- Visibility 176 Views
- Downloads 19 Downloads
- DOI 10.18231/j.ijca.2024.006
-
CrossMark
- Citation
Factors influencing decision-making for the anesthetic technique in molar pregnancy patients for suction curettage: A retrospective study
Introduction
Molar pregnancy, hydatidiform mole or gestational trophoblastic disease, is a gestational trophoblastic disease that results from an abnormal proliferation of trophoblastic tissue in the developing placenta.[1] The incidence of molar pregnancy in the United States and Europe is constant at 1–2 per 1,000 deliveries.[1] In Thailand, the reported incidence of molar pregnancy at Rajavithi Hospital was 2.32 per 1,000 deliveries.[2] Classically, molar pregnancy was diagnosed with dramatic presenting symptoms, including abnormal uterine bleeding, anemia, enlarged uterus for gestational age, theca lutein ovarian cysts, hyperemesis, gestational hypertension, hyperthyroidism, trophoblastic emboli, and acute cardiopulmonary distress.[3], [4] An excessive uterine size occurs in up to half of the patients with complete molar pregnancy and is associated with a higher incidence of these medical complications.[5] Suction curettage is the method of choice for evacuation for molar pregnancy.[6]
Various anesthetic techniques have been reported for the management of suction curettage.[5], [7] General anesthesia is often a preferred anesthetic technique because of the potential for rapid, substantial blood loss, and cardiopulmonary distress during evacuation of the uterus.[5], [8] However, regional anesthesia is reported in the literature as an alternative method due to it offering several advantages. The volatile agents used in general anesthesia cause uterine relaxation, which may increase bleeding; whereas regional anesthesia affects the pulmonary function less and enhances a faster recovery. It also enables an earlier detection of complications, such as thyroid storm or cardiopulmonary distress.[8] Nevertheless, regional anesthesia has limitations in patients with an enlarged uterus due to the tendency of hemodynamic compromise after sympathetic blockade. Besides, this technique is contraindicated in patients with coagulopathy.
The choice of anesthesia should be individualized. However, the factors that affect the decision regarding the anesthetic technique have not been defined yet. Therefore, the aim of the present study was to report the factors influencing the decision-making for the anesthetic technique in molar pregnancy patients who underwent suction curettage at Siriraj Hospital, a tertiary care institute, and the incidence of complications, which may be related to different anesthetic techniques.
Materials and Methods
The study protocol (SIRB Protocol No.1076/2563(IRB3)) was approved by the Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand (approval number Si 082/2021; January 29, 2021). This study comprised a retrospective chart review. The review was conducted among pregnant women diagnosed with molar pregnancy, according to ICD-10: O010 Classical hydatidiform mole, O019 Hydatidiform mole, unspecified, or O011 Incomplete and partial hydatidiform mole, who underwent suction curettage under anesthesia at Siriraj Hospital between January 2007 to September 2021. Medical records with incomplete information or absent of anesthetic records were excluded from the study.
The patient information, including demographic characteristics and clinical characteristics, e.g, gestational age, uterine size, serum beta-hCG levels, associated medical complications, and treatments, was collected. The intraoperative data, such as choice of anesthesia, drugs and doses of anesthetics, vital signs, blood loss, and complications, were included. Postoperative complications were also collected. Hypotension was defined as systolic blood pressure < 80% of preoperative blood pressure or systolic blood pressure < 90 mmHg.[9] Heart rate < 50 beats per minute was defined as bradycardia and heart rate > 100 beats per minute was defined as tachycardia. Desaturation was defined as an oxygen saturation less than 94% for more than 5 minutes.[10] Hyperthyroidism was diagnosed by an abnormal thyroid function test.[11] The primary outcome of the study was to determine the factors that influenced the decision-making for the anesthetic technique in molar pregnancy patients who underwent suction curettage. The secondary outcomes were the incidence of complications related to the different anesthetic techniques.
