- Visibility 141 Views
- Downloads 26 Downloads
- DOI 10.18231/j.ijca.2020.043
-
CrossMark
- Citation
Bolus dose versus fractionated dose injection of hyperbaric bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgery: A prospective study
- Author Details:
-
Nakul Srivastava
-
Pallavi Ahluwalia *
-
G S Jheetay
-
Gurpartap Singh
Introduction
Spinal Anaesthesia is a commonly used anaesthetic technique in patients undergoing lower-limb, lower abdomen, pelvis and perineum surgeries.[1], [2], [3] It is often preferred over general anaesthesia for its properties of providing a dense block, rapid action, its effect on mental status being minimal, decreased blood loss and its protective effect against thrombo-embolic complications.[4] Spinal Anaesthesia causes a sympathetic blockade by way of sympathetic denervation resulting in prolonged and occasionally severe hypotension . This occurs because of the rapid sympathetic block extension, impeding adaptation of cardiovascular system, hence causing significant morbidity and mortality.[5], [6] Fractionated dose of a Spinal Anaesthetic can also be administered, in which two thirds of the total calculated dose is initially administered; and one-third dose after a time-gap of 90 seconds, which in turn achieves adequate motor and sensory blockade.[7] The administration of fractionated dosage of the local anaesthetic agent, provides a dense block with greater haemodynamic stability.[7]
Dose of hyperbaric bupivacaine depends on factors such as weight, height and anatomy of spine for its intensity and duration of the spinal block. Attainment of appropriate sensory level for surgery incrementally correlates with height and is inversely related to weight 16. The study done by Danelli et al[8] showed that the minimum effective dose of intrathecal bupivacaine in spinal anaesthesia that would provide an effective block in 95% of parturients getting a lower segment caesarean section to be 0.06 mg/cm height. Intrathecal 0.5% bupivacaine with dextrose, is ideal for surgeries lasting for 2-2.5 hours.[9] Based on the above literature, we decided to conduct a prospective study to compare bolus dose versus fractionated dose of Hyperbaric Bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgeries and compared sensory and motor blockade as well as haemodynamic parameters. Block characteristics such as Onset, Peak, Regression of Sensory Blockade, Motor blockade, Vasopressor and Atropine requirements and VAS scoring were also compared.
Materials and Methods
After obtaining aprroval from the Institute’s Ethical Committee, and getting written informed consent, this study was carried out on 60 patients of the American Society of Anesthesiologists physical status I–II, age 18-55 years, BMI 18.5-22.9 kg/m2, undergoing surgery of lower limb under spinal anaesthesia. Based on the pilot study done by Badheka et al[7] considering the difference in MAP changes of 6 mmHg, after 15 minutes of Spinal Anaesthesia. With a α-error of 0.05 and power of study 90%, sample size in each group calculated was 28. Thus we enrolled thirty patients in each group considering the drop outs. Patients were divided into two groups by Randomisation using chit and box method. Patients with infection at the site of injection, coagulopathy, increased Intracranial Pressure, Severely altered mental status, Spine deformities or history of laminectomy, unknown duration of surgery, patients converted to general anaesthesia intra-operatively were excluded from the study.
