avoids all side effects of ramosetron, palanosetron, dexamethasone and even ephedrine which are being tried in newer studies.11, 12, 13
Conclusion
Chewing gum is considered safe, well accepted better alternative to Ondansetron for the treatment of PONV in this randomized controlled study undergoing cesarean delivery under spinal anaesthesia. It also results in rapid resumption of intestinal motility, with potential impact on reducing the overall healthcare costs in case of routine implementation.