Statistical analysis
According to the literature review, we could find no reported incidence of the anesthetic technique used for suction curettage, so we calculated the required sample size for our study from a retrospective chart review. We randomly sampled 10 charts and reviewed the incidence of anesthetic technique. It was found that 6 out of 10 patients received general anesthesia, while 4 out of 10 patients received regional anesthesia, accounting for 60% and 40% of the charts accordingly. We presumed that there were 4 factors that influenced the decision-making for the anesthetic technique: uterine size by ultrasound, anemia, beta-hCG level, and hyperthyroidism. The sample size was determined using the “assumption one ten rule” or “10 events per variables”. Here, given 4 factors (variables), the total events required would be 10 multiplied by 4, equaling 40 events. Then, the sample size was computed using a 40% incidence of molar pregnancy patients undergoing suction curettage under regional anesthesia. Given that the required events were 40 events, we needed to utilize a sample size of 40 × 100 / 40 = 100 patients. With 20% in reservation for incomplete medical records, the final sample size was thus determined as needing at least 120 patients.
Statistical analysis was performed using the software program PASW statistics (SPSS) version 17.0 (SPSS Inc, Chicago, IL, USA). Continuous data were expressed as means±standard deviation or medians with interquartile ranges and analyzed by either the unpaired t-test or Mann–Whitney U test. While categorical data were reported as numbers and proportions in percentages and analyzed by the chi-square test. Logistic regression was used to establish the factors influencing the decision-making for the anesthetic technique in the molar pregnancy patients who underwent suction curettage. A p-value < 0.05 was considered statistically significant.
Results
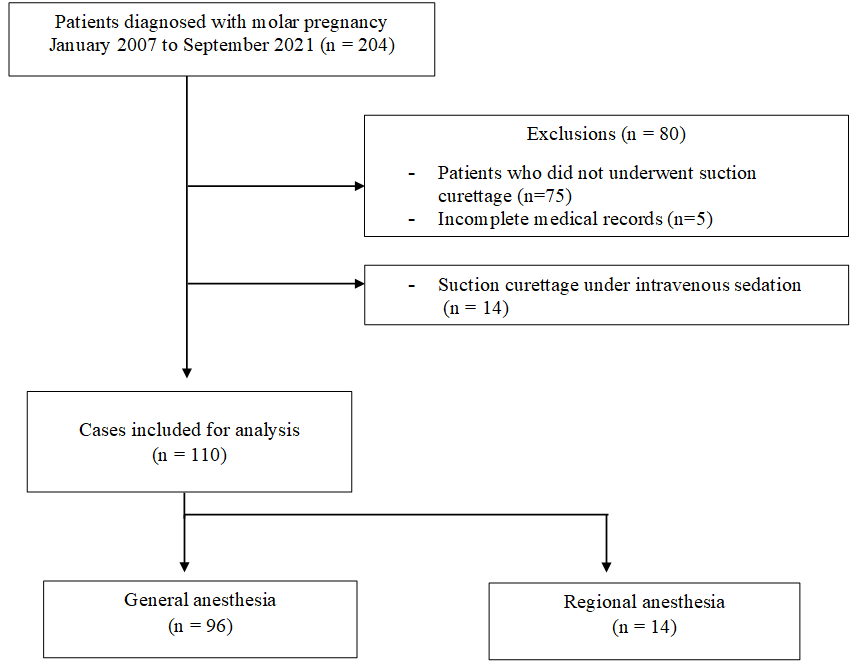
During the 15-year investigated period, 204 charts of patients diagnosed with molar pregnancy were identified and reviewed. Of those, 80 charts of patients who did not undergo suction curettage or who had incomplete medical records were excluded, leaving 124 included cases. In the remaining included cases, general anesthesia was the most commonly applied anesthetic technique, accounting for 77.4% of the molar pregnancy patients who underwent suction curettage, followed by regional anesthesia (11.3%) and intravenous sedation (11.3%). Because deep sedation with total intravenous anesthesia was not a standard anesthetic technique for suction curettage at our institute,[5] this group of patients was not counted for analysis, as shown in [Figure 1]. In this study, spinal anesthesia was only applied as a regional anesthetic technique for the procedure.