Standard monitors were attached to the patients- non invasive Blood Pressure (NIBP), Electro-cardiogram and Pulse oximeter. Basal systolic blood pressure(SBP), diastolic blood pressure(DBP), mean arterial pressure(MAP), heart rate(HR) and Oxygen Saturation(SPO2) were taken. Intravenous(IV) line was taken with 20 gauge IV cannula. Preloading with Ringer’s lactate solution was done at 10–15 ml/kg over 10 min. Spinal anaesthesia was administered to the patients in sitting position using a 25G Quincke spinal needle in either L3–L4 or L4–L5 interspace after infiltrating skin with lignocaine (2 ml, 2%). On noticing free flow and aspiration of Cerebrospinal Fluid, Hyperbaric Bupivacaine 0.5% heavy with total dose of Hyperbaric Bupivacaine was taken as 3ml (15mg) was injected depending on respective group the patient belongs to, i.e. B or F. Group-B patients were administered a single bolus dose of 3ml (15mg) of Bupivacaine. Group-F patients were administered a fractionated dose of 3ml(15 mg) Bupivacaine with two third, i.e.,2ml (10 mg) of the total calculated dosage given initially, the syringe was kept attached to the spinal needle for remaining 90seconds, after which remaining one third dose i.e., 1ml(5mg) dose was administered. Both Bolus and Fractionated doses was administered at a rate of 0.2 ml/second. Patients were then turned in supine position (5-10° Trendelenberg). The time of onset, level and the regression of sensory and motor block was assessed. Assessment of sensory block was done and confirmed by loss of sensation to pinprick, while modified Bromage scale[10] was used to assess motor block. Surgeon was allowed incision when sensory block at T10 level and Bromage scale of three was achieved. Patients with inadequate sensory blockade and requiring conversion to general anaesthesia were excluded from the study. The assessments were performed every 2 minutes till the achievement of maximum sensory and motor block (Bromage scale 3) and every 30 minutes in the post operative period till sensory and motor variables returned back to normal. We defined onset time of sensory and motor blockade as the interval between intrathecal administration and time to achieve maximum block height(T10) and a modified Bromage score of 3, respectively. Haemodynamic parameters was recorded immediately after administering Spinal Anaesthesia, followed by every 2 minutes for the first 10 minutes of administering Spinal Anaesthesia, followed by every 3 min till the next 30 min, followed by every 5 minutes until 60 minutes of surgery. Hypotension was treated with Inj. Mephentermine 6mg IV when mean arterial pressure (MAP) decreased 20% or less from baseline. The dose and frequency of Mephentermine administered was recorded. Bradycardia (HR of < 50 beats/min), if any, was treated with Inj Atropine 0.6mg IV as per ACLS guidelines and recorded. We assessed post-operative pain every 30 minutes till 2 hours post-surgery and then each hourly for the next 4 hours to evaluate the duration of analgesia. Pain was evaluated by using a Visual Analogue Scale (VAS).[7] The duration of analgesia was defined as the time from administration of spinal anaesthesia till the first demand for rescue analgesic when VAS was ≥4. The patient was given Inj Diclofenac sodium 75 mg IM as rescue analgesic. Any incidences of nausea/vomiting, respiratory distress, shivering, pruritus were noted and treated accordingly.
Statistical analysis
We compared Quantitative variables by use of Independent t test/Mann-Whitney Test(when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using Chi-Square test/Fisher's Exact test. A p-value of <0.05 was considered statistically significant. Analysis was done using Statistical Package for Social Sciences (SPSS) version 21.
Results
Demographic data of the study population (Age, Gender, ASA Status, BMI) in study Groups B and F was comparable ([Table 1]).
| Groups | Group B | Group F | P Value |
| Mean age (years) | 31.87±9.46 | 32.77±9.90 | 0.720 |
| ASA I/II | 19/11 | 14/16 | |
| BMI | 20.86±0.96 | 20.83±1.13 | 0.922 |
| Sex (M:F) distribution | 27:3 | 27:3 |
The baseline mean arterial pressure was comparable among the two groups (88.77. ± 7.65 vs 89.17±8.42, P>0.05). Compared to Group F, Group B patients had lower mean. Mean arterial pressure post spinal, 2, 4, 6, 8, 10, 16, 33, 25, 28, 30, 35, 40, 45, 50, 60 minutes(P<0.05) ([Figure 1]).

Sensory block and motor block onset was comparable in both the groups. Sensory block peak in Group B was faster than group F (333.67±42.71 vs 366.33±30.03, p<0.05 respectively). Sensory block regression took longer time in group F as compared with group B (192.83±13.18 vs 177.83±17.20, p<0.05 respectively). Motor block peak in Group F was faster than group B (18.07±1.72 vs 20.73±2.24, p <0.05 respectively). Motor block regression took longer in group F as compared with Group B (149.00±11.85 vs 141.83±11.78, p<0.05 respectively).
Time for rescue analgesia was delayed in group F as compared with Group B (512.43±30.92 vs 339.31±29.31, p<0.001)([Table 2]).
| Group | B | F | P value |
| Sensory onset time (sec) | 107.33±13.50 | 111.67±14.46 | 0.235 |
| Motor onset time(sec) | 446.00±56.97 | 438.00±47.30 | 0.556 |
| Sensory block peak(sec) | 333.67±42.71 | 366.33±30.03 | 0.001 |
| Motor block peak(min) | 20.73±2.24 | 18.07±1.72 | < 0.001* |
| Duration of sensory block(min) | 177.83±17.20 | 192.83±13.18 | <0.001* |
| Duration of motor block(min) | 141.83±11.78 | 149.00±11.85 | 0.022* |
| Time for first analgesic (min) | 339.31±29.31 | 512.43±30.92 | <0.001 |

Motor block onset was comparable in both Group B and Group F(p>0.05). Motor block peak in Group F was faster than group B (p<0.05). Motor block regression took longer in group F as compared with Group B (p<0.05). Sensory block onset was comparable in both the groups (p>0.05) Sensory block peak in Group B was faster than group F, p<0.05. ([Figure 2]).
