Introduction
Pharyngeal mass often presents to the anaesthesiologist for airway management and anaesthesia, needed to aid in diagnosis or treatment. These patients present a challenge to the anaesthesiologist as they block the pathway for ventilation as well as intubation. Spindle cell carcinomas are rare tumors with very few cases of oropharyngeal spindle cell carcinomas reported. These tumors of the pharynx usually present as pedunculated masses of less than 2 cm in size. The anesthetic management for excision is usually simple. We report a unique case of a large size 5 cm pedunculated oropharyngeal mass, which was mobile causing dynamic airway obstruction. A meticulous pre-operative examination and planning for the airway management lead to anticipation of difficulties and easy navigation through them.
Case Report
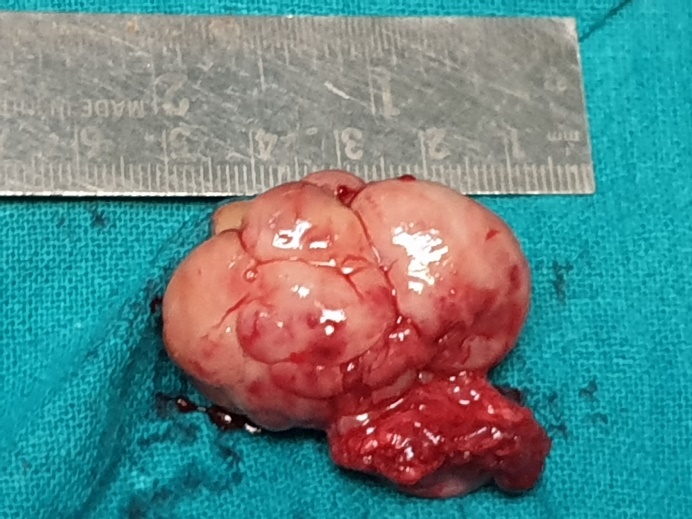
A 68-year-old female presented to the pre-anaesthetic clinic for excision of an oropharyngeal mass. She had a history of difficulty in swallowing solids for the past six months, which had progressed to difficulty in swallowing liquids in the past three months. She also complained of difficulty in breathing in the supine position, for the past three months. This had progressively increased to difficulty in breathing in the standing position. Tongue protrusion leads to the mass moving further forward and relief in dyspnea as per the patient. On examination, the patient's MMPC was 1. A s the mouth was opened and tongue protruded, the mass visibly moved into the oral cavity. This was because the mass obstructed the flow of air from the nasopharynx as well as the oral cavity, and tongue protrusion led to movement of the mass forward and created a passage for airflow. The CT scans (Figure 1) showed a pedunculated well-defined 4*4*5 cm mass, arising from the oropharynx and falling into the hypopharynx. General Physical Examination and Laboratory investigations were within normal limits.
Excision of the mass was planned under general anaesthesia. Informed written consent was obtained, which included consent for emergency tracheostomy.
On the day of surgery, intravenous access was secured, intramuscular Glycopyrrolate 0.2 mg was given. The patient was nebulized with 5 ml of 4% Lignocaine. Xylometazoline nasal drops were instilled twice. The patient was shifted to the operation theatre and standard monitors attached. Superior and recurrent laryngeal nerve blocks then given. The patient was given intravenous Midazolam 1 mg and a bolus dose of intravenous Dexmetomidine (0.5 mcg/kg). An infusion of Dexmedetomidine was titrated to a Ramsay Sedation Score of 3. Para oxygenation using a nasal cannula was continued at all times.