There was no difference in demographic characteristics between patients who received general anesthesia and regional anesthesia, as shown in [Table 1]. The patients’clinical characteristics, including uterine size and medical complications associated with molar pregnancy, are listed in [Table 2]. The size of the uterus was measured as a “weeks size” compared with the size expected for a normal pregnant uterus. The average uterine size of patients receiving general anesthesia was significantly larger than for those receiving regional anesthesia (16.2 ± 4.2 weeks compared to 12.0 ± 2.6 weeks). The proportion of patients diagnosed with hyperthyroidism was significantly higher in the general anesthesia group compared to in the regional anesthesia group (69.8% vs. 35.7%, respectively). Regarding the 72 patients with hyperthyroidism, 25 patients (26%) required beta blockers for treatment, and 11 patients (10%) received antithyroid drugs. Serum beta-hCG levels were also significantly higher in the general anesthesia group than in the regional anesthesia group (median 445,785 mIU/ml compared to 185,875 mIU/ml). Hyperemesis gravidarum and gestational hypertension were only detected in the general anesthesia group (26% and 11%, respectively). Reported postoperative serious complications, such as pulmonary edema (4.2%), were confined to the general anesthesia group. All of the patients with preoperative anemia and electrolyte imbalance underwent suction curettage under general anesthesia, but there was no statistical significance.
|
Variable |
General anesthesia (= 96) |
Regional anesthesia (= 14) |
p-value |
|
Age (years) |
29.1 ± 10.2 |
29.8 ± 10.7 |
0.743 |
|
Body mass index (kg/m2) |
22.4 ± 4.3 |
23.6 ± 4.7 |
0.327 |
|
Gestational age (weeks) |
12.3 ± 4.1 |
10.3 ± 3.2 |
0.100 |
|
General anesthesia (= 96) |
Regional anesthesia (= 14) |
P-value |
|
|
Uterine size* (weeks) |
16.2 ± 4.2 |
12.0 ± 2.6 |
<0.001 |
|
Abnormal uterine bleeding |
81 (84.4%) |
11 (78.6%) |
0.698 |
|
Anemia** |
20 (20.8%) |
0 (0.0%) |
0.069 |
|
Hyperthyroidism*** |
67 (69.8%) |
5 (35.7%) |
0.017 |
|
Beta blocker |
25 (26.0%) |
0 (0.0%) |
0.037 |
|
Antithyroid drug |
10 (10.4%) |
1 (7.1%) |
1.000 |
|
Gestational hypertension |
11 (11.5%) |
0 (0.0%) |
0.353 |
|
Theca-lutein cyst |
18 (18.8%) |
1 (7.1%) |
0.457 |
|
Acute cardiopulmonary distress**** |
4 (4.2%) |
0 (0.0%) |
1.000 |
|
Hyperemesis gravidarum***** |
25 (26.0%) |
0 (0.0%) |
0.037 |
|
Electrolyte imbalance |
7 (7.3%) |
0 (0.0%) |
0.592 |
|
Serum beta-hCG levels (mIU/ml) |
445,785 [226798, 836,773] |
185,875 [103192, 397,487] |
0.003 |
Analyzed by logistic regression, as shown in [Table 3], the univariable logistic regression showed that general anesthesia was likely to be used in patients with a larger uterine size, hyperthyroidism, and higher serum beta-hCG levels with odds ratios of 1.49, 4.56, and 1.00 accordingly (p = 0.002, 0.016, and 0.01). Multivariable logistic regression demonstrated that uterine size was only significantly associated with the decision-making for the anesthetic technique after adjusting for hyperthyroidism and the serum beta-hCG levels (adjusted OR 1.35, 95% CI 1.02–1.79, p < 0.05). This result demonstrated that a uterine size ≥ 16 weeks is a predictor for the choice of general anesthesia as the anesthesia technique.
|
Crude odds ratio (95% CI) |
p-value |
Adjusted odds ratio (95% CI) |
p -value |
|
|
Uterine size (per increased size of 1 week) |
1.49 (1.16, 1.91) |
0.002 |
1.35 (1.02, 1.79) |
0.033 |
|
Uterine size ≥ 16 weeks |
11.64 (1.08, 125.72) |
0.043 |
||
|
Hyperthyroidism |
4.56 (1.33, 15.64) |
0.016 |
2.45 (1.02, 1.79) |
0.259 |
|
Serum beta-hCG levels (per increased level of 100,000 mIU/ml) |
1.45 (1.09, 1.91) |
0.010 |
0.99 (0.69, 1.41) |
0.940 |
|
Hyperemesis gravidarum |
N/A |
N/A |
N/A |
N/A |
Intraoperative complications are described in Table 4. The incidence of hypotension was not different among both groups. Only patients under general anesthesia encountered intraoperative uterine atony or massive hemorrhage (17.7% and 7.3%, respectively) but there was no statistical significance. The incidence of intraoperative pulmonary edema was 4.2%, which was observed in the general anesthesia group. Thyroid storm was not observed in any of the patients. Also, none of the patients had anesthesia-related complications, such as pulmonary aspiration, difficult intubation, or a high neuraxial blockade. Postoperative complications were confined to patients receiving general anesthesia, as shown in [Table 5].
