Introduction
Sore throat and hoarseness after general anaesthesia with tracheal intubation are reported to occur in 21% to 65% of patients.1 Coughing after endotracheal extubation are most bothersome clinical problems faced during general anaesthesia. Though a minor complication, any one of these may be troublesome, and can make the patient feeling uncomfortable.2 Various complications such as bronchospasm, surgical site bleeding, myocardial ischemia, arrhythmias, increased intraocular and intracranial pressure are frequently associated.3,4
Contributory mechanisms include trauma to the tonsillar pillars, pharynx, tongue, larynx and trachea,4 drying out of mucosal membrane in the trachea with endotracheal intubation or the upper airway following anaesthesia by mask, involvement of cuff-tracheal surface contact area that have the largest cuff tracheal surface contact upon inflation5,6 infection, type of cuff, cuff pressure and inflating agent of the cuff. Drying effects of anaesthetic gases and anti-sialagogue effects of anticholinergic drugs also play a role.7 A irway related problems like sore throat and others tend to occur in patients who have undergone tracheal intubation.8
There are different methods for prevention of intubation related sore throat. Many pharmacological interventions have been suggested but none have been totally successful.1 Various factors have been evaluated to reduce the rise in cuff pressure such as repeated inflation deflation technique, use of O2 -N2O mixture, polyurethane cuff and liquid cuff media like lignocaine, hydrocortisone, saline. At present there is no effective therapy for the prevention of postoperative sore throat or hoarseness in patients. Still this aspect requires further research for prevention of this problem. There is an ongoing search to prevent these problems. Hence our study was undertaken to assess incidence of sore throat, cough and hoarseness of voice following extubation with intracuff air, saline, 4% lignocaine and hydrocortisone.
Materials and Methods
The present study was conducted in the Department of Anaesthesiology, Basaveshwara medical college hospital and Research centre, Chitradurga. A total of 400 patients, between 18-65 years of age with Mallampati grading I and II, belonging to ASA class I and II, undergoing elective general, orthopaedic, gynaecological, neurosurgical and urological surgeries carried out under general anesthesia were included in the study. Patients with anticipated difficult intubation, laryngeal disease/trauma, Mallampati grading III and IV, allergy to lignocaine, ASA class III and IV were excluded from the study. Ethical committee clearance and informed consent was obtained prior to the commencement of the study. Randomization was done based on the agent used for inflation of cuff, randomization was done using computer generated randomization into four groups namely; Group A – Cuff inflation with air; Group S – Cuff inflation with saline; Group L – Cuff inflation with lignocaine; Group H – Cuff inflation with hydrocortisone.
Age and sex of the patients was recorded and history was taken. After thorough pre-anaesthetic evaluation, patients were allocated by computer generated randomization into group A or group S or group L or group H, on the day of surgery according to randomization plan. Intravenous (IV) line secured with 18 G canula for males, 20G canula for females in a peripheral vein. Study subjects were premedicated with Midazolam 0.05 mg/kg body weight, fentanyl 1.5 microgram/kg body weight. Patients preoxygenated with 100% oxygen for three minutes. Patients were induced with propofol 1.5- 2 mg/kg body weight, atracurium 0.5 mg/kg body weight to facilitate tracheal intubation. Laryngoscopy done and trachea intubated using cuffed endotracheal tube (portex), orally. Tube size of 7.0 mm was used in females and 8.0 mm in males, three minutes after giving atracurium.
For group A endotracheal tube inflated with a syringe, with air as inflating agent and the cuff pressure set at 20 cm of water with a portex cuff inflator. For group S, L and H the amount of air required to attain the set cuff pressure that is, 20 cm of water measured and the same amount of saline, lignocaine 4% and hydrocortisone 2% respectively injected to inflate the cuff. Cuff pressure measured just before deflating the cuff and recorded, Extubation was performed after checking for spontaneous ventilation, ability to follow verbal commands (eye opening, tongue protrusion). Immediately post extubation, patients were assessed for cough, sore throat and hoarseness of voice and subsequently at 6,12 and 24 hours after extubation.
