Introduction
Ultrasound guidance for rectus sheath block is associated with higher success rate, shorter onset times, reduced total anesthetic doses and reduced complications. Early mobility is the major advantage. Excellent analgesia combined with no motor block of limbs and no mandatory connection to infusion devices allowing the patients to mobilize early with clinical benefits of reduced deep vein thrombosis, pulmonary embolus, reduced atelectasis and respiratory infection especially in obese patients. It was first described by Schleich in 1899. Earlier it was used for relaxation of abdominal wall muscles before the adjunct of neuromuscular blocking drugs.1 However now it is used to provide analgesia after umbilical or incisional hernia repair extended midline incision used in laparotomy and other abdominal surgeries associated with severe postoperative pain associated with neuroendocrine stress response which is undesirable in patients with cardiac conditions. The increased work of breathing coupled with shallow breathing following this incision is another major problem of those having compromised pulmonary functions.2
The aim of this technique is to block the terminal branches of the 9th, 10th and 11th intercostal nerves which run in between the internal oblique and transversus abdominis muscles.3 Transversus Abdominis Plane block is useful mainly for providing analgesia below umbilicus while rectus sheath block provides analgesia to midline and paramedian incisions both above and below umbilicus but does not provide analgesia for lateral side of abdomen. The advent of ultrasound guidance has helped to increase the feasibility and clinical application allowing easier identification of the target anatomical structures and accurate visualization of the needle and Local Anaesthetic spread and thus refining the rectus sheath block.11, 10, 9, 8, 7, 6, 5, 4
Aims and Objectives of Study
Aim of the study is to evaluate and compare the analgesic efficacy of bupivacaine, levobupivacaine and ropivacaine in ultrasound guided bilateral rectus sheath block in patients undergoing umbilical surgeries
Materials and Methods
After the hospital ethical committee approval 60 patients of (American society of Anaesthesiologists) ASA I and II physical status, aged between 18-65 years with Body mass Index (BMI) between 25-40 kg/m2 scheduled for umbilical hernia under General Anaesthesia (GA) in our hospital were included in this study.
Exclusion criteria were age <18ys, ASA class III, IV and patients with a history of hypertension, diabetes, and liver disease, patients with acute or chronic renal disease, neurosurgical and cardiovascular surgical cases, patients with known psychiatric disorders, patients allergic to local anaesthetics, H/O coagulation disorder and BMI> 40kg/m2
The study was performed between January to June 2019 in LG Hospital, Ahmedabad. All the patients underwent thorough pre-anaesthetic checkup which included history taking, general and physical examination. Investigations were checked and written informed consent was taken from patients. All systems were examined including airway and surface anatomy of the abdomen where blocks to be given. The patients were kept nil per oral as per fasting guidelines.
Patients were randomly divided into three groups of 20 each by computerized generated numbers.
Group L: Rectus sheath block was given with Inj. Levobupivacaine 0.25% 15ml on each side
Group R: Rectus sheath block was given with Inj. Ropivacaine 0.375% 15ml on each side.
