Introduction
Diagnostic and therapeutic knee arthroscopies are common procedures that can be performed under general, regional or local anaesthesia. Effective post-operative pain relief with minimum associated side effects is important to permit early mobilization after surgery and to improve the patient’s comfort, mobility and rehabilitation.
Intra-articular administration of local anaesthetic is an ideal method of providing better analgesia after knee arthroscopy to reduce consumption and possible side effects of oral and intravenous anaesthetics. Various drugs have been used for this purpose including local anaesthetics, opioids, NSAIDS etc.1
Among the local anaesthetics Bupivacaine has proved useful and effective, however its cardio-toxicity as well as with the advent of newer safer drugs like Ropivacaine, it is slowly being replaced.2
Ropivacaine is an amino amide local anaesthetic. It has similar duration of action but lesser systemic toxicity as compared to Bupivacaine so larger doses of it can be administered. It also has an inherent local vasoconstrictor effect which may help prolong its duration of action locally. All these characteristics make it a more suitable local anaesthetic for intra-articular injection as compared with Bupivacaine.3
Common combinations of local anaesthetics with drugs like Morphine, Ketorolac, etc. have been tried with good results due to the additive or synergistic effects and concomitant reduction of side effects because of lower doses used. Morphine is a potent, cheap opioid which can bring about analgesia by acting on peripheral opioid receptors. The side effects of morphine such as pruritus, respiratory depression and urinary retention can be avoided by giving it intra-articular.7, 6, 5, 4
Materials and Methods
Source of data
The study was undertaken on 60 consenting adult in-patients of Father Muller Medical College Hospital scheduled for elective knee arthroscopy, under general anaesthesia.
Inclusion criteria
Adult patients of ASA I and II physical status of either sex between the ages of 18 to 70 years of weight 40 to 65 kg posted for elective knee arthroscopy.
Exclusion criteria
Patients of ASA physical status III and IV
Patients with cardio-respiratory diseases, coagulopathy, raised intracranial tension.
History of sensitivity to local anaesthetics, morphine.
Following approval of institutional ethical committee, 60 consenting adult patients fulfilling the inclusion criteria were selected for the study.
All patients were kept nil per oral for 6 hours and were pre-medicated with Tab. Ranitidine 150mg, Tab. Diazepam 5mg orally 12 hours before surgery. Patients were taught the visual analogue pain score (VAS) (0 = no pain, 10 = worst imaginable pain), and VAS was measured pre-operatively at rest and on movement of the knee to be operated.
Patients were divided into 2 groups of 30 each, based on random numbers.
Table 1
| Group | Pretreatment Given | Number or Patients |
| R | Intra-articular Ropivacaine 150mg in 20ml | n= 30 |
| RM | Intra-articular Ropivacaine150mg + 4mg morphine in 20ml. | n= 30 |
The arthroscopies were performed by two orthopaedic surgeons. Surgery was performed using a standard 2-portal technique with a tourniquet inflated to 350mm of Hg.
All patients received standard general anaesthesia. Patients will be pre-oxygenated and will be induced intravenously with Inj. Fentanyl 1microg/kg, Inj. Propofol 2mg/kg, paralysed with Inj. Vecuronium 0.1mg/kg as loading dose, intubated with an appropriate sized cuffed endotracheal tube. Maintenance dose of Inj. Vecuronium 0.02mg/kg was administered when required with nitrous oxide 66% and oxygen 33%. Allocated drug was injected by the surgeon through the ports after closure of the ports with a suture for each portal five minutes before tourniquet release.8 Local Anaesthetic was infiltrated subcutaneously at the site of the suture.2 At the end of the surgery, neuromuscular blockade will be reversed by Inj. Neostigmine 0.05mg/kg and Inj. Glycopyrrolate 0.02mg/kg intravenously
Postoperatively, the heart rate, blood pressure, allergic reactions, nausea and headache were monitored for the first six hours. Visual Analogue Score (VAS) for pain scores in neutral position and were recorded at hourly intervals for the first eight hours, 2 hourly for the next eight hours and hourly for the final 24 hours.