The sore throat, cough and hoarseness of voice was assessed using Kazemi A et al. and Sun-young Park et al. assessment score.9,10
Statistical analysis was expressed as percentages and continuous data was expressed as mean ± standard deviation (SD). The comparison among the groups was done by appropriate statistical test using chi-square test, unpaired ‘t’ test and one way ANOVA test. A ‘ p ’ value of < 0.05 was considered as significant.
Results
In the present study overall 45.5% were males and 54.5% were females with male to female ratio of 1:1.19. However, the comparison between the groups showed equal gender distribution among all the four groups (Table 1). In this study the mean age of the patients in group A, S, L and H were 37.68 ± 12.54, 37.09 ± 13.54, 38.12 ± 13.32 and 38.38 ± 12.26 years respectively. There was no statistical difference between the mean age among all the four groups (Table 2). In the present research 70.5% had ASA I status and 29.5% had ASA II status. We found that there was no statistical difference between the four groups (Table 3).
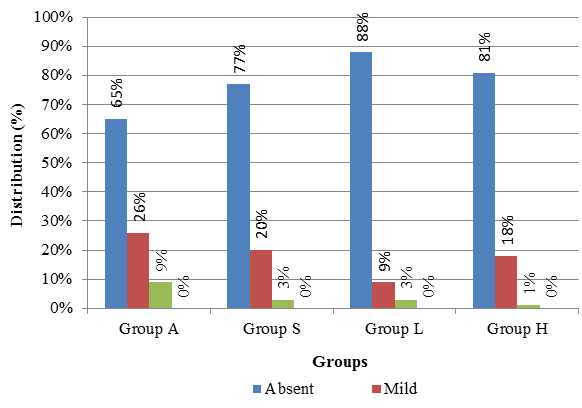
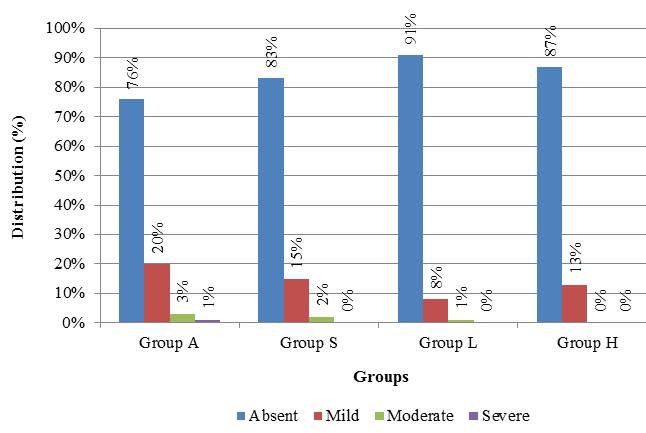
The incidence of sore throat at the beginning was absent in 87% of patients in group L compared to group A, S and H (61%, 76% and 81% ) respectively which is statistically significant (p=0.002 ). At 6 hours, 26% of patients had mild sore throat in group A compared to group L, H and S (9%, 18% and 20%) (p=0.002) (Figure 1), which is again statistically significant. No sore throat was observed in 97% of patients in group L, 96% in group S and 95% in group H at 12 hours which is significantly low when compared to group A 84% (p=0.001) (Figure 2). Lastly at 24 hours 95% of the patients in group A had no sore throat and among 5% it was mild suggesting significantly higher incidence of sore throat in group A compared to other groups (p=0.002).