Group B: Rectus sheath block was given with Inj. bupivacaine 0.25% 15ml on each side
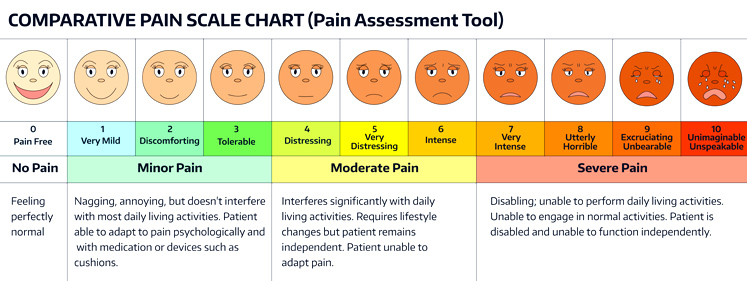
Patients were premedicated with Inj midazolam 0.02mg/kg, Inj glycopyrrolate 0.04 mg /kg and injection fentanyl 2 µg /kg intravenously. They were induced with Injection Propofol 2mg /kg and injection scoline 2mg/kg and endotracheal intubation was done with appropriate sized endotracheal tube. Anaesthesia was maintained with O2, N2 O, Injection Atracurium and sevoflurane. After the completion of surgical procedure and before extubation, modified rectus sheath block was performed with ultrasound high frequency (5-13MHz) linear ultrasound probe (Sonosite Micromax) placed immediately lateral to the umbilicus. A 23 gauge spinal needle was inserted in medial to lateral orientation, through the subcutaneous tissue, to pierce through the anterior rectus sheath. The needle was advanced further through the body of the muscle until the tip rest ed on the posterior rectus sheath. After negative aspiration, 1 to 2 m l of local anesthetic was injected verifying needle tip location. The distribution of the local anesthetic was monitored under real-time imaging. The study drug was deposited according to the assigned groups between the Rectus Abdominis Muscle and the posterior sheath, just before extubation. All the patients were assessed for postoperative pain in the recovery room and in the surgical ward by an anesthesiologist (independent observer) at 1,2,3,4,5,6,8,10,12,14,16 hours after surgery. VAS (0: no pain to 10: worst imaginable pain) (Fig1) was used for pain assessment, for which all patients were instructed before the surgery. No analgesic was given as per the standard protocol. When VAS > 6, rescue analgesic, Injection Diclofenac 75mg IV was given and the time was noted as duration of analgesia.
Statistical analysis
Sample size was taken as 60. Data analysis was performed by using Statistical Package SPSS by Microsoft excel 2010. Data were expressed as mean ± standard deviation. chi square test was used to identify the distribution of variables. Continuous variables was analyzed by ANNOVA. Statistical significance was determined by subject t test. Two tailed p values were used throughout and p value < 0.05 was taken as statistical significant with 1 – ß 80 % sensitivity.
Results
Demographic variables and operative characteristics were similar between the groups. There were no statistically significant differences in age (yrs), sex (M:F), ASA physical status (I:II), BMI (kg/m2) and operative time (minutes) between the L Group, R Group and B group as depicted in Table 1.
The mean time taken for the rectus sheath block procedure was similar in three groups and the difference was not significant. Table 2
The First dose of rescue analgesia (Mean duration of analgesia) was given at 9.30 ± 0.92 hrs in Gp L, 13.02±1.17 hrs in Gp R and 6.2 ± 0.83 hrs in Gp B. The difference was highly significant <0.0001.Table 3
Patients of all three groups showed the VAS above 5. The mean VAS at the time of extubation was 7.25 ± 1.07 in Gp L, 7.32 ± 1.21 in Gp R and 7.18 ± 0.98 in Gp B which was not significant.Table 4
Quality of VAS was highly significant (< 0.0001) in three groups except at 9 hrs (not significant) where mean VAS was 4.14 ± 1.23 in Gp L and 3.6 ± 0.60 in Gp R. At 9 hrs rescue analgesia was already given in Gp B so its VAS was not considered. Table 5, Figure 2
In Gp L 30% of patients were given rescue analgesia at 8 hrs, 10% were given at 9 hrs and the rest 60 % were given rescue analgesia at 10 hrs. In Gp R 50% of the patients were given rescue analgesia at 12 hrs, 10% were given at 13 hrs, 35% were given at 14 hrs and 5% were given rescue analgesia at 16 hrs. In Gp B 25% of patients were given rescue analgesia at 5hrs, 30 % at 6 hrs and 45% patients were given rescue analgesia at 7 hrs, as shown in Table 6.
Table 1
Demographic variables
Table 2
Time taken for the procedure
Table 3
| Group L | Group R | Group B | P value | |
| Duration of analgesia (Hrs) ± sd | 9.30 ± 0.92 | 13.02 ± 1.17 | 6.2 ± 0.83 | < 0.0001 (highly significant) |
Mean duration of analgesia
Table 4
Percentage of VAS Score at the time of Extubation
Table 5
VAS Score mean ± SD
Table 6
Percentages of VAS score postoperatively
Discussion
This study demonstrated that for umbilical hernia repair with BMI 25 -40 mg/m2, ultrasound guided rectus sheath block with general anesthesia provides excellent analgesia as compared to general anesthesia alone. In addition, absence of motor block of the limbs and no mandatory connection to infusion devices or IV poles, allowed patients to mobilize early.