|
General anesthesia (n = 96) |
Regional anesthesia (n = 14) |
p-value |
|
|
Hypotension* |
12 (12.5%) |
4 (28.6%) |
0.120 |
|
-Episodes of hypotension (times) |
1.1 ± 0.3 |
1.3 ± 0.5 |
|
|
-Patients required intraoperative vasopressor |
12 (12.5%) |
4 (28.6%) |
|
|
-Intraoperative ephedrine (mg) |
5.5 ± 5.4 |
13.5 ± 7.5 |
|
|
-Intraoperative norepinephrine (mcg) |
5.7 ± 10.7 |
0.0 |
|
|
Tachycardia (HR > 100 bpm) |
30 (31.3%) |
0 (0.0%) |
0.010 |
|
Bradycardia (HR < 50 bpm) |
1 (7.1%) |
1 (7.1%) |
0.239 |
|
Desaturation (SpO2 < 94%) |
1 (7.1%) |
0 (0.0%) |
1.000 |
|
Uterine atony (required at least 2 uterotonic agents) |
17 (17.7%) |
0 (0.0%) |
0.121 |
|
Massive hemorrhage (blood loss > 1,000 ml) |
7 (7.3%) |
0 (0.0%) |
0.592 |
|
Acute pulmonary edema |
4 (4.2%) |
0 (0.0%) |
1.000 |
|
Thyroid storm |
0 (0.0%) |
0 (0.0%) |
N/A |
|
Fluid intake (ml) |
643.3 ± 356.3 |
428.6 ± 267.3 |
0.011 |
|
Intraoperative blood loss (ml) |
414.9 ± 454.0 |
75.0 ± 87.2 |
<0.001 |
|
Packed red cells transfused |
16 (16.7%) |
0 |
0.215 |
|
General anesthesia (n = 96) |
Regional anesthesia (n = 14) |
p-value |
|
|
Tachycardia required treatment |
11 (11.5%) |
0 (0.0%) |
0.353 |
|
Desaturation (SpO2 < 94%) |
2 (2.1%) |
0 (0.0%) |
1.000 |
|
Pulmonary edema (from CXR or required treatment) |
4 (4.2%) |
0 (0.0%) |
1.000 |
|
- ICU admission |
2 (2.1%) |
0 (0.0%) |
1.000 |
|
- Remained intubation |
1 (1.0%) |
0 (0.0%) |
1.000 |
Discussion
This study demonstrated that the most preferable anesthetic technique in molar pregnancy patients undergoing suction curettage is general anesthesia. The key factor influencing the decision-making for the anesthetic technique in molar pregnancy patients who underwent suction curettage was the uterine size. General anesthesia was an anesthetic technique chosen in patients with enlarged uterine size > 16 weeks.
It is important to choose an anesthetic technique based on the patient’s condition, associated medical complications, and disease severity, because each technique has its pros and cons. Regional anesthesia is associated with several benefits compared to general anesthesia. First, it avoids the tocolytic effect of volatile agents, which may reduce the risk of bleeding during surgical procedures.[12] Second, the use of regional anesthesia allows for the earlier detection of complications, such as thyroid storm or cardiopulmonary distress.[12], [13] Additionally, regional anesthesia can also avoid potential complications related to the airway and ventilation.[12], [13] Finally, regional anesthesia provides effective postoperative pain contro.[14] Meanwhile general anesthesia is the recommended anesthetic technique because of the potential for acute intraoperative blood loss, acute pulmonary edema, and cardiovascular instability.[5]
Standard anesthetic techniques for suction curettage that have been described are both general anesthesia and regional anesthesia.[5] General anesthesia is mostly preferred in the previous literature,[15] although regional anesthesia is reported in some specific cases.[7], [8] According to Swaminathan S, suction curettage can be safely done in molar pregnancy patients with hyperthyroidism under spinal anesthesia after the optimization of thyrotoxicosis. [8] Nevertheless, there is a paucity of publications on the impact of the anesthetic technique on suction curettage.