Patients were given rescue medication on demand. The initial rescue medication was Inj. Diclofenac 75mg intramuscularly. In the event of insufficient analgesia Inj.Butorphanol 1 mg intravenously was given. The time for the first request for analgesia and total analgesic requirement were recorded.
Statistical analysis
Descriptive statistical analysis has been carried out in this particular study.
Repeated measures ANOVA were performed to study the significance of parameters studied. Strongly significant (P value <0.001)
The statistical software SPSS 15.0 was used for analysis of data. Microsoft Word and Excel were used to generate graphs, tables, etc.
Results
The two Groups were comparable in terms of age, sex and weight
In Group R 15 patients (50%) on the patients opted for rescue medications within six hours of surgery and 15 (50%) of patients opted for rescue medications after six hours of surgery, whereas in group RM only 3 patients (10%) opted for rescue medications after six hours of surgery and 27 (90%) opted for rescue medications six hours after surgery. (P-value<.001)
Figure 3
Bar chart representing the time and frequency of patients who opted for rescue medication in the two treatment groups
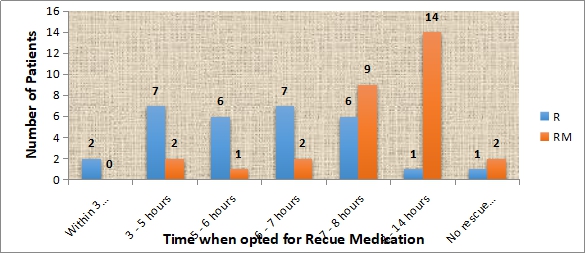
In the First 3 hours 2 patients in Group R and no patients in Group RM opted for rescue medications.
At 3 – 5 hours 7 patients in Group R and 2 patients in Group RM opted for rescue medications.
At 5-6 hours 6 patients in Group R and 1 patient in Group RM opted for rescue medications.
At 6-7 hours 7 patients in Group R and 2 patients in Group RM opted for rescue medications
At six hours 22 patients in Group R and 5 patients in Group RM opted for rescue medications.
Discussion
Effective pain relief is important after diagnostic and therapeutic arthroscopic knee surgery to permit early discharge and improve comfort and mobility at home.5 The ideal analgesic agent would require to be associated with least side effects and with a suitably long duration of action.8
Moiniche S, Mikkelsen S, Wetterslev J, Dahl J. B in 19991 in their systematic review of Local Anaesthesia for postoperative pain relief after arthroscopic surgery have demonstrated that the intra-articular administration of local anaesthetics have been shown to provide superior post-operative analgesia as compared to a placebo. Ropivacaine is a newer local anaesthetic with a better safety profile, long duration of action, and relative motor sparing effect. Convery PN, Milligan KR, Quinn P, Sjövall J, Gustafsson U in 2001,2 Huey Ping et al in 2006,5 Vintar N, Rawal N, Veselko M in 2005,9 Franceschi F, Rizzello G, Cataldo R, Denaro V in 200110 have successfully utilized Ropivacaine intra-articular for relief of pain.
The goal of this study was to compare the post-operative pain relief after knee arthroscopy using intra articular Ropivacaine 20ml of a 0.75% solution (150mg) made up to 21 ml with sterile water as compared to Ropivacaine (150mg) with morphine (4mg) 20ml of 0.75% Ropivacaine and 4mg of Morphine made up to a volume of 21ml. The dose of 150mg Ropivacaine was decided upon in accordance with the findings of Convery PN, Milligan KR, Quinn P, Sjövall J, Gustafsson U et al2 who concluded that Ropivacaine at a higher dose of 150mg reduces post-operative pain more effectively as compared to the lower dose of 100mg. A dose of 4mg of Morphine was decided upon in accordance with the findings of Likar R, Kapral S, Steinkellner H, Stein C, Schäfer M.7
A Total of 60 consenting patients scheduled for elective or emergency arthroscopy under general anaesthesia fulfilling the inclusion criteria were selected for the study. Majority of the studies chose general anaesthesia as the management of choice for intraoperative anaesthesia, with the exception of Vintar N, Rawal N, Veselko M in 20039 who chose subarachnoid blockade and Raja SN, Dickstein RE and Johnson CA in 199211 who chose epidural anesthesia and Heard S. O et al in 199212 who chose patients irrespective of the anaesthetic technique. In our study we chose general anaesthesia over regional anaesthesia as the residual effect of the regional anaesthetic would confound our immediate postoperative pain scores.