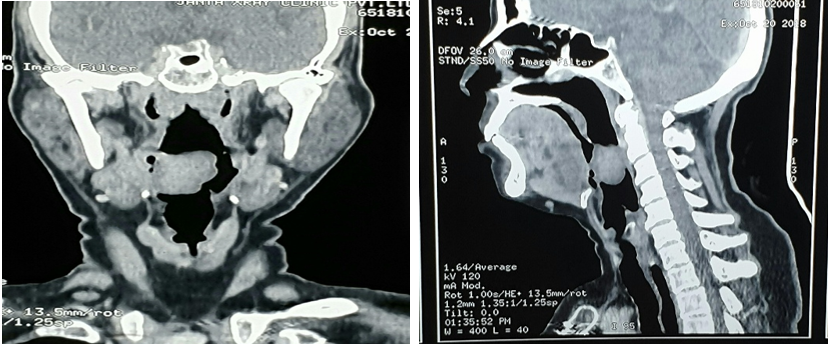
The fiberoptic scope was inserted nasally, the path was easily visualized till the oropharynx, after that the path was obstructed by the mass. The patient was asked to open her mouth and protrude her tongue, this leads to the mass moving forward. We were able to negotiate beyond the mass and on visualizing the carina, a # 6.5 Endotracheal tube was inserted. During tube insertion, on encountering resistance, the patient was asked to protrude her tongue again, the tube was withdrawn 2 cm, rotated by 90 and advanced successfully. After confirming intubation, the patient was paralyzed and sedated. The mass was excised (Figure 2) and found to be arising from the tonsillar fossa and on pathology found to be spindle cell carcinoma. The patient was extubated uneventfully at the end of the procedure.
Figure 1
The CT Scans of the patient shows a mass overhanging the glottic opening, attached precariously by a stalk
Discussion
Spindle cell carcinoma is a rare entity. It is more predominant in males (7:1 ratio).1 Smoking, alcohol consumption and previous irradiation are predisposing factors.3, 2 The most common site of origin is the glottic region (70%), presenting with hoarseness, dyspnea, and cough. They are usually less than 2 cm in size,4 with wide local excision being the treatment of choice.
Airway management in the case of oropharyngeal tumors is a challenge. Sedation and anaesthesia can cause a loss in muscle tone, leading to a collapse of the mass and soft tissue of the airway. This can lead to complete obstruction of the air passage. We expected difficult mask ventilation as a result of the above. Direct Laryngoscopy was expected to be difficult because of the history given by the patient and the CT scan report showing the mass almost obstructing the laryngeal and hypopharyngeal space. As seen in Image 1 and 2 the mass appears to be obstructing the hypopharyngeal space and is attached only by the stalk to the oropharyngeal space. Awake fiberoptic intubation7, 6, 5 is a gold standard in the management of the difficult airway. However, it needs the expertise to be able to manage the airway in cases where trauma may lead to bleeding which would cause difficulty in visualization. Also, injury to the stalk could potentially lead to dislodgement of the mass and complete airway obstruction. The nasal route was chosen so that in case of difficulty in visualizing the larynx, mouth opening and tongue protrusion would be possible. This would potentially lead to the movement of the mass away from the pathway (based on the preoperative examination). Sedation would lead to better toleration of the procedure and less movement. Tracheostomy was planned as a last resort, in case of a CVCI situation.
Management of this case shows the importance of a proper pre operative examination in preventing peri operative airway related morbities. Emphasis on planning the airway management and a proper plan A and B lead to successful airway management without any complications or discomfort to the patient.
Management of the airway in a case of oropharyngeal mass requires skill and preoperative planning to prevent a CVCI situation from arising. All modalities including a CT Scan of the airway may be used in planning the management of such cases. A clear Plan A and B and Emergency plan should be in place with equipment prepared. Awake fibreoptic intubation while being a gold standard should be a part of the management, not the only management.
Conclusion
The patient was a case of oropharyngeal mass which was almost completely obstructing the hypopharynx, leading to dyspnea. The patient gave a history of relief in dyspnea on protruding the tongue, we corroborated the forward movement of the mass on tongue protrusion during the airway examination. As our hypopharyngeal cavity was almost completely blocked we expected a difficult bag and mask ventilation especially after muscle and soft tissue relaxation under anaesthesia. We had therefore planned for awake nasal fiberoptic intubation as our plan A, with tracheostomy planned as Plan B, in case we were unsuccessful in manipulating the fiberoptic scope or endotracheal tube through the patient's airway. During the procedure we were unable to view the passage beyond the base of the tongue, as the passage was blocked by the mass, at this point we asked the patient to protrude her tongue as we had preplanned. This lead to movement of the mass away from the pharyngeal wall, and visualization of the passage beyond the mass. We were able to successfully navigate the scope and view the carina. During tube insertion, on encountering resistance, the patient was asked to protrude her tongue again, the tube was withdrawn 2 cm, rotated by 90 and advanced successfully. This case emphasis the importance of a good history and examination, as we would have been unable to perform the intubation, if the fact that mouth opening and tongue protrusion lead to relief in dyspnea and the mas moving forward was not noticed.