In our study obese patients with BMI >31 kg/m2 were maximally benefited from bilateral rectus sheath block through the opioid sparing effect and these results correlated with study conducted by khaled Abdesalam et al.12
Prior studies have demonstrated efficacy of rectus sheath block with general anesthesia than with general an esthesia alone but none of them have compared analgesic efficacy of different local anaesthetics (Bupivacaine , levobupivacaine and ropivacaine) .
Adding adjuvants to local anesthetic may improve efficacy and duration of the ultrasound guided rectus sheath block and that can be tried in future studies.
The volume and concentration of local anesthetic solution used in ultrasound guided rectus sheath block in our study was 15 ml of 0.25% bupivacaine on each side (30 ml of 0.25% bupivacaine), 15 ml of 0.25% levobupivacaine on each side (30 ml of 0.25%levo bupivacaine)and 15 ml of 0.375% ropivacaine on each side (30 ml of 0.375% ropivacaine) are comparable to those in the literature, e.g., 20 ml 0.25% bupivacaine on each side (40 ml of 0.25% bupivacaine).13 We could get desirable effects with 15 ml each side, total 30ml in our pilot studies and did not exceed the recommended dose.
The USGMRSB is safe and easy technique to provide immediate post-operative analgesia in the patients of umbilical surgeries. We did not come across any complications like rectal sheath hematoma, puncture of posterior rectus sheath, peritoneum and bowel in our study.
Limitation of our study was that we had used only single injection of local anaesthetic in rectus sheath block instead of putting a catheter for providing continuous analgesia. Hence in our study we were able to compare post-operative analgesia up to 12-16 hrs.
Use of ultrasound has increased the success rates of regional techniques. Dolan et al. have shown that ultrasound guidance significantly improves accuracy of RS block versus loss of resistance techniques.5
With the focus on epidural analgesia as part of multidimensional approach of post-operative care; it is essential to have an effectiveopioid sparing technique, especially for patients in whom epidural analgesia is not a viable option. With the current available evidence, RS block is a feasible technique in scenarios that have been reported; that is, in cases where epidural is contraindicated, or has failed or in case of unexpected change in surgical plan. It is probably the need of the hour to formulate and propose an alternate algorithm to epidural analgesia, for effective pain management.
Single injection of Levobupivacaine 0.25% 30ml gives 9.30 ± 0.92 hrs, Bupivacaine 0.25% 30 ml gives 6.2 hrs of analgesia and Ropivacaine 0.375% 30 ml gives analgesia for 13.02 ±1.17 hrs. So, for patients having t runcal obesity and BMI > 25 kg/m2, Ropivacaine is a better choice as it provides longer (14-16) pain free period with lesser incidence of atelactasis, pulmonary embolus, respiratory depression and deep vein thrombosis without early intervention of IV analgesics. Also by this time the critical period of acute post–operative pain is almost over.
The quality of VAS score was highly significant in three groups. On comparison among the three, VAS score didn’t cross 4 until 10 hrs in Gp R where as it crossed at 5 hrs in Gp B and 8 hrs in L Gp, signifying that quality of analgesia is best with ropivacaine. (Table 5 and Figure 2
Ropivacaine, a long acting amide local anaesthetic was introduced as an answer to bupivacaine induced cardio toxicity. It is developed as a pure S (-) enantiomer of propivacaine. It is less lipophilic than bupivacaine so is less likely to penetrate large myelinated motor fibers resulting in a relatively reduced motor blockade. This reduced lipophilicity is also associated with decreased potential for neuro and cardio toxicity. Thus ropivacaine appears to be an important option for regional anaesthesia and for the managem ent of post operative pain.14
Conclusion
We conclude that ultrasound guided modified rectus sheath block is a fairly simple and reliable procedure for patients undergoing umbilical surgeries under general anaesthesia. In our study, the block was performed prior to extubation, thus avoiding patients’ discomfort along with the benefit of immediate post-operative analgesia for 7-16 hours. The study also compared the efficacy of bupivacaine, levobupivacaine and ropivacaine and concluded that excellent analgesia with VAS <4 was provided by ropivacaine for 10 hours postoperatively with a total period of analgesia amounting to 16 hours.