Univariate analysis in the present study showed that patients with a larger uterine size, hyperthyroidism, and higher serum beta-hCG levels are more likely to receive general anesthesia. An enlarged uterine size is also associated with high serum beta-hCG levels. About 25% of patients with uterine sizes greater than that expected at 14 to 16 weeks' gestation experience medical issues, including hyperemesis gravidarum, gestational hypertension, and hyperthyroidism.[5] Higher serum beta-hCG levels stimulate the thyroid hormone and can result in hyperthyroidism.[16] Even though hyperthyroidism, diagnosed with a high thyroid hormone level, is presented in approximately 25%–64% of molar pregnancies, clinical hyperthyroidism was reported in only 5% of cases in one study.[17] Serum beta-hCG levels greater than 200,000 mIU/ml are related to clinical hyperthyroidism.[18] Hyperemesis gravidarum is also associated with high serum beta-hCG levels. A previous study reported the incidence of hyperemesis gravidarum in as many as 26% of molar pregnancies,[19] which was a similar result to our study. Hyperthyroidism may also further aggravate hyperemesis gravidarum.[20] An excessive uterine size has been linked to an increased incidence of medical complications.[5] Multivariate analysis in the present study demonstrated that the uterine size is the only factor that impacts the decision about the anesthetic technique.
According to the present study, patients receiving general anesthesia received more fluid intake and had more operative blood loss intra-operatively. From the literature review, patients with a uterine size greater than 16 weeks are at risk of substantial blood loss.[7] Furthermore, patients in such cases are at a higher risk of experiencing cardiopulmonary complications.[5], [7] This study reported intraoperative complications and postoperative complications, such as massive hemorrhage and pulmonary edema, which were confined within the general anesthesia group, but with no statistical significance.
A higher risk of acute cardiopulmonary distress occurs in patients with uterine enlargement greater than 16 weeks size.[7], [21], [22] Our study reported 4 of 110 patients who suffered from acute pulmonary edema. Trophoblastic embolization might have occurred after uterine evacuation, resulting in acute cardiopulmonary distress. Thyrotoxicosis may induce high-output cardiac failure and acute pulmonary edema.[15], [21] Iatrogenic fluid overload is another presumable cause of perioperative acute pulmonary edema.[22] Therefore, cautiousness in fluid management, especially in high-risk patients, including patients with hyperthyroidism and an enlarged uterine size, is recommended.
Deep sedation is not considered a standard anesthetic technique for suction curettage because of the risks of regurgitation and pulmonary aspiration during the procedure. Gravid uterus can displace the intra-abdominal esophagus into the thorax, causing a reduction of the lower esophageal sphincter tone.[23] Moreover, progesterone-induced decreased gastric motility was reported to result in an increased risk of aspiration in pregnant women.[23] Therefore, we excluded patients receiving intravenous deep sedation.
This study prompts anesthesiologists to consider general anesthesia in molar pregnancy patients with a uterine size greater than 16 weeks and to be aware that patients with a larger uterine size may be associated with more severe medical complications or intraoperative complications.
Our study has some limitations to note. First, the study was a retrospective chart review; thereby, some data regarding the details of the patients’ conditions, such as the clinical presentation before undergoing surgery, might be incomplete. Second, some factors that had an impact on the decision-making for the anesthetic technique that depended on the individual anesthesiologist might be missing. However, this study has the potential to serve as a valuable database for future reference and utilization.
Conclusion
The only factor that has an influence on the decision-making for the anesthetic technique is uterine size. General anesthesia is preferred in patients with a uterine size ≥ 16 weeks. Patients with an enlarged uterine size are significantly associated with higher beta-hCG levels, resulting in more severe medical complications, such as hyperthyroidism and hyperemesis gravidarum.
Source of Funding
This research project was supported by Siriraj Research Fund, Grant number (IO) R016431044, Faculty of Medicine Siriraj Hospital Mahidol University.
Potential Conflicts of Interest
The authors declare they have no conflicts of interest.