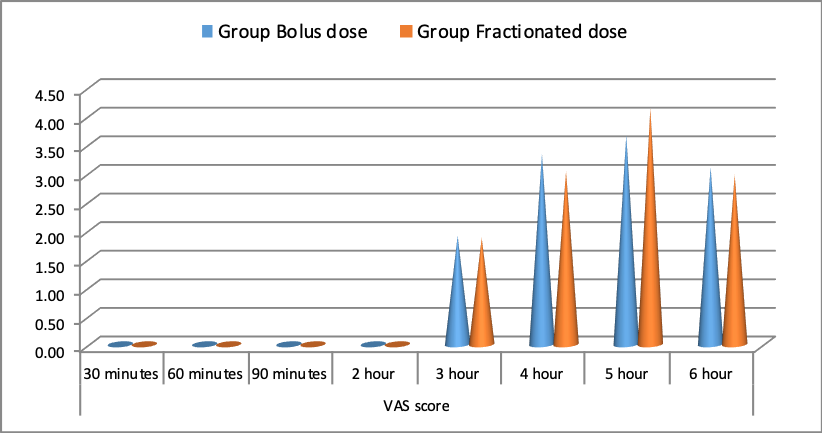
VAS score significantly higher in Group F as compared with Group B at 5 hour interval (4.13±0.78 vs 3.67±0.88, p<0.05) ([Figure 3]).
Vasopressor was used significantly more frequently in Group B as compared with Group F (p<0.05). Atropine was used significantly more frequently in Group B as compared with Group F (p<0.05) ([Table 3]).
| Group B | Group F | p value | |
| Vasopressor | 10 | 5 | 0.045* |
| Atropine | 8 | 3 | 0.034* |
No significant difference was noted in distribution of nausea/ vomiting, shivering, pruritus and respiratory distress between Bolus dose and Fractionated dose groups(p>0.05) ([Table 4])
| Group B | Group F | P value | |
| Nausea/vomiting | 3 | 1 | 0.301 |
| Hypotension | 0 | 0 | 0.00 |
| Pruritus | 2 | 0 | 0.150 |
| Shivering | 4 | 1 | 0.161 |
Discussion
Spinal anaesthesia is routinely employed anaesthetic procedure in patients undergoing lower-limb surgeries.[1], [2], [3] It is preferred due to its rapid time of onset, it being efficacious, having very little effect on mental-status and decreased blood-loss as compared with general anaesthesia, its action to protect patients against thromboembolic sequelae make it a preferred choice of anaesthesia for patients undergoing lower limb surgery. [4] However, danger of serious and prolonged hypotension is related with spinal anaesthesia. This is because of the quick sympathetic blockade, upsetting cardiovascular adaptation and causing morbidity and mortality.[5], [6]
Our study aimed to compare fractionated dose versus bolus dose of spinal anaesthesia for haemodynamic stability; as well as and duration of sensory and motor block.
It was indicated by Schnider et al.[11] that time of onset to reach an acceptable sensory-level for for surgical procedure is directly proportional to height and inversely proportional with weight. Our study enrolled adult ASA I or II subjects with BMI 18.5-22.9 kg/m2.
In the study by Badheka et al,[7] bbolus group was administered a mean dosage of 2.14 (2–2.4) ml while the fractionated group was administered a mean dosage of 2.2 (2–2.6) ml which were comparable among the two groups. The dosages were comparable to the fixed dose used in the study done by Harten et al.[12]
Danelli et al.[8] used 0.5% hyperbaric Bupivacaine in a dose of 0.06mg/cm, which was adequate for providing effective spinal block in 95% of women undergoing LSCS.
Jigisha Badheka[7] used a dose of 0.07mg/cm, 0.5% Bupivacaine in her study to compare the effect of fractionated dose versus bolus dose of LA in spinal anaesthesia for LSCS. For fractionated dose, they administered initial two third dose then after 90 sec time gap, the remaining one third dose was administered.