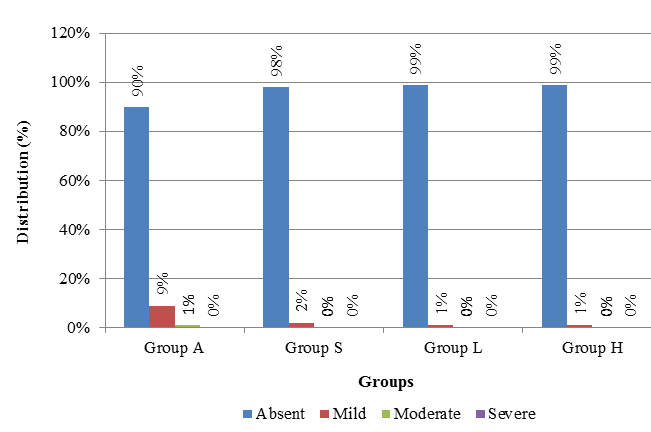
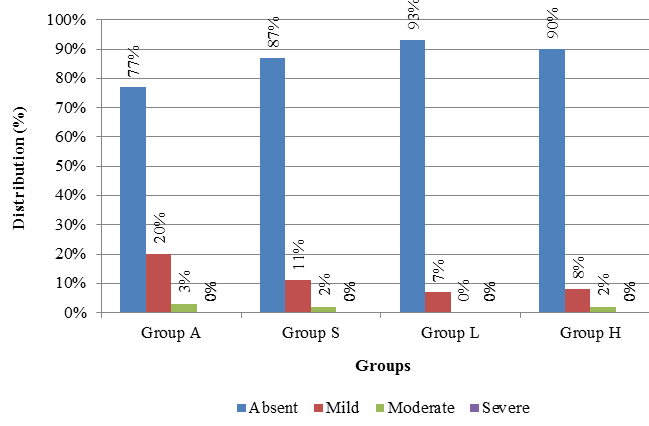
The incidence of cough at the beginning was significantly less in group L (7% patients with mild and 5% with moderate) compared group A, S and H (p=0.005). A t 6 hours the incidence of mild cough was high in group A (20%) compared to group S (15%), H (13%) and L (8%) and severe cough was observed only in group A (1%). However, the result was statistically not significant (p=0.159) (Figure 3), at 12 hours in group A among nine percent patients mild cough and among one percent patients moderate cough was present suggesting significantly higher incidence of cough compared to other groups (p=0.008) (Figure 4) and at 24 hours duration cough was absent in group L and H whereas mild cough was observed in group A among seven percent patients and one percent in group S patients. The result was statistically significant (p=0.001).
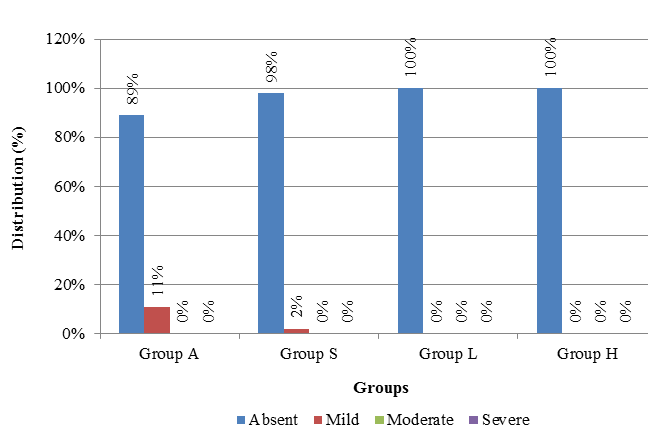
The incidence of hoarseness at the beginning was absent in 90% of the patients in group L compared group H (83%), S (77%) and A (65%). This difference was statistically significant (p=0.005). At 6 hours, the peak incidence of mild hoarseness and moderate hoarseness was 20% and 11% respectively in group A and S compared to (7%) in group L patients which was statistically significant (p=0.036) (Figure 5). At 12 hours 11% patients had mild hoarseness in group A and in group S 2 % patients had mild hoarseness suggesting significantly higher incidence of hoarseness compared to other groups (p<0.0001) (Figure 6) and at 24 hours duration 2% of patients had mild hoarseness in group A wherein no hoarseness was seen in group S, L and H patients. However, the result was statistically not significant (p=0.110).