References
- FG Cunningham, KJ Leveno, SL Bloom, JC Hauth, DJ Rouse, CY Spong, FG Cunningham, KJ Leveno, SL Bloom, CL Spong, JS Dashe, BL Hoffman. Gestational Trophoblastic Disease. Williams Obstetrics 2014. [Google Scholar]
- M Yanaranop, C Potikul, S Tuipae. A 10-year clinical experience of gestational trophoblastic disease at Rajavithi hospital. J Med Assoc Thai 2001. [Google Scholar]
- A Braga, V Moraes, I Maestá, JA Júnior, JD Rezende-Filho, K Elias. Changing trends in the clinical presentation and management of complete hydatidiform mole among Brazilian women. Int J Gynecol Cancer 2016. [Google Scholar]
- JT Soper. Gestational Trophoblastic Disease: Current Evaluation and Management. Obstet Gynecol 2021. [Google Scholar]
- KW Arendt, ME Long, DH Chestnut, CA Wong, LC Tsen, WD NganKee, Y Beilin, JM Mhyre. Problems of early pregnancy. Chestnut’s obstetric anesthesia: principles and practice 2020. [Google Scholar]
- LR Lurain. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol 2010. [Google Scholar]
- D Celeski, J Micho, L Walters. Anesthetic implications of a partial molar pregnancy and associated complications. AANA J 2001. [Google Scholar]
- S Swaminathan, RA James, R Chandran, R Joshi. Anaesthetic implications of severe hyperthyroidism secondary to molar pregnancy: A case report and review of literature. Anesth Essays Res 2017. [Google Scholar]
- K Kouz, P Hoppe, L Briesenick, B Saugel. Intraoperative hypotension: Pathophysiology, clinical relevance, and therapeutic approaches. Indian J Anaesth 2020. [Google Scholar]
- BR O’Driscoll, LS Howard, AG Davison. TS guideline for emergency oxygen use in adult patients. Thorax 2008. [Google Scholar]
- S Matsumoto, C Shingu, S Hidaka, K Goto, S Hagiwara, H Iwasaka. Anesthetic management of a patient with hyperthyroidism due to hydatidiform mole. J Anesth 2009. [Google Scholar]
- C Ryalino, T Ariasa, G Budiarta, TA Senapathi. Regional anesthesia in molar pregnancy with thyrotoxicosis in a remote hospital. Bali J Anesthesiol 2017. [Google Scholar]
- T Girma. Anesthesia management of known asthmatic patient with gestational trophoblastic disease in resource limited area: Case report. Int J Surg Open 2021. [Google Scholar] [Crossref]
- BF Rochman, MP Adhi, I Nuryawan. Perioperative anesthetic management of molar pregnancy patients with hyperthyroidism and COVID-19 underwent suction curettage. Majalah Anestesia Crit Care 2021. [Google Scholar]
- MS Kurdi, RS Deva. Post-evacuation cardiopulmonary distress in a case of molar pregnancy. Anaesth Pain Intensive Care 2014. [Google Scholar]
- N Anisodowleh, K Farahnaz, J Nasrin, H Maryam, B Elaheh. Thyroid hormone levels and its relationship with human chorionic gonadotropin in patients with hydatidiform mole. Open J Obstet Gynecol 2016. [Google Scholar]
- C Blick, KE Schreyer. Gestational Trophoblastic Disease-induced Thyroid Storm. Clin Pract Cases Emerg Med 2019. [Google Scholar]
- JM Hershman. Physiological and pathological aspects of the effect of human chorionic gonadotropin on the thyroid. Best Pract Res Clin Endocrinol Metab 2004. [Google Scholar]
- MM Glick, EL Dick. Molar pregnancy presenting with hyperemesis gravidarum. J Am Osteopath Assoc 1999. [Google Scholar]
- NS Panesar, CY Li, MS Rogers. Are thyroid hormones or hCG responsible for hyperemesis gravidarum? A matched paired study in pregnant Chinese women. Acta Obstet Gynecol Scand 2001. [Google Scholar]
- S Bhatia, U Naithani, YK Chhetty, N Prasad, SR Jagtap, I Agrawal. Acute pulmonary edema after evacuation of molar pregnancy. Anaesth Pain Intensive Care 2011. [Google Scholar]
- H Abbasi, A Behforouz. Acute Pulmonary Edema After Large Molar Pregnancy Uterine Evacuation. Acta Med Iran 2020. [Google Scholar]
- RM Kacmar, R Gaiser, DH Chestnut, CA Wong, LC Tsen, WD Ngankee, Y Beilin, JM Beilin. Physiologic changes of pregnancy. Chestnut’s obstetric anesthesia: principles and practice 2020. [Google Scholar]