We used 3ml (15mg) 0.5% hyperbaric Bupivacaine for spinal anaesthesia for patients undergoing lower limb surgeries.
In our study, baseline haemodynamic parameters comparable among the two groups (p>0.05)
Compared to fractionated group, bolus group patients had lower MAP post spinal, 2, 4, 6, 8, 10, 16, 22, 25, 28, 33, 25, 28, 30, 35, 40, 45, 50, 60 minutes(P<0.05). However, it was comparable at 13, 19, 55 minutes (P>0.05). This was in agreement with Badheka et al,[7] where fractionated dose of spinal anaesthesia provided more haemodynamic stability as compared with bolus dose in patients undergoing elective caesarean section. It was also in agreement to the study by Favarel Garrigues, et al[13] who compared the hemodynamic changes between Continuous Spinal Anaesthesia (CSA)and single-dose SA (SDSA) on 60 elderly patients older than 70years who underwent hip surgeries and concluded that there was more decrease in mean arterial blood pressure in SDSA than CSA.
Pitkanen et al,[14] in contrast, compared hemodynamic changes between CSA and single-dose SA with plain bupivacaine on 40 elderly patients scheduled for hip or knee surgeries and found that CSA and single-dose SA were quite similar regarding hemodynamic stability.
A steady-onset of segmental-block can explain the steady-progression and reduced haemodynamic changes within CS group. This makes it easier to adapt the cardiovascular system than when the sympathectomy occurs suddenly, like in SDSA. The slow-onset of blockade has been observed in earlier papers using other CSA regimens[15], [16] whereas with SDSA, a quick fall in Blood Pressure is commonly noted.
In contrast to our study, Nugroho AM et al,[17] comparison of Fractionated and Single Dose Injection of Spinal anaesthesia for Cesarean Section patients with Pregnancy Induced Hypertension was done. They concluded that MAP was not significantly different the two groups. Total vasopressor used and level of sensory blockade were not significantly different.
In our study, sensory block onset was comparable between both bolus and fractionated groups. Sensory block peak in bolus group was faster than fractionated group (333.67±42.71366.33±30.03, p<0.05 respectively). Sensory block was regression took longer time in the fractionated group as compared with bolus group (192.83±13.18 vs 177.83±17.20, p<0.05 respectively).
In the study done by Badheka et al, [7] in contrast with our study, the onset of sensory block was comparable between two groups. As with our study, the duration of sensory block was statistically significant among the two groups (161±29 min in Bolus group and 236±42 min in Fractionated group, respectively, P < 0.05)
Similar to our study, Khare et al,[18] concluded that the duration of the sensory block was longer in fractionated group as compared with Bolus group (235 ± 42 min vs 160 ± 29 min, p<0.05).
In our study, motor block onset was comparable between both bolus and fractionated groups (p>0.05). Motor block peak (in seconds) in the fractionated group was faster than the bolus group (18.07±1.72 vs 20.73±2.24, p<0.05 respectively). Motor block regression (in minutes) took longer in fractionated group as compared with bolus group (149.00±11.85 vs 141.83±11.78, p<0.05 respectively).
This was similar to Badheka et al,[7] where onset of motor blockade was comparable between two groups while duration motor regression was statistically significant among the two groups (145±25 in Bolus group and 204±42 in Fractionated group respectively, p < 0.05)
Our results were also similar to Khare et al,[18] the duration of the motor block was longer in fractionated group as compared with bolus group (203 ± 42 vs 144 ± 25, p<0.05).
Our results were similar to Fahmy [19] in his study 1996 concluded that fractionated dose of spinal Bupivacaine is associated with a longer duration of sensory motor blockade and lesser fall in BP. These results were similar to our study.
The mean VAS score at 5 hours was significantly higher among Fractionated dose compared to bolus dose. This was in contrast with the study by Khare et al [18] where in the analgesic duration were longer in fractionated group as compared with Bolus group.
Vasopressor was used significantly more frequently for bolus dose group (33.3%)as compared with fractionated dose group(16.7%)(Chi-square value = 3.784, p<0.05). This was similar to Badheka et al[7] where vasopressor used was significantly more among Bolus dose group compared to Fractionated dose group.
Our results were in agreement with the study by Favarel Garrigues et al[13] where dosage of ephedrine was found to be less in the CSA group which was significant as compared with Singe Dose Spinal Anaesthesia.