Table 1
Gender distribution
Table 2
| Groups | Mean Age (Years) | |
| Mean | SD | |
| Group A | 37.68 | 12.54 |
| Group S | 37.09 | 13.54 |
| Group L | 38.12 | 13.32 |
| Group H | 38.38 | 12.26 |
| F=0.1907 | DF=399 | p=0.900 |
Mean age
Table 3
ASA Grades
Graph 5:
Discussion
Endotracheal intubation is usually carried out during surgeries under general an aesthesia to control respiration and protect airways. Airway related problems are commonly seen after extubation. Of this, sore throat and hoarseness were among the most common complications of endotracheal intubation in the first 24 hours after the procedure.11,12 Majority of the patients have little degree of airway injury post extubation. But injuries to trachea are usually minor and reversible. Rarely there will be development of acute or chronic obstruction of the airway because of oedema and granuloma formation. When the obstruction becomes severe, surgical intervention is required. But these injuries can impair normal functioning of the larynx and their protective roles and predispose the patient to pulmonary aspiration also sometimes.13
Laryngotracheal complications like sore throat, hoarseness, cough are seen more with one or all these three complications together.14 Various other factors are co-related with the occurrence of such complications which includes age, gender, seasonal variations, an aesthetic medications and gases, the number of trails for intubation, its duration, area of surgery and application of lidocaine or steroids.11
Long duration of cuff inflation can result in mucosal ischaemia and further airway complications such as coughing. Various pharmacological and non-pharmacological methods have been tried to decrease post extubation airway problems. Lignocaine, an amide local anaesthetic when inserted intracuff acts as a reservoir which being liquid will prevent diffusion of N2O intracuff and also permeates through semipermeable membrane of polyvinyl chloride cuff to provide soothing effect on tracheal mucosa and helps in reducing pressure induced necrosis, cough reflex.
Intracuff hydrocortisone delivers the drug in smaller doses and do not come in direct contact with the patients airway compared with widespread lubrication of the tube with hydrocortisone which may increase the drug dose in contact with the mucosa of the oropharynx, larynx, and trachea, resulting in higher systemic absorption.11
A recent prospective study from Dhaka on 10 0 patients undergoing surgical operations lasting less than 120 minutes with 2% lignocaine (Group L), distilled water (Group W) and air (Group A) as endotracheal cuff inflating agent showed that, 71% of lignocaine group in comparison to 62% distilled water group and 34% air group reported none of the above complications during the entire study period. The study reported an advantage in using lignocaine as an endotracheal tube cuff inflating agent in reducing postoperative sore throat and hoarseness in comparison to distilled water and air.1 Although the results of the present study were similar to these results, the cuff inflating agents used were different.
A double-blind randomized study from Chicago in 1997 used lignocaine as ETT cuff inflating agent among 110 patients with physical status ASA I and II. Patients ETT cuffs were inflated with either air or lignocaine. There was no difference between groups in age, sex or an aesthetic management. The incidence of sore throat was significantly different at the 24-hour evaluation (56% air vs. 35% lignocaine, p = 0.01).15 But no reports on cough or hoarseness of voice was recorded. The observations were similar to the current research stating very less incidence of sore throat in group L at all the four intervals except at 24 hours.
In 1999 a prospective randomized study was conducted in USA comparing the incidence and occurence of sore throat after using lignocaine, saline, or air to inflate the ETT cuff. The study group included female adult patients who are undergoing general an aesthesia for gynaecological procedures with all AS A physical status I, II, or III. The statistical analysis showed that there was no statistical difference in postoperative sore throat among the three groups of lidocaine, saline, and air. But they also assessed the cough and hoarseness of the voice.16 Interestingly, these results were contradictory to our study which can be attributed to different factors such as age, gender and sample selection.
Yet another double-blind, randomized controlled study in cluding 126 intubated patients comparing the incidence and occurence of sore throat and hoarseness following inflation of the ETT cuff using air or saline was done. The overall incidence of sore throat and hoarseness was 18% but there was no statistically significant difference between the groups (air 15.9%, saline 14.5%).17 A very similar results was seen when compared with this present study. Intracuff lignocaine was found to be very effective in decreasing the post - operative sore throat in a study done by Altintas et al.18
Conclusion
The present research concludes that usage of 4% lignocaine as a cuff inflating agent will reduce the incidence of post - operative sore throat, cough and hoarseness when compared to air, normal saline and hydrocortisone. But the few drawbacks of present study w ere mainly the time constraint, exclusion of other variables like deleterious habits history, type of surgery and anaesthetic agent used. Hence, we suggest further research should be conducted considering the drawbacks and inclusion of the variables with larger sample.