Our patients were randomly allocated into two groups Group R receiving only 150mg Ropivacaine and Group RM receiving 150mg Ropivacaine and 4mg Morphine at the end of the surgery through one of the operative ports after closure of the ports five minutes before tourniquet release in accordance with Whitford A, Healy M, Joshi GP, McCarroll SM, O'Brien TM in 19978 demonstrated that intra-articular bupivacaine administered at the conclusion of arthroscopic knee surgery significantly reduced postoperative pain and prolonged the time to first analgesic use when compared with placebo. In our study a placebo was not used but Ropivacaine was used as a control to which the combination of Ropivacaine and morphine was compared.
Prior to the surgery at the time of pre-anaesthetic round the patients were taught VAS scoring ( Convery PN, Milligan KR, Quinn P, Sjövall J, Gustafsson U2). The VAS scores were then recorded at hourly intervals for the first eight hours, 2 hourly for the next eight hours and hourly for the final 24 hours. Patients were given rescue medication on demand. Initial medication will be Inj. Diclofenac 75mg, intramuscularly. In the event of insufficient analgesia Inj. Butorphanol 1mg intravenously was be given. The time for the first request for analgesia and total analgesic requirement were recorded.
In the present study majority of the patients were in the age group of 18-70 years. The demographic data was comparable to the literature. The two groups R and RM were comparable in terms of age, sex and weight.
The Mean VAS score In Group R was 5.189 and in group RM was 3.815. The Mean VAS score at Sixth hour after surgery in Group R was 6.53 and in Group RM was 4.778 which was similar to the findings of Huey Ping et al6 where the VAS scores were <3 up to 8 hours postoperatively, however they used Ropivacaine alone and compared it to bupivacaine. Rasmussen S, Allan S. Larsen A, Søren T. Thomsen and Henrik K also found that VAS scores were significantly lower in their Bupivacaine Morphine and Ketorolac combination group as compared to their bupivacaine group.
In Group R 15 patients (50%) on the patients opted for rescue medications within six hours of surgery and 15 (50%) of patients opted for rescue medications after six hours of surgery, whereas in group RM only 3 patients (10%) opted for rescue medications after six hours of surgery and 27 (90%) opted for rescue medications six hours after surgery. (P-value<.001). This proves that the combination of local anesthetic and opioid provide better analgesia as compared to the analgesia obtained on instilling local anesthetic alone. This was similar to the findings of Huey Ping et al6 who found that the group receiving multimodal analgesia intra- articularly in their study consumed less analgesics in the first 24 hours after surgery as compared to the groups having only a local anesthetic injected intra-articular.
None of the patients in our study showed any adverse effects like nausea, vomiting, pruritus. Constipation or circumoral tingling.
Conclusion
The combination of Ropivacaine and morphine provides better analgesia post knee arthroscopy as compared to Ropivacaine alone.
Multimodal analgesia is effective in reducing postoperative pain by synergistic and additive effect between various analgesics. Hence the combination of local anaesthetic Ropivacaine and the opioid Morphine instilled intra-articular provides a good analgesic regimen for patients following knee arthroscopy for the first 24 hours.
Acknowledgements
It gives me great pleasure in preparing this dissertation and I take this opportunity to thank everyone who has made this possible.
At the outset, I would like to thank the Almighty God for his blessings in making this work possible and whose grace has strengthened me throughout.
I would like to thank Dr. Jacob Chacko, Dr. Prashanth, Dr. Vivian from the Department of Orthopedics for encouraging their patients to enrol into this study.
I am thankful to all my staff members, postgraduate students and anaesthesia technicians who helped me during this study.
I am indeed indebted to my parents, for their unfailing love and prayers that has been my inspiration.
I am also thankful to the post operative anaesthesia care unit nurses and staff for their cooperation and support.
I am truly grateful to all the patients who were a part of this study. It is their contribution that has made this study a success.