Our results were also similar to Abdel Kader et al[20] nearly 75% of SA patients required ephedrine (3 mg to >30 mg) to maintain pressure; no patients in the CSA group required ephedrine and only three patients in the SFA group received ephedrine. Bharadwaj et al[21] compared three vasopressors- Phenylephrine, Ephidrine and Metaramiol for keeping tight control on maternal blood pressure in elective caesarean sections under spinal anaesthesia. They concluded that all three were similarly effective. We used Mephentermine as the vasopressor in our study for treating Hypotension.
In current study, Atropine was used significantly more frequently for Bolus dose group(26.7%) as compared with Fractionated dose group(10.0%)(Chi-square value = 4.089, p-value = 0.034). Badheka et al[7] and Khare et al [18] had no incidence of bradycardia in both the groups.
Bradycardia is a known prominent serious side effect of Spinal Anaesthesia, with the incident of bradycardia ranging from 30% to 40%; often requiring atropine, 10 mcg / kg IV bolus.[22], [23]
We noted no significant difference in distribution of nausea/vomiting, shivering, pruritus and respiratory distress between Bolus dose and Fractionated dose groups(p>0.05).
Conclusion
Fractionated dose of 0.5% Hyperbaric Bupivacaine in spinal anaesthesia provides greater haemodynamic stability in terms of less fall in heart rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure while also providing longer duration of sensory and motor block as compared with bolus dose in adult patients undergoing lower limb surgeries. Fractionated dose of Intrathecal Bupivacaine can be an acceptable and safe alternative in patients undergoing lower limb surgeries.
Limitation of the Study
Our study consisted of 60 patients. Further studies and research on a larger population comparing bolus and fractionated dose of spinal anaesthesia can be done to evaluate the effectiveness of fractionated dose in maintaining haemodynamic stability.
Source of Funding
Nil.
Conflicts of Interest
There are no conflicts of interest
References
- R J Buist. A Survey of the Practice of Regional Anaesthesia. J R Soc Med 1990. [Google Scholar]
- Sergi Sabaté, Carmen Gomar, Jordi Huguet, Jorge Castillo, Jaume Canet, Antonio Villalonga. Anesthesia for urological surgery in a European region with 6.7 million inhabitants (Catalonia, Spain). J Clin Anesth 2009. [Google Scholar]
- A. Rodgers. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised. BMJ 2000. [Google Scholar]
- P.-A. Sutter, Z. Gamulin, A. Forster. Comparison of continuous spinal and continuous epidural anaesthesia for lower limb surgery in elderly patients A retrospective study. Anaesthesia 1989. [Google Scholar]
- Caroline R. Covert, Gordon S. Fox. Anaesthesia for hip surgery in the elderly. Can J Anaesth 1989. [Google Scholar]
- Vincent W. S. Chan, Frances Chung, Manuel Gomez, Chanth Seyone, Godofredo Baylon. Anesthetic and hemodynamic effects of single bolus versus incremental titration of hyperbaric spinal lidocaine through microcatheter. Anesth Analg 1994. [Google Scholar]
- JigishaPrahaladray Badheka, VrindaPravinbhai Oza, Ashutosh Vyas, Deepika Baria, Poonam Nehra, Thomas Babu. Comparison of fractionated dose versus bolus dose injection in spinal anaesthesia for patients undergoing elective caesarean section: A randomised, double-blind study. Indian J Anaesth 2017. [Google Scholar]
- G Danelli, A Zangrillo, D Nucera, Giorgi E Fanelli, G Senatore, R. The minimum effective dose of 0.5% hyperbaric spinal bupivacaine for cesarean section. Minerva Anestesiol 2001. [Google Scholar]
- D L Brown. . Spinal, epidural, and caudal anesthesia. Miller’s Anesthesia. 7th ed 2009. [Google Scholar]
- H J Harder. Unilateral lumbar spinal anesthesia with hyperbaric solutions. Anaesth 1959. [Google Scholar]
- Thomas W. Schnider, Charles F. Minto, Heini Bruckert, Jaap W. Mandema. Population Pharmacodynamic Modeling and Covariate Detection for Central Neural Blockade. Anesthesiol 1996. [Google Scholar]
- J. M. Harten, I. Boyne, P. Hannah, D. Varveris, A. Brown. Effects of a height and weight adjusted dose of local anaesthetic for spinal anaesthesia for elective Caesarean section. Anaesth 2005. [Google Scholar]
- J F Favarel-Garrigues, F Sztark, M E Petitjean, M Thicoipe, P Lassie, P Dabadie. Hemodynamic effects of spinal anesthesia in the elderly: single dose versus titration through a catheter. Anesth Analg 1996. [Google Scholar]
- M. Pitkänen, P. Rosenberg, M. Silvanto, M. Tuominen. Haemodynamic changes during spinal anaesthesia with slow continuous infusion or single dose of plain bupivacaine. Acta Anaesthesiol Scand 1992. [Google Scholar]
- A Sabaté, R Asbert, T Gracia, I Camprubi, R Sopena, E Udina. Regional anesthesia and elderly patients: continuous subarachnoid anesthesia versus single dose in peripheral vascular surgery. Reg Anesth Pain Med 1994. [Google Scholar]
- W Klimscha, C Weinstabl, W Ilias, N Mayer, A Kashanipour, B Schneider. Continuous spinal anesthesia with a microcatheter and low-dose bupivacaine decreases the hemodynamic effects of centroneuraxis blocks in elderly patients. Anesth Analg 1993. [Google Scholar]
- Alfan Mahdi Nugroho, Adhrie Sugiarto, Susilo Chandra, Laras Lembahmanah, Rafidya Indah Septica, Annisaa Yuneva. A Comparative Study of Fractionated Versus Single Dose Injection for Spinal Anesthesia During Cesarean Section in Patients with Pregnancy-Induced Hypertension. Anesth Pain Med 2019. [Google Scholar]
- D Khare, N Nema. Comparison of bolus dose versus fractionated dose of injection bupivacaine heavy (0.5%) in spinal anaesthesia for patients undergoing emergency caesarean section: a randomised study. Anesthesiol 2019. [Google Scholar]
- N R Fahmy. Circulatory and anaesthetic effects of bupivacaine for spinal anaesthesia fractionated vs. bolus administration. Anaesthesiol 1996. [Google Scholar]
- AliaaM.A.R Abdel Kader, KamalE Ali Hekal, YaserM Amr Ragheb, AmrA Magdy. Single-shot spinal anesthesia with heavy bupivacaine in two regimens versus continuous spinal anesthesia in elderly patients undergoing hip surgery: a prospective randomized controlled study. Tanta Med J 2018. [Google Scholar]
- Neerja Bhardwaj, Kajal Jain, Suman Arora, Neerja Bharti. A comparison of three vasopressors for tight control of maternal blood pressure during cesarean section under spinal anesthesia: Effect on maternal and fetal outcome. J Anaesthesiol Clin Pharmacol 2013. [Google Scholar]
- V W Whizar-Lugo, I A Gómez, R Cisneros-Corral, N Martínez-Gallegos. Intravenous dexmedetomidine vs. intravenous clonidine to prolong bupivacaine spinal anesthesia. A double blind study. Anestesia en Mexico 2007. [Google Scholar]
- K Elcicek, M Tekin, Kati I. The effects of intravenous dexmedetomidine on spinal hyperbaric ropivacaine anesthesia. Anesth 2010. [Google Scholar]
How to Cite This Article
Vancouver
Srivastava N, Ahluwalia P, Jheetay GS, Singh G. Bolus dose versus fractionated dose injection of hyperbaric bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgery: A prospective study [Internet]. Indian J Clin Anaesth. 2025 [cited 2025 Sep 07];7(2):238-244. Available from: https://doi.org/10.18231/j.ijca.2020.043
APA
Srivastava, N., Ahluwalia, P., Jheetay, G. S., Singh, G. (2025). Bolus dose versus fractionated dose injection of hyperbaric bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgery: A prospective study. Indian J Clin Anaesth, 7(2), 238-244. https://doi.org/10.18231/j.ijca.2020.043
MLA
Srivastava, Nakul, Ahluwalia, Pallavi, Jheetay, G S, Singh, Gurpartap. "Bolus dose versus fractionated dose injection of hyperbaric bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgery: A prospective study." Indian J Clin Anaesth, vol. 7, no. 2, 2025, pp. 238-244. https://doi.org/10.18231/j.ijca.2020.043
Chicago
Srivastava, N., Ahluwalia, P., Jheetay, G. S., Singh, G.. "Bolus dose versus fractionated dose injection of hyperbaric bupivacaine in spinal anaesthesia among adult patients undergoing lower limb surgery: A prospective study." Indian J Clin Anaesth 7, no. 2 (2025): 238-244. https://doi.org/10.18231/j.ijca.2020.043
